This article has been
cited by other articles in ScienceCentral.
Abstract
Myofascial pain syndrome (MPS) is one of the common musculoskeletal conditions of the shoulder which may develop sensory-motor and autonomic dysfunctions at the various level of the neuromuscular system. The pain and dysfunction caused by MPS were primarily treated with physical therapy and pharmacological agents in order to achieve painfree movements. However, in recent years intramuscular electrical stimulation (IMES) with conventional electrode placement was used by researchers to maximise therapeutic values. But, in this study an inverse electrode placement was used to deliver electrical impulses intramuscularly to achieve neuro-modulation at the various level of the nervous system. Nine patients with MPS were treated with intramuscular electrode stimulation using inversely placed electrodes for a period of three weeks. All nine subjects recovered from their shoulder pain and disability within the few weeks of intervention. So, this inverse electrode placement may be more appropriate for chronic pain management.
Go to :

Keywords: Dry needling, Inverse electrode placements, Intramuscular electrical stimulation, Myofascial pain syndrome, Myofascial trigger points, Surface electrical stimulation
INTRODUCTION
Travel and Simmons have described the myofascial trigger point (MTrP) as a hypersensitive knot within the cytoskeleton of skeletal muscle [
1]. According to Bron et al. [
2] the shoulder musculature is very prone to developing MTrPs due to various non-traumatic shoulder pathologies. The presence of MTrPs may gradually reduce the muscle's function and also manifest spontaneous pain, spot tenderness, altered movement pattern, etc. The untreated MTrPs may sensitise the peripheral, segmental, and central neurons that may develop chronic symptoms including muscle weakness, diffused or referred pain, radiculopathic pain, allodynia, trophoedema, etc [
34].
For many decades, physical therapy and pharmacological agents have been primarily used as a general approach to treat MPS. But, dry needling (DN) and intramuscular electrical stimulation (IMES) methods have shown interesting evidences in the recent past [
56]. There are several research findings supporting the therapeutic benefits of electrical impulses of various pulse durations and frequencies in pain relief and improvement of function [
78]. A few studies on shoulder and back pain have stated that the IMES with dry needle has been effective in achieving therapeutic effects [
910]. However, there is no uniform electrode placement followed among these studies and no study has documented the use of inverse electrode placement. Inverse electrode placement is defined as a new method of electrode placement in which cathode pole will be placed over the spinal level and anode pole over the distal parts of limbs. This method of stimulation initiates electrical impulses from the spinal level and helps impulses to flow bi-directionally towards the peripheral and central direction. Theoretically, the multilevel electrical stimulation effects can induce widespread pain inhibition, segmental relaxation and tissue healing, etc. So, this method may be an appropriate option for neuro-modulation of sensory-motor and autonomic neurons at the level of MTrPs, the spinal neuronal pool, and the central level. To support this hypothetical model of electrode placement we have treated nine patients with MPS of the shoulder with IMES.
Go to :

CASE REPORT
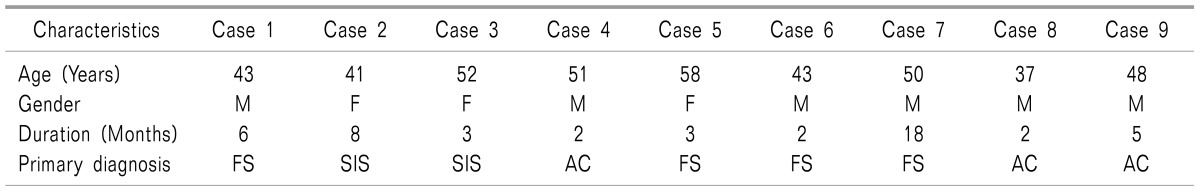
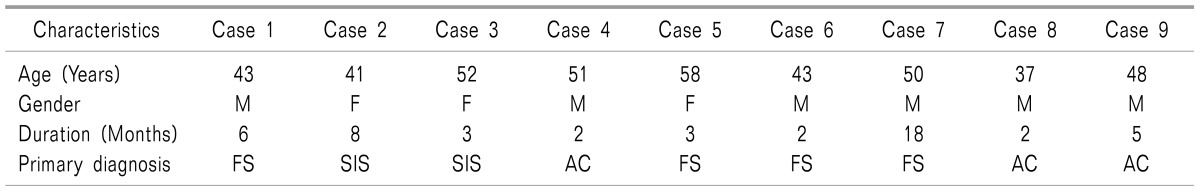
There were nine patients with non-traumatic shoulder dysfunction aged between 37 and 60 years referred to the physical therapy department. All patients had complaints of shoulder pain and difficulty in performing upper limb functions over a period between two and eighteen months (
Table 1). The preliminary medical report has shown that all patients were not suffering from coaglulopathy, rheumatoid arthritis, rotator cuff tear, or other major systemic illnesses. The cervical radiographs of all the patients have not shown any indication of intervertebral disc pathology and osteophytes formation. However, physical examination has revealed the clinical signs of MTrPs, especially within the upper trapezius, deltoid, infraspinatus, and rhomboid muscle of the shoulder girdle [
11]. Five patients had demonstrated shoulder asymmetry which suggest an altered movement pattern due to abnormal plastic changes over the neuromuscular system. The taut bands in the upper trapezius and anterior deltoid were identified by manual palpation which also elicited spot tenderness and local twitch responses [
311]. The diffuse pain in five patients showed evidence of the sensitisation of pain receptors by chemical mediators around the MTrPs [
12]. Manual pressure over the cervical spine of all the patients elicited an excessive sympathetic response and three cases reported radiating pain down the lower arm. This may be caused by segmental sensitisation of the spinal roots due to sustained loading over the facet joints [
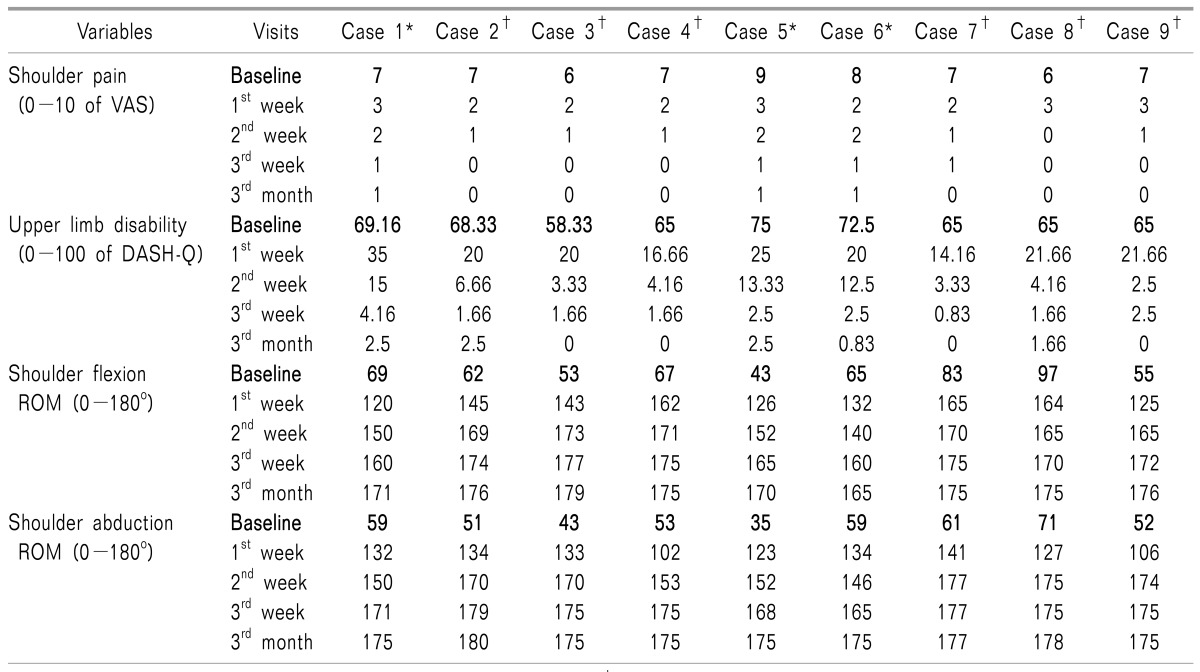
14]. Baseline visual analog scale (VAS) scores between 6 and 9, and upper limb disability (DASH) scores between 58.33 and 75 were documented. The goniometric measurement of shoulder flexion and abduction range of motion was also reduced in all patients to below 100 degrees (
Table 2). Based on the nature of the clinical manifestations we came to the conclusion that there was evidence for chronic stage MPS.
Table 1
Characteristics of Nine Patients with Myofascial Pain Syndrome Due to Non-traumatic Shoulder Dysfunction
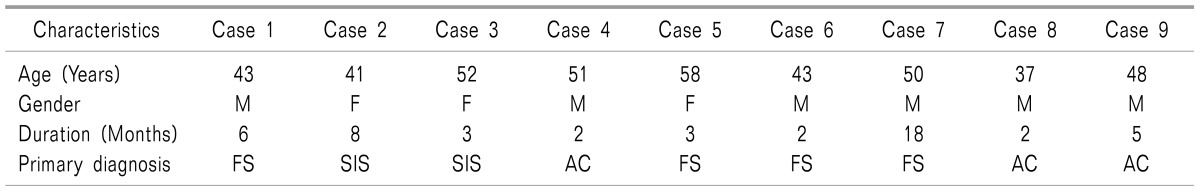

Table 2
Description of Baseline and Post Intervention Shoulder Pain, Upper Limb Disability, and Shoulder Flexion and Abduction Range of Motion Scores among Nine Patients

Procedure for IMES: With the patient lying in a prone position the area of skin over the cervical region and the MTrPs of the shoulder muscles were cleaned with Sterimax® antiseptic liquid. A straight line was drawn from the tip of the C
7 spinous process to the posterior arch of the C
1 vertebra along the supraspinous line. The needle insertion site for the paraspinal muscles of the C
7 spine was marked just 1.5-2 cm lateral to the midpoint of the C
7 spinous process prominence. The needle insertion sites for the spinal muscles between the 6
th and 3
rd cervical spine were marked just 1 cm lateral to the corresponding tip of the spinous process. A sterilised acupuncture needle (0.25 mm thick × 25 & 40 mm length, Cloud & Dragon®, Jiangsu, China) was inserted into the paraspinal muscles of the C7 spine through the marked site at 45°-90° angles. And, from the sixth to third cervical spine the needle was inserted into the spinal muscles just perpendicular to the skin from the marked site (
Fig. 1) till it reaches the laminar side myofascia of the spinal muscles without touching the bony obstruction [
13]. Similarly, the dry needles were inserted into the myofascial trigger point of the upper trapezius, deltoid, infraspinatus and rhomboid muscles from the midpoint of muscle belly [
14]. Thereafter, the spinal needles were connected to the cathode lead and the needles over the shoulder muscles were connected to the anode lead by using a crocodile clip connector. Then, the patients were informed about the electrically induced muscle twitches over the needle insertion areas. The low frequency (5 Hz) electrical impulses from the 12V (500 mA) electrical stimulator source (Acu-TENS, Technomed Electronics) were connected to the needle electrodes. A tolerable intensity was applied to the muscles for 5-10 minutes and minimal muscle twitches were observed throughout the treatment session. Each level was stimulated twice a week with a 48-72 hour interval between the two sessions. Among the nine patients, 3 cases received IMES for three weeks and the remaining six patients have received it for two weeks. All patients were instructed to perform active free shoulder exercises once optimal muscle relaxation was achieved especially after one week of IMES.
 | Fig. 1Superior view of dry needle electrodes insertion over 3rd, 4th, 5th, 6th & 7th cervical levels.
|
Go to :

DISCUSSION
This study was conducted to evaluate the effects of IMES using inversely placed electrodes on chronic MPS in the shoulder. In contemporary practice, the active electrode (cathode) is placed on the peripheral target region and the reference electrode (anode) placed over the spinal level [
6910]. This conventional electrode placement (non-inverse) usually generates electrically induced muscle contraction of the peripheral muscles rather than the spinal musculatures. But in cases of chronic MPS the spinal and cortical neuronal involvements were prominent compared to the peripheral. Based on this reason the electrode placement method was changed to the reverse order to achieve bidirectional flow of electrical impulses from the spinal neurons to the central neurons and peripheral musculatures. Thus, to evaluate this inverse electrode placement scientifically we selected nine patients with MPS of the shoulder due to various non-traumatic shoulder pathologies.
The baseline data of the nine patients clearly stated that there was a reduction of upper limb function due to shoulder pain and movement deterioration. Interestingly, the shoulder pain and dysfunction were noticed with slight variation even though the duration of the conditions varied among the nine patients. These baseline scores have shown the evidence for the chronic nature of the shoulder dysfunction due to MPS (
Table 2).
In the comparison between the baseline and 1
st week post intervention, VAS and DASH scores showed larger variation. Similar improvements were also noted for shoulder flexion and abduction range of motion even after one week of IMES (
Table 2). In fact, some of the patients recovered moderately from pain and movement dysfunction within two sessions of IMES. This immediate reduction of pain and disability suggests that an active needle electrode placed over the spinal level may effectively modulate neurons at the various levels of the central and peripheral nervous system.
The comparison of the second week's post intervention outcome scores over baseline scores has also clearly showed maximum recovery from pain and movement dysfunction in all patients. Therefore, only very minimal differences were noted among the second and third week post intervention scores and 3rd month follow-up measurements (
Table 2). These results are evidence that even two weeks of IMES with inversely placed electrodes may be sufficient to achieve maximum therapeutic benefits. The post IMES examination also has not shown any adverse effects from dry needle procedure like external bleeding, excessive soreness etc.
In contrast, the non-inverse electrode placement was used in the few studies of IMES in the recent past. Particularly, a case study of Rainey [
10] has demonstrated the benefits of IMES on low back myofascial pain syndrome. The authors of another study on thoracic spine dysfunction have placed both active and reference electrodes over the spinal level to deliver the electrical impulses intramuscularly [
15]. So, further research is required to compare the effects of IMES with inversely placed electrodes with conventional placement methods.
Based on the outcomes in these nine patients we conclude that inverse electrode placement can be an appropriate method for IMES in cases of chronic pain management. The evidence from this study may be helpful in formulating a larger sample randomised control trial to compare the inverse electrode placement with other electrode placement methods. If researchers intend to evaluate the additional benefits of IMES, further study can be conducted for comparing the dry needle technique with and without IMES.
Go to :