Abstract
Background
The study aimed to determine if ultrasonography of masseter can be used to evaluate the outcome of transcutaneous electrical nerve stimulation (TENS) in subjects with temporomandibular disorders (TMDs) such as myositis and myofascial pain.
Methods
Fifteen TMD subjects with myofascial pain/myositis who satisfied the RDC/McNeil criteria were included in the study. All the subjects were administered TENS therapy for a period of 6 days (30 minutes per session). The mouth opening (in millimeters) and severity of pain (visual analogue scale score) and ultrasonographic thickness of the masseter (in millimeters) in the region of trigger/tender areas was assessed in all the subjects both prior and post TENS therapy. A comparison of the pre-treatment and post-treatment values of the VAS score, mouth opening and masseter thickness was done with the help of a t-test.
Go to : 
Temporomandibular joint disorder (TMD) is a generic term used to describe a group of disorders or diseases affecting masticatory muscles, the temporomandibular joint (TMJ), and associated structures [1]. The most common muscle disorder in patients complaining of temporomandibular pain and dysfunction is myofascial pain [2]. Myofascial pain may be associated with a thickened masseter muscle; however, the mechanism of thickening has not been well described [3]. Myositis refers to inflammation of muscle tissue and has been divided into delayed onset and generalized myositis by McNeill [4].
A number of modalities including occlusal adjustments, pharmacological therapy, and physical therapy have been advocated in the management of masticatory muscle pain. Physical therapies (such as mouth opening exercises, occlusal splints, acupuncture, ultrasound, short-wave diathermy, and low-level laser therapy) aim at muscle relaxation and increases in the blood and lymphatic circulation to re-establish the muscle physiology. Transcutaneous electrical nerve stimulation (TENS) has been widely used as a physical therapeutic modality [5]. TENS is a safe, noninvasive, effective, and rapid method of providing analgesia in which potential adverse reactions associated with other methods of pain control are eliminated [6].
The therapeutic efficacy of TENS has been evaluated with the help of clinical parameters such as the visual analogue scale (VAS) score, extent of mouth opening, and alteration of joint sounds, among others [678910]. However, to the best of our knowledge, imaging modalities in the form of ultrasonography have not been used to determine whether TENS therapy can alter the thickness of the masseter in patients with TMD pathologies. Ultrasonographic imaging is considered a "real-time", reliable, simple, inexpensive, and safe imaging modality [11]. Ultrasonography can noninvasively depict the morphology of muscles situated superficial to the bone structures in the head and neck, such as masticatory muscles [12].
With the above background, the present study aimed to determine whether ultrasonography of the masseter can be used to evaluate the efficacy of TENS therapy in subjects with TMDs such as myositis and myofascial pain. The efficacy of TENS was also evaluated with the help of clinical parameters such as the VAS score and improvement in mouth opening.
Go to : 
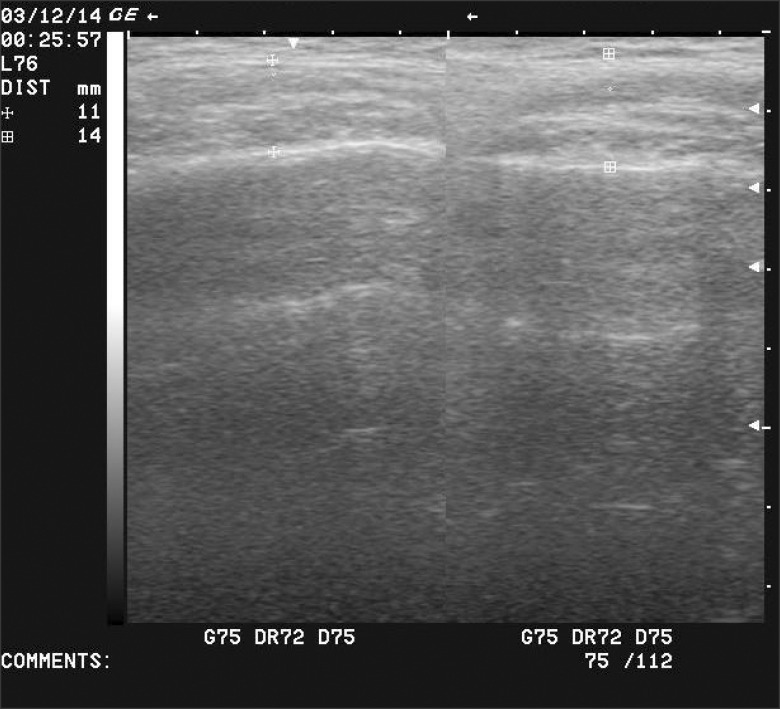
Fifteen TMD subjects with myofascial pain/myositis who satisfied the Research Diagnostic Criteria (RDC)/McNeill criteria were included in the study [2]. The sample size was calculated using the following formula:
Where, n = sample size
S = Combined standard deviation between pre-treatment and post-treatment values
d = Clinically acceptable error between pre-treatment and post-treatment values
Zα = Z-value for α level, Zβ = Z-value for β level
α = False positive error, β = False negative error
All the values used for the above formula were obtained based on the results of a similar study by Ariji et al. [5].
Subjects with acute dental conditions, more than one missing tooth, or removable prostheses, and those with a history of craniofacial neuralgias and prior treatment for muscle pain were excluded from the study. Written consent was obtained from all study subjects and ethical clearance was obtained from the Institutional Review Board prior to conducting the study.
The relevant history of the subjects was recorded. The severity of pain was assessed with the help of the VAS as follows: a line measuring 10 cm was drawn, and the beginning of the line was marked as 0 and the end of the line was marked as 10. It was explained to each patient that "0" represents "no pain" and 10 represents "pain as bad as it could be." The patient was then asked to mark a point along that line that best represented his or her pain, and the score was measured from the "no pain" end of the scale. The interincisal distance was also measured in all subjects with the help of a divider and a scale.
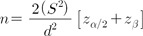
These measurements were followed by ultrasonographic evaluation of the masseter with the help of an ultrasound machine, (2D, LOGIQ 100 PRO, GE Medical Systems, Milwaukee, WI, USA) equipped with a wide band-width linear active matrix transducer with a frequency of 7.5 MHz (Model 2274907, serial 168 WPS, Wipro GE Medical Systems Ltd., Bangalore, India). For ultrasonographic evaluation, the subject was positioned in a semi-reclined position with the head turned to the side to be examined (Fig. 1). Ultrasonographic measurement was performed in a resting position. A water-based gel was applied to the transducer and it was placed transversely perpendicular to the long axis of the muscle in the region of the trigger/tender points. Special care was taken to avoid excess pressure. The distance between the outer fascia of the muscle and the lateral surface of the mandibular ramus was measured to assess the thickness of the muscle (Fig. 2). The measurements were performed on the screen during scanning by freezing the ideal image. The thickness of the masseter muscle was assessed on both sides objectively (in mm) with the help of a measuring tool provided in the software of the ultrasound machine.
Following ultrasonographic examination, the subjects were administered TENS therapy for a period of six days. Each therapeutic session lasted for approximately 30 min. TENS equipment (Indian Medical Systems Electrocare Technologies (P) Ltd., Chennai, India) with a frequency ranging from 1-60 Hz and amplitude ranging from 1-10 µA was utilized. The frequency of the electric current used for the subjects in the present study ranged from 10 to 40 Hz and the amplitude ranged from 1 to 5 µA.
Following TENS therapy, the severity of the pain, maximum mouth opening, and muscle thickness were assessed. The examiner was blinded to the values of masseter muscle thickness prior to TENS therapy.
The pre- and post-treatment values of VAS scores, extent of mouth opening, and muscle thickness were compared with the help of the t-test.
Go to : 
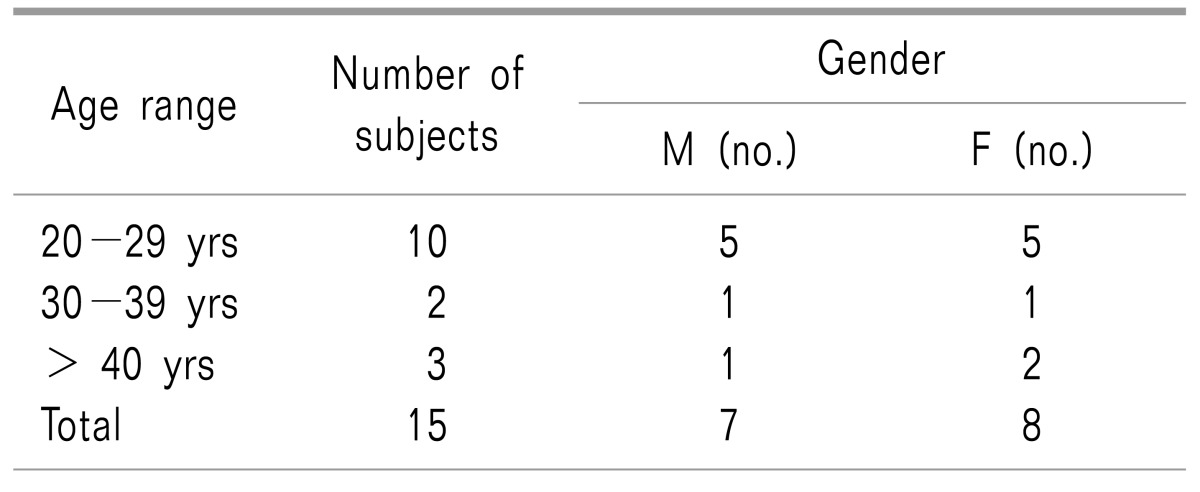
Of the 15 TMD subjects included in the study, six subjects were diagnosed with myositis, five subjects with anterior disc displacement and myositis/myofascial pain, three with arthralgia and myositis/myofascial pain, and one subject with myofascial pain. There were a total of seven males and eight females in the study. The ages of the subjects ranged from 20 to 65 years. Most of the subjects (10/15, 66.67%) belonged to the age group of 20 to 29 years, followed by three subjects (20%) who were 40 years of age or older and two subjects (13.33%) who were found in the age group of 30 to 39 years (Table 1).
The most common predisposing factor for TMDs among the study subjects was stress, noted in eight subjects (53.33%), followed by trauma and bruxism, noted in three subjects (20%) each. Two subjects (13.33%) described a history of postural abnormality, and one had occlusal factors contributing to TMD. The mouth opening of subjects ranged from 25 to 46 mm.
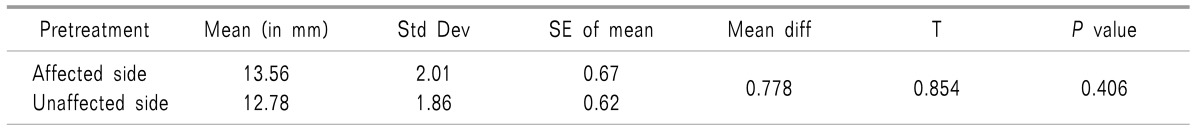
In subjects with unilateral involvement, the thickness of the masseter on the affected and unaffected sides ranged from 11 to 17 mm and 10 to 15 mm, respectively. The average thickness of the masseter on the affected side (13.56 + 2.01 mm) was greater than that on the unaffected side (12.78 + 1.86 mm), although this difference was not statistically significant (P = 0.406) (Table 2).
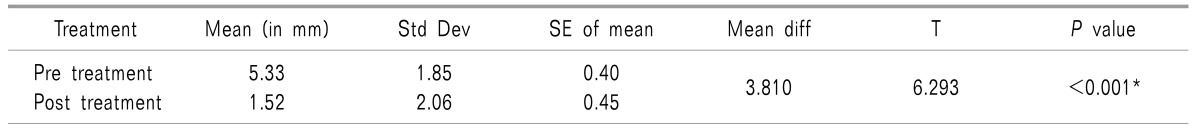
The mean VAS score post-TENS therapy in all of the study subjects was lower (1.52 + 2.06) than the score noted prior to TENS therapy (5.33 + 1.85) (Table 3). This finding was noted to be statistically significant (P < 0.001). There was a 74.19% decrease in VAS scores.
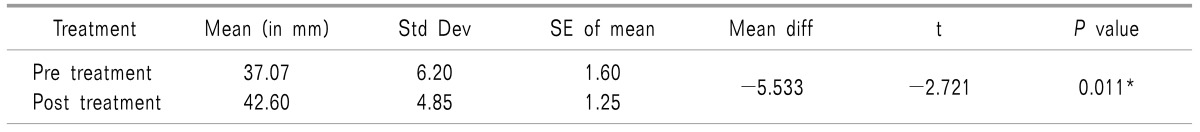
The mean mouth opening post-TENS therapy in all of the study subjects was greater (42.60 + 4.85) than the score noted prior to TENS therapy (37.07 + 6.20) (Table 4). This finding was observed to be statistically significant (t-test, P = 0.011). There was a 19.46% increase in mouth opening.
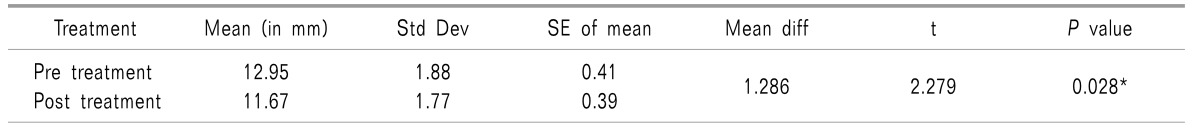
The mean masseter muscle thickness post-TENS therapy in all of the study subjects was decreased (11.67 + 1.77) compared to the thickness noted prior to TENS therapy (12.95 + 1.88) (Table 5). This finding was statistically significant (t-test, P < 0.028). There was a 9.64% decrease in the thickness of the masseter.
Go to : 
TENS is widely used to relieve acute and chronic pain and in various conditions such as back pain, neck pain, phantom limb pain, and extremity pain, among others, but there have been few studies on its use for the relief of orofacial pain [6]. TENS therapy works on several interrelated theories. The first theory suggests that TENS stimulates the thick, myelinated, sensory fibers (A-fibers), which in turn blocks the impulses of thin pain-modulating fibers (C-fibers) and closes the gate to pain signals at the level of their entry into the spinal cord [10]. Another theory suggests that TENS stimulates the endogenous release of morphine-like substances that have analgesic properties. A third mechanism of action is related to the ability of TENS to cause mild, rhythmic muscle contractions, which increases the local circulation of blood and lymph. This reduces interstitial edema and the accumulation of noxious tissue metabolites [10].
Most of the subjects in the present study were in the age group of 20 to 40 years. This is in accordance with the observations of several other studies, in which TMDs have been found to occur in the second to fourth decades of life [6]. The lower prevalence of TMD signs and symptoms in older age groups supports the probability that a significant portion of TMDs are self-limiting [13].
In the present study, a definite gender predilection was not evident. Similar findings have been noted in another study. However a female predominance has been reported in most of the previous studies [6]. This can be attributed to the sex hormones that influence pain sensitivity; the pain threshold and pain tolerance in women can vary with the stage of the menstrual cycle [2].
The VAS is considered an accurate and reliable scale to quantify pain [1]. In the present study, the VAS was used to measure the intensity of pain, and palpation of the masseter muscle was performed to identify the presence of pain. This method of evaluation of muscle pain was recommended by Dupont in the year 1999 [3]. In the present study, a statistically significant decrease in VAS scores following TENS therapy was evident and a considerable reduction (74.19%) in pain was noted. Most previous studies have reported an approximate 57% reduction in pain following TENS therapy in patients with myogenic TMDs [614]. However, one particular study reported a much higher rate of pain reduction (95%) [15].
Further, it was reported in one study that 63.6% of patients with joint and muscle pain were completely relieved of pain after TENS therapy, whereas another study reported that 23.3% were pain-free following TENS [14]. In the present study, 40% of the study subjects were pain-free after TENS therapy. This variation in the percentage of pain reduction and pain-free subjects may be attributed to the fact that pain is a subjective symptom and multifactorial in nature. Pain is an extremely personal experience. Patients feeling a little pain can suffer a lot, while others with significant pain can suffer less [10]. The evaluation of pain relies on the subjective judgment of the patient, because "objective pain" does not exist.
Studies have reported an improvement in the range of mandibular movements including the interincisal distance in patients with TMDs after TENS therapy. In the present study, a significant increase in mouth opening was noted. An increase of 19.46% was observed in the present study, which is higher than that observed in previous studies (5.3% to 13%) [6]. It was also noted in the present study that the percentage increase in mouth opening in subjects with bilateral involvement was more than that in subjects with unilateral involvement. This could be attributed to the fact that in subjects with unilateral involvement, mouth opening was not as restricted compared to subjects with bilateral involvement, hence a greater increase in mouth opening cannot be expected in these subjects.
TMDs such as myofascial pain/myositis are associated with a thickened masseter muscle [11]. A study investigated the ultrasonographic features of inflammatory myopathies (myofascial pain/myositis) at various sites with reference to histological findings and confirmed that edematous muscle was thicker than nonedematous muscle [13]. TENS probably reduces edema, thereby decreasing the thickness of the masseter muscle. This may lead to decreased muscle force and thus, decreased pain.
A study employed occlusal splint therapy in the management of TMD subjects, and a significant reduction in the muscle thickness (mean reduction of 0.93 mm) was noted following splint therapy [11]. In another study, robotic massage treatment resulted in a significant reduction in the muscle thickness in TMD subjects. In the present study, there was a significant reduction in muscle thickness post-TENS, and a mean reduction of 1.26 mm was found [5]. The results of the present study are in accordance with the above-mentioned studies. It may be inferred that TENS therapy is as effective as occlusal splint and massage therapy in reducing masseter muscle thickness.
As previously mentioned, myofascial pain is associated with an edematous change in the muscle which in turn results in increased thickness of the involved muscle. Following TENS therapy, a reduction in the thickness of the muscle is expected as TENS therapy has a role in reducing interstitial edema. This can be appreciated by ultrasonography, whereas clinical methods such as VAS scores and mouth opening do not reflect the reversal of the pathological changes within the muscle. Furthermore, these clinical methods are more reliant on the patient's response. Hence, ultrasonography can be considered as an objective and standardized method to assess the outcome of TENS.
In the present study, a significant improvement in mouth opening and reduction in pain were noted following TENS therapy. A notable reduction in the masseter thickness was also evident post-TENS. Hence, TENS therapy may be considered as an effective therapeutic modality in the management of myofascial pain and myositis. The results of the present study suggest that ultrasonography is an effective tool in the evaluation of the efficacy of TENS.
Go to : 
References
1. Grossmann E, Tambara JS, Grossmann TK, de Siqueira JT. Transcutaneous electrical nerve stimulation for temporomandibular joint disorder. Rev Dor São Paulo. 2012; 13:271–276.
2. Blasberg B, Greenberg MS. Temporomandibular disorders. In : Greenberg MS, Glick M, Ship JA, editors. Burket's oral medicine. 11th ed. Hamilton: BC Decker Inc;2008. p. 223–256.
3. Ariji Y, Sakuma S, Izumi M, Sasaki J, Kurita K, Ogi N, et al. Ultrasonographic features of the masseter muscle in female patients with temporomandibular disorder associated with myofascial pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:337–341. PMID: 15356473.

4. Rajendran R. Diseases of nerves and muscles. In : Rajendran R, Sivapathasundharam B, editors. Shafer's textbook of oral pathology. 6th ed. Gurgaon: Reed Elsevier India Private Limited;2009. p. 844–860.
5. Ariji Y, Katsumata A, Hiraiwa Y, Izumi M, Sakuma S, Shimizu M, et al. Masseter muscle sonographic features as indices for evaluating efficacy of massage treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:517–526. PMID: 20868996.

6. Moger G, Shashikanth MC, Sunil MK, Shambulingappa P. Transcutaneous electrical nerve stimulation therapy in temporomandibular disorder: a clinical study. J Indian Acad Oral Med Radiol. 2011; 23:46–50.

7. Rodrigues D, Siriani AO, Bérzin F. Effect of conventional TENS on pain and electromyographic activity of masticatory muscles in TMD patients. Braz Oral Res. 2004; 18:290–295. PMID: 16089258.

8. Kato MT, Kogawa EM, Santos CN, Conti PC. TENS and low-level laser therapy in the management of temporomandibular disorders. J Appl Oral Sci. 2006; 14:130–135. PMID: 19089044.

9. Kogawa EM, Kato MT, Santos CN, Conti PC. Evaluation of the efficacy of low-level laser therapy (LLLT) and the microelectric neurostimulation (MENS) in the treatment of myogenic temporomandibular disorders: a randomized clinical trial. J Appl Oral Sci. 2005; 13:280–285. PMID: 20878031.

10. Zuim PR, Garcia AR, Turcio KH, Hamata MM. Evaluation of microcurrent electrical nerve stimulation (MENS) effectiveness on muscle pain in temporomandibular disorders patients. J Appl Oral Sci. 2006; 14:61–66. PMID: 19089032.

11. Aldemir K, Üstüner E, Erdem E, Demiralp AS, Oztuna D. Ultrasound evaluation of masseter muscle changes in stabilization splint treatment of myofascial type painful temporomandibular diseases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:377–383. PMID: 23953424.

12. Bakke M, Tuxen A, Vilmann P, Jensen BR, Vilmann A, Toft M. Ultrasound image of human masseter muscle related to bite force, electromyography, facial morphology, and occlusal factors. Scand J Dent Res. 1992; 100:164–171. PMID: 1631486.

13. Okeson JP. Functional anatomy and biomechanics of the masticatory system. In : Okeson JP, editor. Management of temporomandibular disorders and occlusion. 6th ed. St. Louis (MO): Mosby Elsevier;2008. p. 2–24.
14. List T, Helkimo M. Acupuncture and occlusal splint therapy in the treatment of craniomandibular disorders. II. A 1-year follow-up study. Acta Odontol Scand. 1992; 50:375–385. PMID: 1476055.

15. Wessberg GA, Carroll WL, Dinham R, Wolford LM. Transcutaneous electrical stimulation as an adjunct in the management of myofascial pain-dysfunction syndrome. J Prosthet Dent. 1981; 45:307–314. PMID: 6971327.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download