Although its etiology is unclear, calcific tendinitis is usually caused by the deposition of calcium hydroxyapatite crystals in periarticular muscle attachments such as the tendon, adjacent soft tissue, or ligament near the bone attachment. It is often accompanied with painful inflammation, exquisite tenderness, local swelling and redness, and limitation of the range of motion in the affected structures. The rotator cuffs of the shoulder are the most commonly affected structures in clinical practice. When calcific tendinitis affectsa hip lesion, which may occur with a low repetition rate, it usually causes pain in the buttock and the posterolateral aspect of the thigh, and this could mimic radicular pain of a herniated lumbar intervertebral disc. Therefore, misdiagnosis is common and leads to a delay in management. Here, we report the case of a 30-year-old woman with calcific tendinitis of the rectus femoris that was successfully managed with ultrasound-guided injection. The authors received written permission from the patient to report and provide details about this case.
CASE REPORT
A 30-year-old woman visited our clinic with pain on the right inguinal area and lateral aspect of the thigh, which spontaneously started 3 months ago and had become aggravated a week before. The pain intensity in the visual analogue scale (VAS) was about 80 of 100. Her height was 164 cm and body weight was 62 kg. She was a caddie, and had no specific medical or trauma history. She was experiencing right groin and thigh pain precipitated by walking, which made it difficult for her to walk normally. Lumbar magnetic resonance imaging (MRI) done at a previous clinic showed otherwise normal (
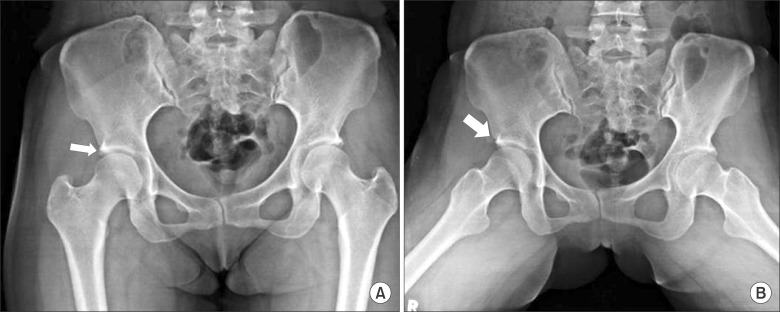
Fig. 1). In the previous clinic, lumbar epidural steroid injection was done twice in combination with medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxants for 2 months; however, these failed to improve her symptoms. She has even had a gynecological examination to rule out the disorder such as pelvic inflammatory disease, yield to normal. On physical examination, she complained of tenderness over the right buttock and the anterolateral aspect of the thigh, as well as pain with flexion and internal rotation of the right hip joint. Both the straight-leg-raising test and the flip test were negative, as concordant with previous MRI showing non-specific finding. Motor weakness and sensory alteration on the lower legs were not observed. Her body temperature was 36.3℃, and laboratory findings such as complete blood count, erythrocyte sedimentation rate, C-reactive protein, and rheumatoid factor were normal. We checked the hip radiograph and found a small amorphous calcification near the right anterior inferior iliac spine (AIIS)-the attachment site of the rectus tendon-suggesting calcific tendinitis of rectus femoris. Additionally, it was more visible in frog leg lateral views around the bony structure (
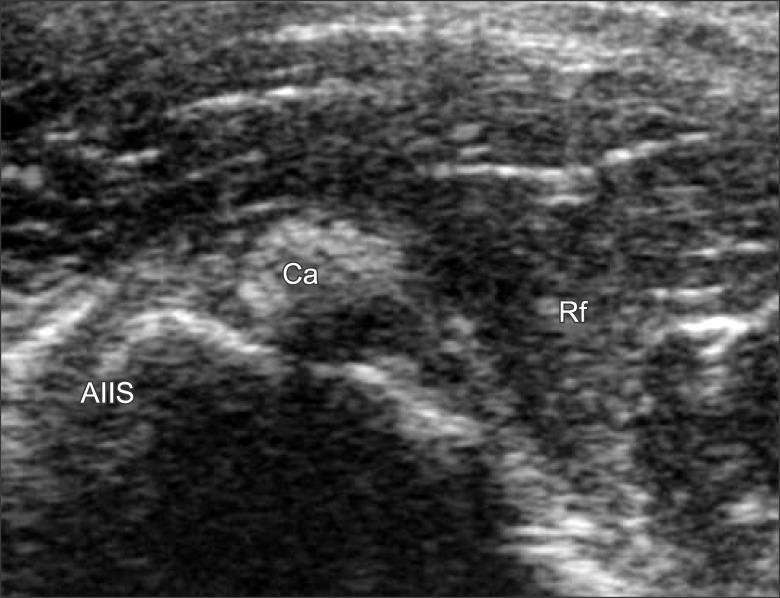
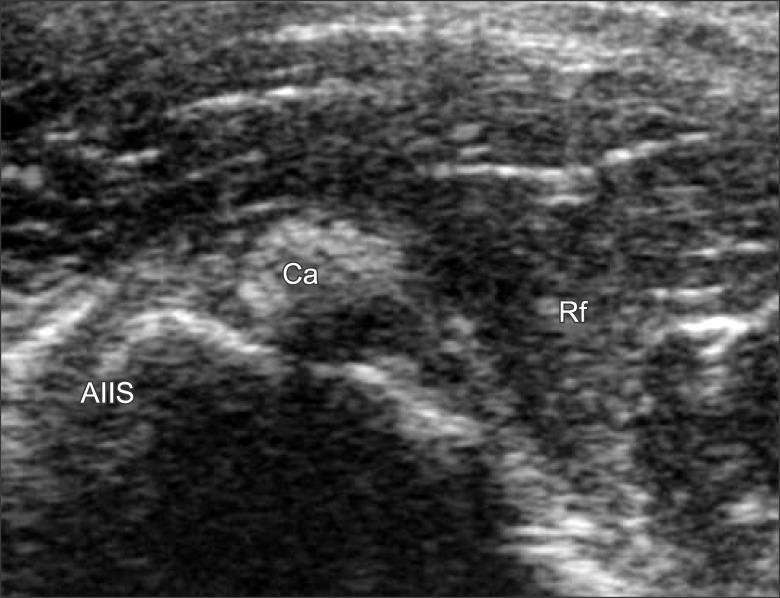
Fig. 2). On initial ultrasonography scanning on the tender area over the hip, oval- shaped calcification was seen with surrounding hyperechoic fat suggesting inflammation. Fluid collection was also noted (
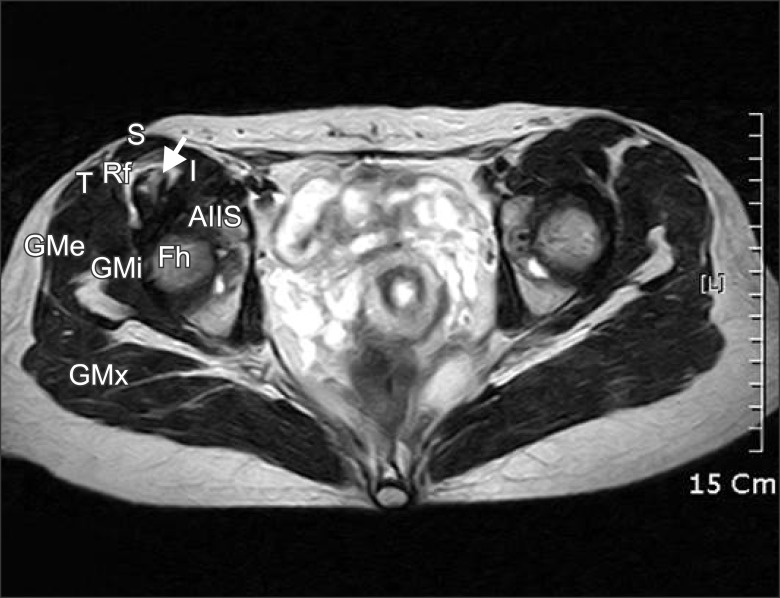
Fig. 3). Hip MRI was performed to confirm the diagnosis. In the MRI findings, calcification was noted in the right rectus femoris tendon, showing thickening with a small amount of fluid collection and edematous change of peripheral soft tissue (
Fig. 4). With the diagnosis of rectus femoris calcific tendinitis, injection therapy was planned.
 | Fig. 1Magnetic resonance imaging finding of the lumbar spine, sagittal plane. 
|
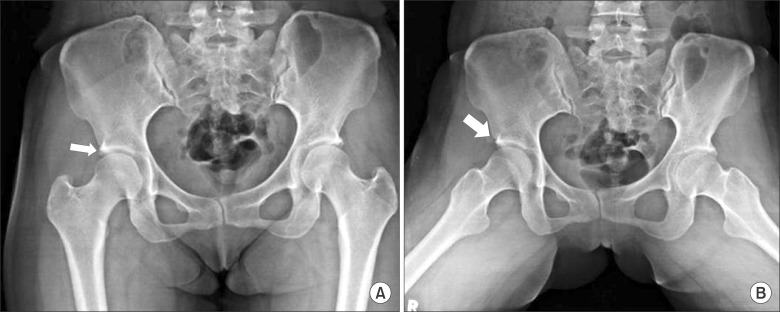 | Fig. 2Plain hip AP showed a small amorphous calcification near the right anterior inferior iliac spine, which is the attachment site of the rectus tendon, suggesting calcific tendinitis of rectus femoris (A). The lesion was more clearly defined when the patient posed frog leg position (B). 
|
 | Fig. 3Ultrasound scanning over the hip area showing calcification around the rectus femoris with mild fluid collection. AIIS: anterior inferior iliac spine, Ca: calcification, Rf: rectus femoris. 
|
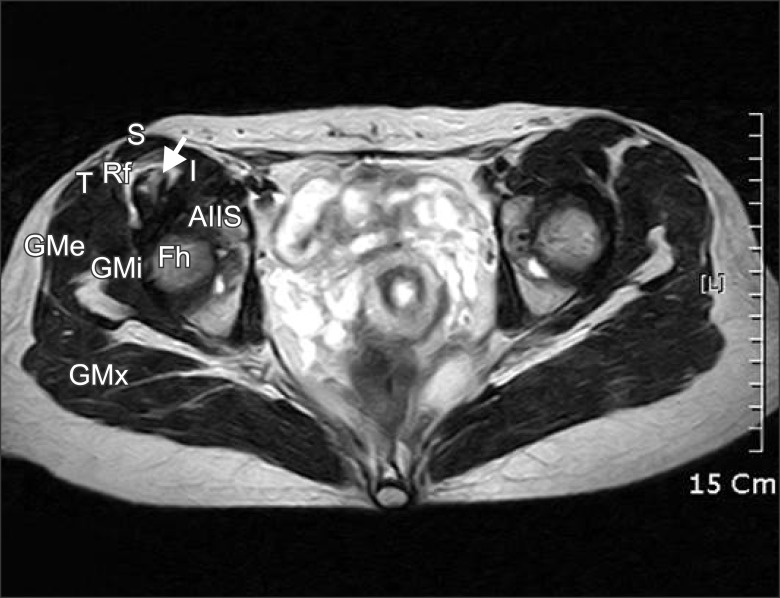 | Fig. 4Magnetic resonance imaging finding of the hip, axial plane. Calcification was noted in the right rectus femoris tendon showed thickening with small amount of fluid collection at the intermuscular fat plane. White arrow indicates calcification. AIIS: Anterior inferior iliac spine, Rf: Rectus femoris muscle and tendon, S: Sartorius muscle, I: Iliopsoas muscle, T: Tensor fasciae latae muscle, GMx: Gluteus maximus, GMe: Gluteus medius, GMi: Gluteus minimus. 
|
The patient was positioned in left lateral decubitus. With aseptic dressing, the transducer was positioned over the hip area to find the calcification. Around the calcified lesion, we injected 5 ml of 1% of mepivacaine with 20 mg triamcinolone acetate, by using a 25 G 38-mm needle (BD PrecisionGlide Needle; Becton Dickinson Medical, Singapore) with the short-axis in-plane technique. At 1 week intervals, additional injections were done in the same manner. The pain intensity started to decrease 2 days after the first injection and decreased to 0-10 of 100 in the VAS 3 days after the second injection. She returned to work in a pain-free state and after 6 weeks of follow-up, US image demonstrated decreased echogenicity of surrounding fat and also decreased amount of fluid collection with resolved symptom (
Fig. 5).
 | Fig. 5Ultrasonography scanning over the hip area, after 6 weeks. Decreased echogenicity of surrounding fat with decreased amount of fluid collection and size was observed. 
|
Go to :

DISCUSSION
Painful periarticular calcification is an acute inflammatory reaction, with pain, exquisite tenderness, local swelling, and redness. It is most commonly seen within the rotator cuffs of the shoulder, although it can develop around the wrist, elbow, hip, knee, foot, and, rarely, in the neck. In the hip area, since the report of King and Vanderpool [
1] in 1967, it has been rarely reported in the literature [
2,
3].
The exact etiology of the origin and resorption of the calcium deposits are not clearly understood, although several hypothetical mechanisms have been proposed. The only disorders reported to be associated with the disease are chronic renal failure with persistent hemodialysis and diabetes mellitus [
4]. Traumatic [
5], genetic [
6], and metabolic factors [
7] have been proposed as etiologies. However, historically, it was assumed that these deposits might have resulted from trauma around the involved joints, although no specific mechanism was elucidated. As repetitive trauma has been cited as a factor, especially in the shoulder region, tendinous tears of hip abductors have also been proposed to be related to calcific tendinitis [
8]. In this case, the patient's history of overuse of the hip abductors, in relation to her job that involves walking for 6-8 h a day, supported the above by describing repetitive trauma hypothesis.
It is known that periarticular calcific tendinitis can be classified as acute or chronic. In acute disease, most attacks last 2 weeks and the calcification disappears from radiographs at 4 weeks to 8 months post-onset. Despite its self-limiting nature, if mild or moderate pain persists for 2-24 months after disease onset, the disease can be classified as chronic [
7]. In the hip, it is known that calcification occurs at three sites, namely the tendon of the gluteus medius, the bursa between the tendon of the gluteus medius and the greater trochanter, and the undersurface of the gluteus medius but not connected to the trochanter [
9]. All locations can cause pain in the posterolateral aspect of the thigh that can simulate radicular pain from a herniated intervertebral disc [
10]. Hence, misdiagnosis is common and leads to a delay in treatment, as in our case; this case was primarily managed under the diagnosis of a herniated lumbar disc, and the patient's condition failed to improve.
The diagnosis is usually based on clinical suspicion and typical findings of plain radiography of the hip, locating calcific depositions in the tendon or bursa [
11]. However, plain radiography can lead to misdiagnosis without additional diagnostic tools, as the bone, adjacent soft tissue, ligaments, and tendons around hip are arranged three-dimensionally. Furthermore, if the calcification is very thin and small, and located in the posterior aspect, it is even more difficult to detect with only plain radiography, sometimes even in retrospective examinations. The use of the "frog-leg position" while obtaining the plain x-ray image also supports this three-dimensional anatomical characteristic as it was also shown in our case [
1].
In the diagnosis of calcific tendinitis, computed tomography (CT) allows the best visualization and localization of proper lesions, as well as facilitates accurate injection, when required. MRI can be a useful tool to rule out other conditions, especially when the lesions involve soft tissue areas, and to show the severity of inflammation [
5]. Ultrasonography is also useful in the evaluation of calcific tendinitis. Tendon calcification is seen as a hyperechoic focus. The real-time nature of ultrasonography has led to its use in both diagnostic and therapeutic procedures, as we did in our case. Ultrasonography is reliable for the detection and localization of calcifications; however, it is unable to classify the pathophysiologic phase. Therefore, clinical correlations and other radiographs are necessary to evaluate the disease [
12].
The differential diagnoses of calcifications in the rectus femoris include osacetabuli, avulsion fractures, sesamoid bones in the rectus femoris, myositis ossificans, and malignancies, usually based on the size, characteristic ovoid shape, bony trabeculation, and painlessness of the ossicle. The comet-tail appearance of the calcific deposit suggests that it lies within a tendon [
2].
Periarticular calcific tendinitis is widely accepted as a self-limited disease; however, some refractory patients need treatment because the duration of symptoms varies from months to years [
1]. The treatment options include conservative management such as rest, NSAIDs, local applications of heat and cold, arthroscopy, local surgical excision, and local steroid injection [
11]. Surgical excision is usually considered in case of long-lasting symptoms that are refractory to conservative treatment [
13]. Among the conservative modalities,local steroid and anesthetic injections provide rapid and long-lasting pain relief and shorten the clinical course. However, their mechanisms of action are still unclear. There are several literature reports in which a prompt diagnosis and early treatment with a local injection of corticosteroid under CT or fluoroscopy guidance were performed [
2,
3]. Both procedures yield diagnostic and therapeutic values. In this case, we first used ultrasonography to diagnose and treat the disease. Evaluating the general condition by using ultrasonography alone has some limitations; however, it has the benefits of convenience and the lack of radiation exposure compared with CT or fluoroscopy. It also allows real-time and dynamic assessments on physical examinations. There are insufficient cases reported in the literature in which ultrasonography was mainly used to treat calcific tendinitis in the hip area as this case, compared with that in the rotator cuff of the shoulder.
We performed local injection under ultrasound guidance because it has the advantage of real-time image acquisition, enabling fast and accurate diagnosis and treatment. Especially in a hip lesion, although a tiny calcification can cause severe pain, a misdiagnosis is easily made, causing the disease to progress into the chronic state. It is difficult to detect the calcification initially because of its rarity and the complex three-dimensional anatomic structure of the hip. It could be more easily found in conjugation with valid radiographs of the patient's pain area. Physicians should consider acute calcific tendinitis of the rectus femoris when making a differential diagnosis of hip pain, although it is a rare disease entity, as misdiagnosis leads to inappropriate treatment and delays in recovery. We also recommend ultrasonography in the evaluation of hip pain, as it can be used as a rapid and effective diagnostic and therapeutic tool.
Go to :






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download