1. Means-Christensen AJ, Roy-Byrne PP, Sherbourne CD, Craske MG, Stein MB. Relationships among pain, anxiety, and depression in primary care. Depress Anxiety. 2008; 25:593–600. PMID:
17932958.

2. Farb DH, Ratner MH. Targeting the modulation of neural circuitry for the treatment of anxiety disorders. Pharmacol Rev. 2014; 66:1002–1032. PMID:
25237115.

3. Almeida TF, Roizenblatt S, Tufik S. Afferent pain pathways: a neuroanatomical review. Brain Res. 2004; 1000:40–56. PMID:
15053950.

4. Willis WD, Westlund KN. Neuroanatomy of the pain system and of the pathways that modulate pain. J Clin Neurophysiol. 1997; 14:2–31. PMID:
9013357.

5. Price DD. Central neural mechanisms that interrelate sensory and affective dimensions of pain. Mol Interv. 2002; 2:392–403. 339PMID:
14993415.

6. Price DD. Psychological and neural mechanisms of the affective dimension of pain. Science. 2000; 288:1769–1772. PMID:
10846154.

7. Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MC. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997; 277:968–971. PMID:
9252330.

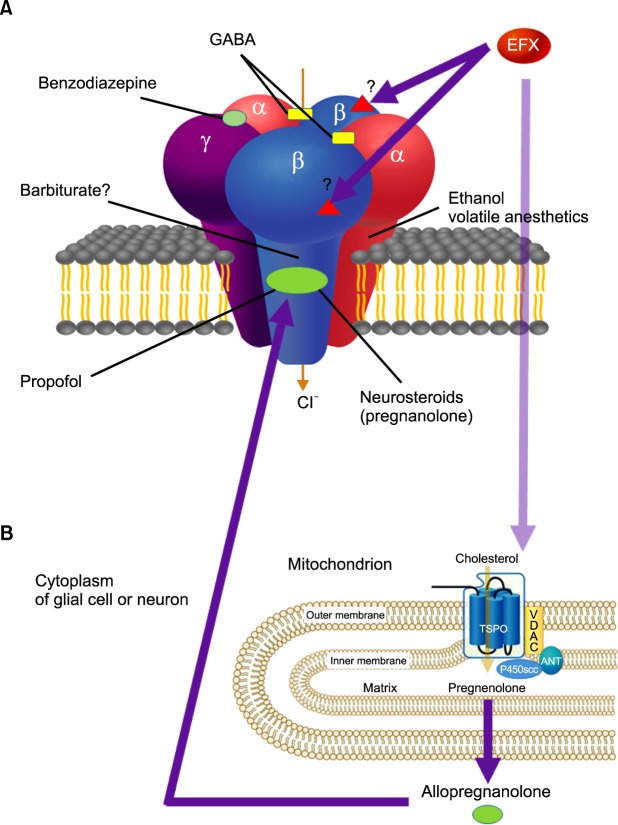
8. Hamon A, Morel A, Hue B, Verleye M, Gillardin JM. The modulatory effects of the anxiolytic etifoxine on GABA(A) receptors are mediated by the beta subunit. Neuropharmacology. 2003; 45:293–303. PMID:
12871647.

9. Schlichter R, Rybalchenko V, Poisbeau P, Verleye M, Gillardin J. Modulation of GABAergic synaptic transmission by the non-benzodiazepine anxiolytic etifoxine. Neuropharmacology. 2000; 39:1523–1535. PMID:
10854897.

10. Papadopoulos V, Baraldi M, Guilarte TR, Knudsen TB, Lacapère JJ, Lindemann P, et al. Translocator protein (18 kDa): new nomenclature for the peripheral-type benzodiazepine receptor based on its structure and molecular function. Trends Pharmacol Sci. 2006; 27:402–409. PMID:
16822554.

11. Zeilhofer HU. Etifoxine (Stresam) for chemotherapy-induced pain? Pain. 2009; 147:9–10. PMID:
19822395.

12. Kucken AM, Wagner DA, Ward PR, Teissére JA, Boileau AJ, Czajkowski C. Identification of benzodiazepine binding site residues in the gamma 2 subunit of the gamma-aminobutyric acid(A) receptor. Mol Pharmacol. 2000; 57:932–939. PMID:
10779376.
13. Sigel E, Steinmann ME. Structure, function, and modulation of GABA(A) receptors. J Biol Chem. 2012; 287:40224–40231. PMID:
23038269.

14. Scheller M, Forman SA. The gamma subunit determines whether anesthetic-induced leftward shift is altered by a mutation at alpha1S270 in alpha1beta2gamma2L GABA(A) receptors. Anesthesiology. 2001; 95:123–131. PMID:
11465549.

15. Olsen RW, Li GD. GABA(A) receptors as molecular targets of general anesthetics: identification of binding sites provides clues to allosteric modulation. Can J Anaesth. 2011; 58:206–215. PMID:
21194017.

16. Rupprecht R, Papadopoulos V, Rammes G, Baghai TC, Fan J, Akula N, et al. Translocator protein (18 kDa) (TSPO) as a therapeutic target for neurological and psychiatric disorders. Nat Rev Drug Discov. 2010; 9:971–988. PMID:
21119734.

17. Gunn BG, Brown AR, Lambert JJ, Belelli D. Neurosteroids and GABA(A) Receptor Interactions: A Focus on Stress. Front Neurosci. 2011; 5:131. PMID:
22164129.

18. Girard C, Liu S, Cadepond F, Adams D, Lacroix C, Verleye M, et al. Etifoxine improves peripheral nerve regeneration and functional recovery. Proc Natl Acad Sci U S A. 2008; 105:20505–20510. PMID:
19075249.

19. Girard C, Liu S, Adams D, Lacroix C, Sinéus M, Boucher C, et al. Axonal regeneration and neuroinflammation: roles for the translocator protein 18 kDa. J Neuroendocrinol. 2012; 24:71–81. PMID:
21951109.

20. Zhou X, He X, He B, Zhu Z, Zheng C, Xu J, et al. Etifoxine promotes glial derived neurotrophic factor induced neurite outgrowth in PC12 cells. MOL Med Rep. 2013; 8:75–80. PMID:
23670018.

21. Dai T, Zhou X, Li Y, He B, Zhu Z, Zheng C, et al. Etifoxine promotes glia-derived neurite outgrowth in vitro and in vivo. J Reconstr Microsurg. 2014; 30:381–388. PMID:
24956483.

22. Zhou X, He B, Zhu Z, He X, Zheng C, Xu J, et al. Etifoxine provides benefits in nerve repair with acellular nerve grafts. Muscle Nerve. 2014; 50:235–243. PMID:
24273088.

23. Daugherty DJ, Selvaraj V, Chechneva OV, Liu XB, Pleasure DE, Deng W. A TSPO ligand is protective in a mouse model of multiple sclerosis. EMBO Mol Med. 2013; 5:891–903. PMID:
23681668.

24. Aouad M, Charlet A, Rodeau JL, Poisbeau P. Reduction and prevention of vincristine-induced neuropathic pain symptoms by the non-benzodiazepine anxiolytic etifoxine are mediated by 3alpha-reduced neurosteroids. Pain. 2009; 147:54–59. PMID:
19786322.

25. Aouad M, Petit-Demoulière N, Goumon Y, Poisbeau P. Etifoxine stimulates allopregnanolone synthesis in the spinal cord to produce analgesia in experimental mononeuropathy. Eur J Pain. 2014; 18:258–268. PMID:
23881562.

26. Aouad M, Zell V, Juif PE, Lacaud A, Goumon Y, Darbon P, et al. Etifoxine analgesia in experimental monoarthritis: a combined action that protects spinal inhibition and limits central inflammatory processes. Pain. 2014; 155:403–412. PMID:
24239672.

27. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959; 32:50–55. PMID:
13638508.

28. McCracken LM, Zayfert C, Gross RT. The Pain Anxiety Symptoms Scale: development and validation of a scale to measure fear of pain. Pain. 1992; 50:67–73. PMID:
1513605.

29. McCracken LM, Dhingra L. A short version of the Pain Anxiety Symptoms Scale (PASS-20): preliminary development and validity. Pain Res Manag. 2002; 7:45–50. PMID:
16231066.

30. Micallef J, Soubrouillard C, Guet F, Le Guern ME, Alquier C, Bruguerolle B, et al. A double blind parallel group placebo controlled comparison of sedative and mnesic effects of etifoxine and lorazepam in healthy subjects [corrected]. Fundam Clin Pharmacol. 2001; 15:209–216. PMID:
11468032.

31. Nguyen N, Fakra E, Pradel V, Jouve E, Alquier C, Le Guern ME, et al. Efficacy of etifoxine compared to lorazepam monotherapy in the treatment of patients with adjustment disorders with anxiety: a double-blind controlled study in general practice. Hum Psychopharmacol. 2006; 21:139–149. PMID:
16625522.

32. Verleye M, Gillardin JM. Effects of etifoxine on stress-induced hyperthermia, freezing behavior and colonic motor activation in rats. Physiol Behav. 2004; 82:891–897. PMID:
15451655.

33. Moch C, Rocher F, Lainé P, Lacotte J, Biour M, Gouraud A, et al. Etifoxine-induced acute hepatitis: A case series. Clin Res Hepatol Gastroenterol. 2012; 36:e85–e88. PMID:
22633197.

34. Nadendla LK, Meduri V, Paramkusam G, Pachava KR. Evaluation of salivary cortisol and anxiety levels in myofascial pain dysfunction syndrome. Korean J Pain. 2014; 27:30–34. PMID:
24478898.

35. Cho SK, Heiby EM, McCracken LM, Moon DE, Lee JH. Daily functioning in chronic pain: study of structural relations with posttraumatic stress disorder symptoms, pain intensity, and pain avoidance. Korean J Pain. 2011; 24:13–21. PMID:
21390174.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download