Abstract
Brachial plexus block (BPB) under ultrasound guidance has come to be widely used. However, nerve injury has been reported following ultrasound-guided BPB. We hypothesized that BPB under ultrasound guidance in conjunction with real-time electrical nerve stimulation would help us prevent nerve injury and do more successful procedure. Here, we report the successful induction and maintenance of ultrasound-guided BPB and the achievement of good peri- and postoperative pain control using a conductive catheter, the EpiStim®.
Go to : 
Brachial plexus block (BPB) under ultrasound guidance has come to be widely used because the application of ultrasound can improve success rate of the procedure and prevent nerve injury. However, nerve injury has been reported following ultrasound-guided BPB.
We hypothesized that direct visualization of neural structures under ultrasound guidance in conjunction with real-time electrical nerve stimulation would help us prevent nerve injury and do more successful procedure. Here, we report the successful ultrasound-guided BPB using a conductive catheter, the EpiStim® (Sewoon Medical Co. Ltd, Seoul, Korea), placed through electrical nerve stimulation in a 50-year-old man undergoing thumb surgery for a chainsaw injury. Also, it is particularly useful to manage a peri- and postoperative pain control.
A 50-year-old man presented to our hospital with a chainsaw injury to his right thumb. On admission, the patient exhibited sensory loss on the radial side due to an interphalangeal joint level injury. He was scheduled to undergo emergency surgery to restore the thumb. All laboratory tests performed for preoperative evaluation returned normal results. Upon arrival of the patient in the operating room, electrocardiography and pulse oximetry were initiated for vital sign monitoring. The patient was placed in the supine position with the arm abducted and externally rotated to 90°, and the axilla was sufficiently disinfected with Hibicol (2% chlorhexidine and 75% alcohol) and aseptically draped. The SonoSite M-Turbo (SonoSite®, Bothell, WA, USA) ultrasound device, a 38 mm, 7-12 MHz linear array transducer was covered with sterile transparent plastic wrap and placed in the patient's axillary wrinkles so that the axillary artery and nerves could be visible on the shorter side of the transducer. After the skin and subcutaneous tissue around the axillary wrinkles was anesthetized with 1% lidocaine, a Tuohy needle was positioned close to the brachial plexus under sonographic guidance (Fig. 1).
An EpiStim® conductive catheter was inserted through the Tuohy needle and the guide wire within the catheter was connected to a peripheral nerve stimulator (MultiStim SENSOR, PAUJNK® GmbH Medizintechnologie, Geisingen, Germany) using a connector. The tip of the catheter was located near the radial nerve. The intensity of the stimulation was then gradually increased from 0.25 mA to 1.0 mA until the stimulation corresponding to the dermatome with lesions was confirmed. The minimum responsive stimulation intensity was 0.5 mA.
After confirming the exact location of the catheter in the brachial plexus through electrical nerve stimulation, the guide-wire was removed and 0.38% ropivacaine hydrochloride (Naropin®, AstraZeneca plc, London, UK) 15 ml was injected. Five minutes after the injection, sensory loss and decreased motor movements were confirmed. The catheter was subsequently secured to the skin with 2-0 black silk to prevent dislocation, and then dressings were applied for further fixation. The surgery lasted for over 150 min, dexmedetomidine hydrochloride (Precedex®, Hospira Inc., Lake Forest, IL, USA) was continuously injected at the rate of 0.5 µg/kg/min as a sedative. Immediately after the surgery, the patient was transferred to a recovery room. None of the common surgical complications such as nerve injury, hematoma, numbness, or paresthesia were observed. The patient was moved to the general ward an hour later, immediately following an injection of 10 ml of 0.38% ropivacaine through the catheter for pain control. He experienced mild postoperative pain, represented by a visual analog scale score of 2/10. The patient was expected to be discharged the day after the surgery, and the catheter was removed 12 h after the operation.
Go to : 
BPB under ultrasound guidance has come to be widely used of late [1]. Utilization of ultrasound prevents many complications, including brachial plexus injury, vessel punctures, pneumothorax, and hemothorax, among others [2345]. However, nerve injuries have been reported despite identification of the locations of various structures using ultrasound imaging prior to insertion of the needle close to the target nerve [6789]. Thus we postulated that direct visualization of neural structures under ultrasound guidance in combination with real-time electrical nerve stimulation would help us prevent nerve injury.
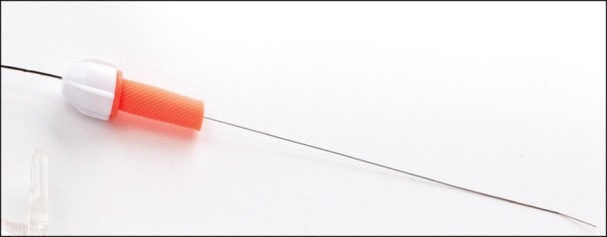
The EpiStim® is an end-hole-type epidural catheter with a bent-tip conductive guide-wire (Fig. 2). The conductive guide-wire can be used to deliver an electrical stimulation via the catheter tip, allowing the nerve to be electrically stimulated so that the corresponding dermatome will respond. So, through the use of electrical nerve stimulation, the catheter tip can be accurately placed close to the nerve innervating the surgical site.
In the present case, the intensity of nerve stimulation was gradually increased until the patient responding to the stimulation. The intensity of stimulation felt by the patient was found to be approximately 0.5 mA, which is the minimum value required to position the EpiStim® in a specific neuromuscular region. Motor response at very-low-current intensity (<0.2 mA, 0.1 ms) may indicate intra-neural needle placement [10]. Therefore, this method can aid in preventing nerve injury during BPB induction.
Moreover, the EpiStim® is useful for pain control because it allows the local anesthetic agent to be continuously injected. In our case, one unfortunate point was that the patient was discharged 24 h after the operation, so the catheter was removed 12 h after the surgery. If the patient had been admitted for a longer period of time, the catheter could have been used more effectively for pain control. However, during his recovery, the patient was satisfied with his pain control, so we estimate that it was a good procedure. Although the EpiStim® is a high cost device and it has some economic limitation, it is a valuable device to prevent nerve injury and related complications.
In conclusion, ultrasound-guided BPB using a conductive catheter, the EpiStim®, placed through electrical nerve stimulation, can prevent nerve injury and allow identification of the exact location of the brachial plexus, which results in successful regional anesthesia and good peri- and postoperative pain control.
Go to : 
References
1. Chan VW, Peng PW, Kaszas Z, Middleton WJ, Muni R, Anastakis DG, et al. A comparative study of general anesthesia, intravenous regional anesthesia, and axillary block for outpatient hand surgery: clinical outcome and cost analysis. Anesth Analg. 2001; 93:1181–1184. PMID: 11682392.

2. Imasogie N, Ganapathy S, Singh S, Armstrong K, Armstrong P. A prospective, randomized, double-blind comparison of ultrasound-guided axillary brachial plexus blocks using 2 versus 4 injections. Anesth Analg. 2010; 110:1222–1226. PMID: 20142336.

3. Bernucci F, Gonzalez AP, Finlayson RJ, Tran DQ. A prospective, randomized comparison between perivascular and perineural ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012; 37:473–477. PMID: 22660484.

4. Tran DQ, Pham K, Dugani S, Finlayson RJ. A prospective, randomized comparison between double-, triple-, and quadruple-injection ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012; 37:248–253. PMID: 22354104.

5. Chan VW, Perlas A, McCartney CJ, Brull R, Xu D, Abbas S. Ultrasound guidance improves success rate of axillary brachial plexus block. Can J Anaesth. 2007; 54:176–182. PMID: 17331928.

6. Jung MJ, Byun HY, Lee CH, Moon SW, Oh MK, Shin H. Medial antebrachial cutaneous nerve injury after brachial plexus block: two case reports. Ann Rehabil Med. 2013; 37:913–918. PMID: 24466530.

7. Asheghan M, Khatibi A, Holisaz MT. Paresthesia and forearm pain after phlebotomy due to medial antebrachial cutaneous nerve injury. J Brachial Plex Peripher Nerve Inj. 2011; 6:5. PMID: 21896172.

8. Yildiz N, Ardic F. A rare cause of forearm pain: anterior branch of the medial antebrachial cutaneous nerve injury: a case report. J Brachial Plex Peripher Nerve Inj. 2008; 3:10. PMID: 18426569.

9. Barrington MJ, Watts SA, Gledhill SR, Thomas RD, Said SA, Snyder GL, et al. Preliminary results of the Australasian Regional Anaesthesia Collaboration: a prospective audit of more than 7000 peripheral nerve and plexus blocks for neurologic and other complications. Reg Anesth Pain Med. 2009; 34:534–541. PMID: 19916206.

10. Reiss W, Kurapati S, Shariat A, Hadzic A. Nerve injury complicating ultrasound/electrostimulation-guided supraclavicular brachial plexus block. Reg Anesth Pain Med. 2010; 35:400–401. PMID: 20607905.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download