Abstract
Caudal epidural injection is a common intervention in patients with low back pain and sciatica. Even though the complications of fluoroscopically directed epidural injections are less frequent than in blind epidural injections, complications due to contrast media can occur. We report a case of anaphylactic shock immediately after injection of an intravenous nonionic contrast medium (iohexol) during the caudal epidural injection for low back pain and sciatica in a patient without a previous allergic history to ionic contrast media (ioxitalamate). Five minutes after the dye was injected, the patient began to experience dizziness, and the systolic blood pressure dropped to 60 mmHg. Subsequently, the patient exhibited a mild drowsy mental state. About 30 minutes after the subcutaneous injection of 0.2 mg epinephrine, the systolic blood pressure increased to 90 mmHg. The patient recovered without any sequela. Life-threatening complications after injection of intravenous contrast medium require immediate treatment.
Go to : 
The prevalence of chronic spinal pain is gradually increasing in Korea [1]. Epidural injections are commonly used interventions for managing spinal pain. One of these interventions is a caudal block that is commonly performed by physicians and is considered a safe and easy approach, with minimal risk of inadvertent dural puncture [23].
Caudal epidural injections have been reported to be associated with a few complications. Even though the complications of fluoroscopically guided caudal epidural injections are less frequent than in blind epidural injections, caudal epidural injections guided by fluoroscopy are not devoid of complications. The use of contrast media has a risk of adverse effects, from mild rash to fatal anaphylaxis or anaphylactoid reaction that can lead to death [45].
Anaphylactic shock due to contrast medium is a serious but rare complication. We report a case of severe anaphylactic shock caused by a nonionic contrast medium (iohexol) following caudal epidural injection for low back pain and sciatica in a patient without a previous allergic history to ionic contrast media (ioxitalamate).
A 78-year-old woman visited the pain clinic for management of low back pain and sciatica. The patient did not have any underlying disease except for hypertension. The patient recently underwent a caudal epidural block and a transforaminal epidural block 6 times in a year by using an ionic contrast medium (ioxitalamate, Telebrix®). She underwent a caudal epidural block 4 times, and had no history of allergic reactions to contrast media or other substances. All procedures were performed without complications.
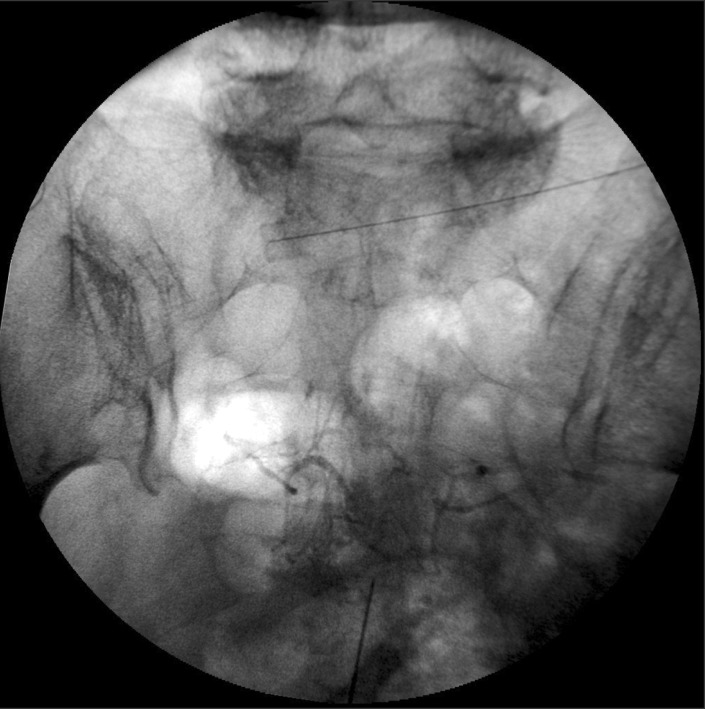
Magnetic resonance imaging revealed central stenosis at the L 2-3 and L 3-4 levels and spondylolisthesis at the L5-S1 level. Full informed consent was obtained from the patient prior to performing the procedure. The patient was placed in the prone position, and the sacral hiatus was typically identified between the sacral cornua. The sacral hiatus was punctured with a 22 G epidural needle through the sacrococcygeal membrane. The epidural space was confirmed by fluoroscopy with a C-arm. After the needle was advanced 2-3 cm, 1 ml of nonionic contrast media (iohexol, Omnipaque®, GE Healthcare co., Uhan, China) was injected for confirming that there was no intravascular injection or abnormal flow. Nonionic contrast media (300 mg/ml) was used as undiluted state. After the first dye injection, we detected intravascular injection of the dye (Fig. 1). We displaced the needle and injected an additional 1 ml of the dye, and again detected the intravascular injection. We then withdrew and repositioned the needle and injected the dye. This time, the intravascular and intrathecal injection of the dye remained undetected. We initially planned to perform a caudal block, with a mixture of 12 ml of lidocaine hydrochloride (0.5%, preservative free) and 5 mg of dexamethasone prior to the procedure. However, we decided to administer 5 mg of dexamethasone and 9 ml of normal saline instead through the caudal epidural space. Five minutes after the dye was injected, the patient began to experience dizziness but no other symptoms and was transferred to the recovery room for management of vital signs.
At the recovery room, the patient's blood pressure dropped to 60/40 mmHg, heart rate was 100 bpm, peripheral oxygen saturation (SpO2) was 98%, and the electrocardiography showed normal sinus rhythm without ischemic changes. Moreover, the patient exhibited a mild drowsy mental state without any rash or edema. Immediately 10 L/min O2 was administered to the patient through a facial mask. Then, 500 ml of normal saline solution was rapidly loaded and 0.5 mg of atropine and 10 mg of ephedrine was injected intravenously. However, the blood pressure did not improve and the patient continued to remain in a drowsy state. We subcutaneously injected 0.2 mg epinephrine and closely monitored the patient. About 30 minutes later, the blood pressure increased to 90/60 mmHg and the patient was awake. Around 1 hour later, the dizziness resolved and the patient successfully carried out an order. The vital signs became more stable (blood pressure, 100/70 mmHg; heart rate, 80 bpm; SpO2, 98%). The patient recovered without any sequela. The patient refused any additional examination (intradermal skin test, IgE) to identify the cause of the allergic reaction.
Go to : 
Caudal epidural injection is a common intervention in patients with low back pain and sciatica. Even though the complications of fluoroscopically directed epidural injections are less frequent than in blind epidural injections, complications due to contrast media can occur [678].
Contrast material is generally well tolerated, although approximately 1% of patients who receive nonionic contrast media will develop anaphylaxis symptoms. Pharmacologic side effects occur due to the characteristic properties of contrast material such as osmolality, ionicity, and viscosity. The grade of anaphylaxis can be divided to 3 types according to Brown SG [9]: mild (grade 1), cutaneous symptoms such as generalized urticaria, periorbital edema, or angio-edema; moderate (grade 2), respiratory, cardiovascular, or gastrointestinal involvement such as dyspnea, stridor, wheeze, nausea, vomiting, dizziness (presyncope), diaphoresis, chest or throat tightness, or abdominal pain; and severe (grade 3), hypoxia, hypotension, or neurologic compromise such as cyanosis or SpO2 ≤ 92%, hypotension (SBP < 90 mm Hg in adults), confusion, collapse, loss of consciousness, or incontinence [9]. In this case, the patient experienced grade 3 anaphylaxis. The risk for severe reactions-that is, anaphylaxis grade 3-has been estimated to range from 0.02% to 0.04% with nonionic contrast material [3456].
Most anaphylactic reactions are mild and non-allergic. The risk of fatal adverse reactions due to iodinated contrast media has decreased owing to the development of ionic, high osmolality to nonionic, low osmolality contrast media. Katayama et al. [10] reported that the incidence of adverse reactions with iodinated contrast was 12.66% for ionic and 3.13% for non-ionic contrast media. Nevertheless, adverse reactions of nonionic contrast media still occur, and some physicians reported that patients exposed to nonionic contrast had higher incidences of severe adverse reactions [11]. Fatal adverse reactions can occur in 0.04% to 0.22% of cases.
In this case, the patient previously underwent a caudal block or transforaminal epidural block once in 2 months using ionic contrast medium (ioxitalamate, Telebrix®). During the procedures, we always used the dye and checked it. The patient had never experienced severe adverse reactions due to ionic contrast medium, lidocaine, or dexamethasone. Furthermore, the patient did not have an allergic history to other drugs either. Recently, anaphylactic shock due to ionic contrast medium occurred in our hospital, so we changed contrast medium from ionic contrast medium (Telebrix®) to nonionic contrast media (Omnipaque®). For the first time in this procedure, we used nonionic contrast media (iohexol, Omnipaque®), after which the patient experienced a fatal adverse reaction. These findings suggest that a patient without a previous allergic history to ionic contrast media can experience adverse events with nonionic contrast media, although the incidence of such cases is low. Nonionic agents have been developed to obviate the adverse effects of ionic contrast media. However, in this case, the situation was reversed. It is important to emphasize that adverse events are not always related to a history of allergy and can occur even if the medical practitioner uses any medicine.
Anaphylaxis refers to a systemic immediate hypersensitivity reaction that can be IgE-mediated or non-IgE mediated. In the clinical setting, the mechanism cannot be determined. The severe reactions of anaphylaxis due to nonionic contrast media are determined by IgE titers, and the anaphylactic reaction itself is assessed on the basis of the levels of histamine or other mediators. Trcka et al. [12] reported that, in more than 90% of cases, the direct release of histamine and other mediators was responsible for the anaphylaxis symptoms after administration of nonionic contrast material, and an IgE-mediated contrast material allergic reaction was identified in 4 of 96 examined patients. The classic hypothesis around IgE-mediated anaphylaxis is that the patient has to be sensitized towards the allergen before the full-blown reaction. Administration of the dye several times possibly caused this sensitization [13].
Hemodynamic instability due to dye was caused by anaphylactoid shock or coronary spasm. Wang et al. [14] reported 2 cases of severe coronary artery spasm with anaphylactoid shock caused by contrast medium. In patients with hypotension secondary to coronary artery spasm, nitroglycerin should be administered, after which favorable responses have been reported. However, the hemodynamic changes due to severe coronary artery spasm and anaphylactoid shock can be difficult to distinguish. The possibility of anaphylactoid shock should also be considered. In cases such as the present, epinephrine should be administered to maintain adequate blood pressure. In this case, we considered the possibility of anaphylactoid shock and therefore administered epinephrine. In this case, the patient was of advanced age and did not have ventricular arrhythmia. Also we feared an over-reaction to epinephrine. Therefore, we administered epinephrine subcutaneously instead of intravenously.
Caudal epidural complications rates have been widely studied. Manchikanti et al. [15] performed intravascular injection of contrast media in 3.1% of caudal epidural block procedures. Although rare, life-threatening anaphylaxis has occurred after intravenous injection of contrast media. Diagnosis and treatment of anaphylaxis should be performed promptly. Emergency protocols and trained medical staff are essential for a successful outcome, an important reason for our patient's recovery without sequela despite old age.
A limitation of this report is the lack of intradermal skin test results for the contrast medium and serum immunologic tests. We also do not have definite evidence that the allergic reaction was caused by the nonionic contrast because the patient refused to undergo any additional examination. However, after the last dye was injected, we injected only dexamethasone and normal saline. Therefore, we suppose that this adverse reaction occurred due to the nonionic contrast. To identify the cause of anaphylaxis, patients with a history of grade 2 or 3 anaphylaxis symptoms should be subjected to an allergologic workup. Skin testing with a panel of different contrast materials appears to be useful for confirming the presence of an IgE-mediated allergy and for identifying alternative contrast material that can be used safely. On the basis of available trials, Delaney et al. [4] reported that the use of H1 antihistamines and corticosteroids can be used to prevent anaphylactoid reactions to radiological contrast media, although those were underpowered studies. In patients with a previous allergic reaction to contrast material, prophylactic antihistamines or corticosteroids can be considered.
In conclusion, fatal adverse reactions due to nonionic contrast are less frequent than with ionic contrast. However, in terms of the possibility of life-threatening reactions, medical practitioners should always be aware of the risk of serious adverse reactions when practitioners perform epidural injections using nonionic contrast medium. Patients should be carefully monitored during and after the procedure. The medical practitioner must additionally promptly respond to unexpected reactions due to the contrast material. Emergency equipment, drugs, and trained personnel should always be immediately available whenever these procedures are performed.
Go to : 
References
1. Cho NH, Jung YO, Lim SH, Chung CK, Kim HA. The prevalence and risk factors of low back pain in rural community residents of Korea. Spine (Phila Pa 1976). 2012; 37:2001–2010. PMID: 22588379.

2. Doo AR, Kim JW, Lee JH, Han YJ, Son JS. A comparison of two techniques for ultrasound-guided caudal injection: the influence of the depth of the inserted needle on caudal block. Korean J Pain. 2015; 28:122–128. PMID: 25852834.

3. Parr AT, Manchikanti L, Hameed H, Conn A, Manchikanti KN, Benyamin RM, et al. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain Physician. 2012; 15:E159–E198. PMID: 22622911.
4. Delaney A, Carter A, Fisher M. The prevention of anaphylactoid reactions to iodinated radiological contrast media: a systematic review. BMC Med Imaging. 2006; 6:2. PMID: 16643668.

5. Bush WH Jr, Mullarkey MF, Webb DR. Adverse reactions to radiographic contrast material. West J Med. 1980; 132:95–98. PMID: 7385829.
6. ten Dam MA, Wetzels JF. Toxicity of contrast media: an update. Neth J Med. 2008; 66:416–422. PMID: 19011267.
7. Wolf GL, Arenson RL, Cross AP. A prospective trial of ionic vs nonionic contrast agents in routine clinical practice: comparison of adverse effects. AJR Am J Roentgenol. 1989; 152:939–944. PMID: 2495706.

8. Caro JJ, Trindade E, McGregor M. The risks of death and of severe nonfatal reactions with high- vs low-osmolality contrast media: a meta-analysis. AJR Am J Roentgenol. 1991; 156:825–832. PMID: 1825900.

9. Brown SG. Clinical features and severity grading of anaphylaxis. J Allergy Clin Immunol. 2004; 114:371–376. PMID: 15316518.

10. Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, Matsuura K. Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. 1990; 175:621–628. PMID: 2343107.

11. Lasser EC, Lyon SG, Berry CC. Reports on contrast media reactions: analysis of data from reports to the U.S. Food and Drug Administration. Radiology. 1997; 203:605–610. PMID: 9169676.

12. Trcka J, Schmidt C, Seitz CS, Bröcker EB, Gross GE, Trautmann A. Anaphylaxis to iodinated contrast material: nonallergic hypersensitivity or IgE-mediated allergy? AJR Am J Roentgenol. 2008; 190:666–670. PMID: 18287437.

13. Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, et al. The diagnosis and management of anaphylaxis practice parameter: 2010 update. J Allergy Clin Immunol. 2010; 126:477–480.e1-42. PMID: 20692689.

14. Wang CC, Chang SH, Chen CC, Huang HL, Hsieh IC. Severe coronary artery spasm with anaphylactoid shock caused by contrast medium--case reports. Angiology. 2006; 57:225–229. PMID: 16518532.

15. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012; 15:131–140. PMID: 22430650.
Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download