Abstract
Facet joint synovial cysts are usually associated with osteoarthritis of the adjacent facet joint and/or spondylolisthesis. In between the conservative and operative ends of the treatment spectrum lie minimally invasive techniques such as cyst rupture using epiduroscopy. In this report, we describe an 82-year-old male patient presenting with low back pain radiating to his lower left extremity and associated paresthesia. Magnetic resonance imaging of the lumbar spine revealed a synovial cyst at left L4/5 facet joint. Using epiduroscopy, the cyst was mechanically ruptured by popping it with the tip of the scope. The patient remained symptom-free at his successive visits until 12 months after the procedure, and was opened for desired follow up.
Go to : 
Synovial cysts of the spine are cysts that arise from the zygapophyseal joint capsule of the lumbar spine, which often cause radicular pain [1]. The number of reported synovial cysts of the lumbar spine has been increasing, likely due to the availability of the technique of magnetic resonance imaging (MRI). These cysts are usually associated with osteoarthritis of the adjacent facet joint and/or spondylolisthesis, particularly in middle-aged or elderly patients. Conservative treatments such as medications and facet joint or epidural injections are sometimes effective, although surgical resection is required in some cases due to persistent radicular symptoms and/or occasional paresis.
Although surgical resection provides satisfactory immediate resolution, there remains the possibility of recurrence, leading to the debate regarding the necessity of fusion, which may result in troublesome long-term problems such as failed back surgery syndrome. As facet cysts seem to be mainly related to spinal segmental instability, which will eventually resolve as the spine settles into the stabilization phase of degeneration, minimally invasive techniques such as cyst rupture without surgery, although associated with frequent recurrence, may have a rationale.
In this report, we describe an intraspinal facet joint cyst successfully treated by epiduroscopy. To our knowledge, there have been no other published articles on the epiduroscopic removal of a lumbar facet joint cyst, and this is the first report on epiduroscopic facet cyst removal.
An 82-year-old male patient visited our pain center due to low back pain radiating to his lower left extremity with associated paresthesia. The location of the pain was primarily the left buttock, which radiated laterally through the thigh to the foot, and its intensity was 6 out of 10 on the visual analogue scale (VAS). The patient had a history of right L5 transforaminal epidural injection due to right foraminal stenosis accompanied by grade 1 degenerative spondylolisthesis at L4/5 level, which resulted in improvement of the pain, and he had been lost to follow-up 3 years earlier.
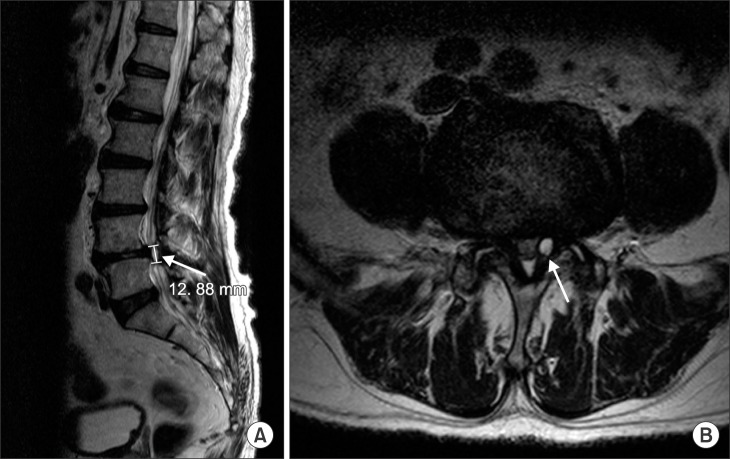
X-ray image showed grade 1 degenerative spondylolisthesis at L4/5 level, and there were no significant differences since the last study. Physical examination revealed decreased straight leg raising test results for the left lower extremity and tenderness around the left L4/5 facet joint area. Under the impression of lumbar radiculopathy, a transforaminal epidural steroid injection was given under fluoroscopic guidance at the left L5 level, without satisfactory improvement in symptoms. Gabapentin was started and increased to 300 mg three times a day, and limaprost 5 mcg and Ultracet tab® (tramadol 37.5 mg/acetaminophen 325 mg, Janssen Korea Ltd., Seoul, Korea) 0.5 tablet three times a day were prescribed, but the patient did not report improvement in symptoms. To diagnose the newly developed lower left extremity radiating pain, an MRI of the lumbar spine was newly performed. This revealed a synovial cyst at the left L4/5 facet joint, not previously observed 3 years earlier. The size of the cyst was 5 × 6 × 13 mm. No other lesions that could explain the left-sided radiating symptoms were observed (Fig. 1).
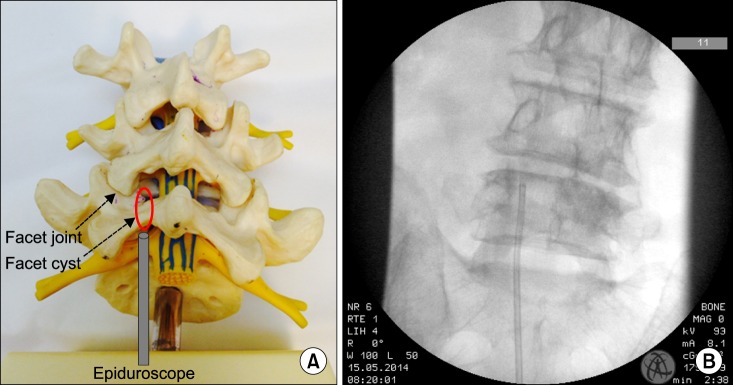
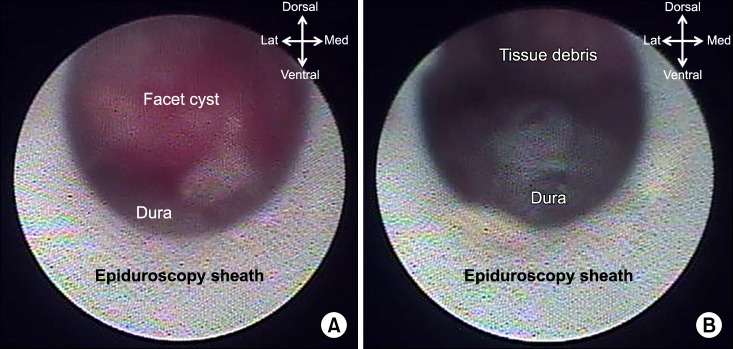
We planned facet cyst removal with epiduroscopy, since the location of the cyst was inside the spinal canal, rendering facet joint injection ineffective. With the patient in prone position, following the placement of sterile drapes, an epidural needle was inserted via the sacral hiatus under C-arm guidance, and an epidural catheter was placed using the Seldinger technique over the guidewire inserted through the needle. Then, an epiduroscope (BioVision 3.0 mm®, BioVision Technologies, LLC, Golden, CO, USA) was inserted through the epidural catheter (Fig. 2). The mass was cystic in shape, inflamed with reddish appearance, and occupying the epidural space. After confirming the location of the cyst near the L4/5 facet joint with the epiduroscope, targeted laser ablation was attempted, but this procedure failed technically, since localizing the laser focus over the cyst was practically impossible. After several trials, we decided to mechanically rupture the cyst by popping it with the tip of the scope (Fig. 3A). Following several repetitions of mechanical compression on the cyst with the epiduroscope, cyst rupture was visually confirmed (Fig. 3B). After the rupture of the cyst, normal saline irrigation was performed, and a mixture of dexamethasone 5 mg and hyaluronidase 1,500 U mixed with 0.18% ropivacaine 4 ml, was subsequently injected. After final fluoroscopic confirmation, the procedure was completed. The patient intermittently complained of moderate pain during the manipulation with the epiduroscope, therefore ketorolac 30 mg was intravenously administered.
The patient stayed at the day clinic for 4 hours for observation following the procedure, and was discharged without any neurologic complications. When he visited the clinic 1 week after the procedure, his radiating pain and associated paresthesia were no longer present, his VAS score was 0, and the straight leg raising test was negative. The patient remained symptom-free at his follow-up visits at 1 and 2 months after the procedure, and the medications except limaprost were all stopped. He was still symptomfree at his visit 12 months after the procedure, and was opened for desired follow-up.
Go to : 
We successfully removed a facet joint cyst at L4/5 level by epiduroscopy. There have been no previously published articles on the epiduroscopic removal of a lumbar facet joint cyst, and this is the first report. The pathogenesis of facet joint cysts is the subject of some debate, although it is generally accepted that it is a part of the spinal degenerative process, in which spinal instability and trauma play important roles [2]. Definite association of these cysts with osteoarthritis (40.5%), spondylolisthesis (43.4%), and disc degeneration (13.2%) emphasizes the degenerative nature of their pathogenesis, thus their tendency to be ailments of patients in their mid-60s or 70s [3]. The incidence of facet joint cysts is reported as 2.2-10% in the literature [45], and L4/5 is the most prevalent level, followed by L5/S1, L3/4, and L2/3, respectively [6]. It is known that 88-99% of spinal synovial cysts occur in the lumbar spine, while cervical (1-4%) or thoracic (0-8%) lesions are less frequent [789]. The most common presenting symptoms are back pain and/or radiculopathy, as found in 55-97% of symptomatic cases, and other symptoms such as neurogenic claudication and cauda equina syndrome may be present in some portion of patients, especially those with spinal stenosis [10]. The current standard diagnosis is made by MRI, observed as T1-weighted hypointense and T2-weighted hyperintense structures because of the proteinaceous content of the cysts, and T1-weighted contrast- enhanced images may occasionally show cystic wall enhancement [311].
The treatment is mainly surgical [10]. Although there are some reports of spontaneous regression of cysts, most reviews support removal of the cyst, especially in severely symptomatic patients. However, debate remains for those patients with less severe symptoms or those for whom surgery carries high risks. Facet joint steroid injection with or without percutaneous cyst rupture is known to have some effect [10]. In studies, one-third to one-half of patients who received this conservative measure experienced remission, and although there was significant recurrence of cysts, repeated treatment resulted in another 50% success rate [1213]. Considering the significantly reduced complication of the procedure compared to spinal surgery, it is reasonable to consider facet joint injection as an attempt at cyst rupture in selected patient groups.
Although facet joint steroid injections under C-arm guidance are relatively simple procedures, rupturing the cyst could become technically demanding depending on the site of the cyst. This is true when the cyst is within the canal, abutting on the medial facet joint border, and has an incomplete communication with the joint. Facet joint injection may not deliver enough volume to rupture the cyst, and the needle may not reach the cyst without injury to the dura. Approach from inside the canal is necessary, which can be achieved by utilizing the epiduroscope.
Epiduroscopic procedures are minimally invasive procedures and can offer potential advantages for the management of spinal problems, such as direct visualization of spinal structures, which allows focused manipulations for mechanical adhesiolysis, irrigation of biomechanical irritators such as phospholipase A2 (PLA2) and tumor necrosis factor (TNF-α), and targeted injection of medications. Several clinical studies have also demonstrated that this novel technique can reduce pain and improve functional status through several therapeutic pathways as described above [1415]. Surgical facet joint cyst removal confronts the complicated question of whether to fuse or not, since the decompression may cause instability of the segment, which may lead to recurrence. Fusion will prevent this instability, which may nevertheless bring about the post back surgery syndrome. Needs are rising for minimally invasive techniques that will allow decompression with less destruction of the surrounding structures, thus maintaining stability, and endoscopic procedures are being tried and are reported to meet this need [16].
The epidural space of a facet joint cyst lesion may usually be filled once it produces radicular symptoms that necessitate intervention. The approach to the cyst itself and/or the targeting of the cyst with a laser could often be quite complicated or even impossible. In the case described here, we attempted to remove the facet cyst with laser ablation but it was not possible, because the direction of the laser beam was not in accordance with that of the epiduroscope. This is because the epiduroscopic laser device was originally designed for the ablation of the herniated disc which lies in the ventral aspect of the epidural space. Forceps removal and mechanical rupture should be attempted in cases of ablation failure. A manipulative epiduroscope tip, various viewing angles, and a side-hole laser may all assist with the targeting. Even with successful treatment, confirmation may also be uncertain solely with the epiduroscopic visualization, because of the packed up anatomy and the inflamed cyst being indistinguishable from adjacent structures. Injection of dye into the facet joint under fluoroscopy and confirmation of dye spread from the joint into the epidural space could be helpful.
In conclusion, intraspinal facet joint cysts can be successfully removed by epiduroscopy. A more navigable forceps, and a technically improved scope in which the laser could target the center of the view, may improve the results.
Go to : 
References
1. Trummer M, Flaschka G, Tillich M, Homann CN, Unger F, Eustacchio S. Diagnosis and surgical management of intraspinal synovial cysts: report of 19 cases. J Neurol Neurosurg Psychiatry. 2001; 70:74–77. PMID: 11118251.

2. Shah RV, Lutz GE. Lumbar intraspinal synovial cysts: conservative management and review of the world's literature. Spine J. 2003; 3:479–488. PMID: 14609693.

3. Boviatsis EJ, Stavrinou LC, Kouyialis AT, Gavra MM, Stavrinou PC, Themistokleous M, et al. Spinal synovial cysts: pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J. 2008; 17:831–837. PMID: 18389295.

4. Doyle AJ, Merrilees M. Synovial cysts of the lumbar facet joints in a symptomatic population: prevalence on magnetic resonance imaging. Spine (Phila Pa 1976). 2004; 29:874–878. PMID: 15082987.
5. Sachdev VP, Savitz MH, Hindi AI, Goldstein HB. Synovial cysts of the lumbar facet joint. Mt Sinai J Med. 1991; 58:125–128. PMID: 1857355.
6. Epstein NE. Lumbar synovial cysts: a review of diagnosis, surgical management, and outcome assessment. J Spinal Disord Tech. 2004; 17:321–325. PMID: 15280763.
7. Freidberg SR, Fellows T, Thomas CB, Mancall AC. Experience with symptomatic spinal epidural cysts. Neurosurgery. 1994; 34:989–993. PMID: 8084409.

8. Hsu KY, Zucherman JF, Shea WJ, Jeffrey RA. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine (Phila Pa 1976). 1995; 20:80–89. PMID: 7709284.
9. Epstein NE, Hollingsworth R. Synovial cyst of the cervical spine. J Spinal Disord. 1993; 6:182–185. PMID: 8504232.

10. Bydon M, Papadimitriou K, Witham T, Wolinsky JP, Sciubba D, Gokaslan Z, et al. Treatment of spinal synovial cysts. World Neurosurg. 2013; 79:375–380. PMID: 23022636.

11. Cecchi PC, Peltz MT, Rizzo P, Musumeci A, Pinna G, Schwarz A. Conservative treatment of an atlantoaxial degenerative articular cyst: case report. Spine J. 2008; 8:687–690. PMID: 17434808.

12. Allen TL, Tatli Y, Lutz GE. Fluoroscopic percutaneous lumbar zygapophyseal joint cyst rupture: a clinical outcome study. Spine J. 2009; 9:387–395. PMID: 18809358.

13. Martha JF, Swaim B, Wang DA, Kim DH, Hill J, Bode R, et al. Outcome of percutaneous rupture of lumbar synovial cysts: a case series of 101 patients. Spine J. 2009; 9:899–904. PMID: 19664971.

14. Manchikanti L, Boswell MV, Rivera JJ, Pampati VS, Damron KS, McManus CD, et al. A randomized, controlled trial of spinal endoscopic adhesiolysis in chronic refractory low back and lower extremity pain [ISRCTN 16558617]. BMC Anesthesiol. 2005; 5:10. PMID: 16000173.

15. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 2009; 12:361–378. PMID: 19305485.
16. Ishii K, Matsumoto M, Watanabe K, Nakamura M, Chiba K, Toyama Y. Endoscopic resection of cystic lesions in the lumbar spinal canal: a report of two cases. Minim Invasive Neurosurg. 2005; 48:240–243. PMID: 16172971.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download