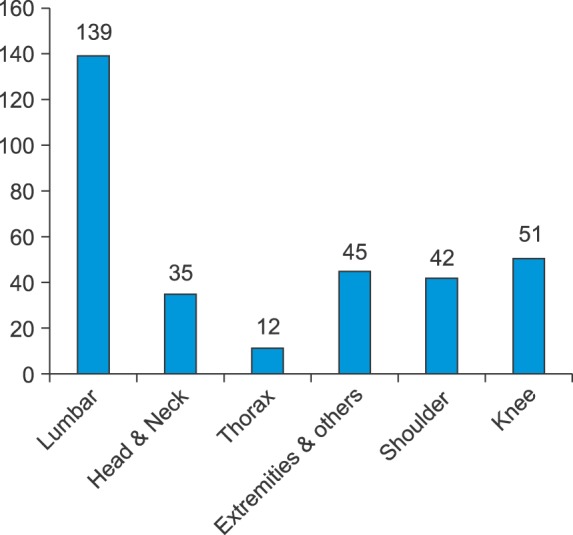
This is the first study analyzing the MDCs on pain management in Korea. These results indicate that a large number of pain specialists engage in medico-legal practice. Pain in the lumbar region made up a major proportion of MDCs and compensation costs. Infection, nerve injury, and diagnosis were the most major contents of MDCs. Only a small proportion of cases involved patient death or unconsciousness, but compensation costs were the highest.
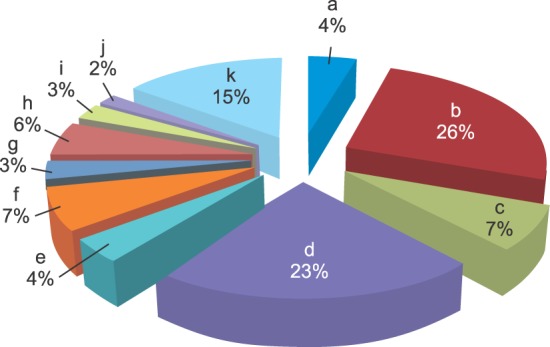
2. Classification of MDCs by contents and severity
1) Cases related to death, brain death, and/or unconsciousness
Fifteen cases were classified as being related to death, brain death, and unconsciousness. Pain in the lumbar and cervical regions was present in 10 and 5 cases, respectively. A definite causative assessment could not be achieved with our data. When all 15 cases were examined together, the importance of prompt intubation and resuscitation in patients who lost consciousness became apparent. Therefore, resuscitation training is essential for staff involved in neuro-axial blockade procedures performed for pain management.
·Sample cases
Example 1: A patient complained of dyspnea and became unconscious following a cervical epidural block procedure. The patient was transferred to a general hospital. Example 2: A patient died due to sepsis and pulmonary edema following fluoroscopy-guided lumbar epidural steroid injection (ESI). Example 3: A patient went into cardiac arrest following lumbar epidural block and was transferred to a general hospital.
2) Cases of mild infection
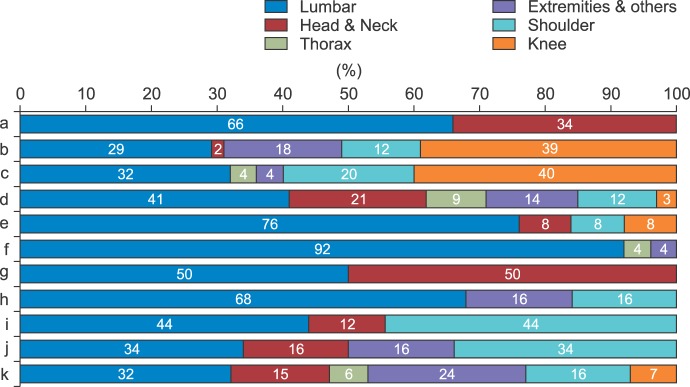
Mild infection was analyzed under the definition of infection related to a procedure that was controllable with conservative treatment. Total cases were 87. In cases involving a mild infection, the body part affected was the knee in 34 cases (39%), the lumbar in 25 cases (29%), the extremities (e.g., elbows, wrists, fingers, ankles, and toes) in 17 cases (18%), the shoulder in 10 cases (11%), and the head & neck in 1 case (1%). The majority of mild infection cases were transient reactive inflammatory reactions following intra-articular injection into the knee. Additionally, most cases were temporary, improved with conservative treatment, and did not result in any significant functional disabilities. Although mild infection is usually managed well with conservative treatment, under the circumstances of suspicious of malpractice, MDC can occur based on the different attitude of the physician and patient, lack of understanding, and misunderstanding of pathophysiology rather than the accident itself [
7].
·Sample cases
Example 1: A patient developed a local inflammatory reaction after a supra-scapular nerve block to relieve shoulder pain. Example 2: A patient developed septic arthritis of the lateral epicondyle following prolotherapy. Example 3: Bee venom (apitoxin) was injected into the ankle joint and caused transient synovitis.
3) Cases of severe infection
Severe infection is defined as an infection related to an injection procedure (e.g., nerve block, articular injection, and soft tissue injection) that was refractory to conservative management and required surgical intervention. There were 25 total cases. Among them, cases of severe infection were related to the knee in 10 cases (40%), the lumbar in 8 cases (32%), the shoulder in 5 cases (20%), the thorax in 1 case (4%), and the extremities in 1 case (4%).
Infection is a recognized complication of any invasive procedure. Analysis of the American Society of Anesthesiologists (ASA) Closed Claims database from 1970 to 1999 revealed that infection accounted for 13% of complications following procedures to treat chronic pain, making it one of the most common causes [
8]. In cases of severe infection, it is common for patients to have severe pain, hot flushes, and local tenderness, all of which are indicative of a severe infection. However, these symptoms may go unnoticed in elderly patients who cannot communicate effectively and in patients who do not accurately disclose their medical history with respect to the invasive procedures they have undergone. Therefore, it is unfair to blame pain physicians for the inevitable occurrence of a postprocedural infection. To protect themselves from MLCs, physicians should always obtain a thorough patient history of systemic disease and prior treatments, including invasive procedures. Additionally, infection risk is reduced by strict attention to aseptic technique. This includes the assiduous preparation of skin over the procedural target site and following established protocols for instrument handling. Disclosure should also be accompanied with quality control.
·Sample cases
Example 1: A patient was transferred to a general hospital after developing a post-procedural knee infection that required incision and drainage. Example 2: A patient allegedly developed an epidural abscess following a lumbar epidural steroid injection for sciatica. Example 3: Following trigger point injections (TPIs) in the lower back and buttock to treat sciatica, a patient developed an intra-muscular abscess. Example 4: A patient underwent nerve block and intra-articular injection to treat shoulder pain and developed a related intra-articular infection and a related ligament rupture.
4) Cases of body injury
These cases include nerve damage, muscle weakness and pneumothorax, which including temporary or permanent nerve damage related to pain procedure. Sensory disturbance and extremity weakness cases were also included.
There were 77 total cases consisting of 38 nerve damage cases, 31 for muscle weakness, and 8 cases of pneumothorax. Regions were related to the lumbar in 32 cases (41%), the head & neck in 16 cases (20%), the extremities in 11 cases (14%), the shoulder in 9 cases (11%), the thorax in 7 cases (9%), and the knee in 2 cases (2%). With regard to nerve injury and paralysis, physicians should consider the possibility of unusual anatomic structure, which may be concomitant with another disease (e.g., progressing nerve compression). With regard to pneumothorax, this complication commonly occurs with TPIs, especially to the cervical and thoracic regions, as found in a study conducted in the United States [
9]. The small needles used for TPI (25-gauge or smaller) bend easily when "fanning" injections are made, making the needle tract relatively uncontrollable. This can sometimes make multiple holes in the pleura, causing a pneumothorax that requires a chest tube. Pneumothorax is a common trigger for MLC [
10]. Using imaging systems (e.g., ultrasound or fluoroscopy) to help guide TPI could help protect both patient and physician [
11]. Thorough anatomical studies and related techniques could also be useful.
·Sample cases
Example 1: A patient developed cauda equina syndrome following lumbar epidural endoscopy. Example 2: A patient developed paraplegia related to lumbar epidural steroid injection. Example 3: A patient developed persistent ptosis following a stellate ganglion block. Example 4: A patient that underwent a nerve block for calf pain developed persistent muscle weakness in the extremities.
5) Cases of bleeding or hematoma
Bleeding or hematoma occurred in the lumbar in 10 cases (76%), the head & neck in 1 case (8%), the shoulder in 1 case (8%), and the knee in 1 case (8%). Anticoagulation therapy and daily aspirin therapy have become very common in Korea. Management of these medications before and after pain management procedures can be problematic because existing data does not answer all questions. It is also often difficult to check all laboratory values in a primary pain center. Discontinuing aspirin therapy has been associated with stroke and myocardial infarction. Patients with mechanical valves, or recent pulmonary emboli, or recently placed coronary stents are not good candidates for discontinuing anticoagulation therapy [
1213]. Though discontinuing platelet inhibitors is considered to be safer, the relative risks of bleeding and infarction should be discussed with their other physician. Coordination with the physician managing anticoagulant therapy is an important protective measure when pain physicians perform the interventional procedures. Immediate transfer to a general hospital would also be essential in reducing MLCs when symptoms reflecting an AE occurrence are suspected.
·Sample case
Example 1: A patient developed an epidural hematoma following a nerve block performed to treat persistent pain. Example 2: A patient developed bleeding associated with a vessel injury following a nerve block to treat shoulder pain.
6) Cases of fractures related to pain procedures
Most cases of fracture related to pain procedures occurred in the post-procedural period and were related to physical therapy (e.g., a manipulation causing vertebral compression fracture). Among the total 24 cases, 22 cases (92%) occurred in the lumbar, 1 case (4%) occurred in the thorax, and 1 case (4%) occurred in the extremities. Motor weakness following sympathetic blockade with local anesthetics is common and most episodes are transient. The duration depends on the local anesthetic and additives used. Therefore, patients should be educated on this phenomenon before the procedure. Transient syncope and rebound hypotension can occur during the recovery period, especially in older patients, which may result in patient falls [
14].
Although these episodes generally occur when the physician is not present, MDCs can occur simply because they happened in the hospital based on the obligations of doctors. Therefore, pain physicians should take care to monitor patients closely during the recovery period, making sure that nursing staff is present and all safety guards are in place.
·Sample cases
Example 1: A patient sustained a femur fracture after attempting to rise from his bed by himself. A fall occurred even though the patient had fully regained muscle power after a lumbar epidural steroid injection. Example 2: A patient developed a thoracic vertebral compression fracture that was related to physical back manipulation therapy.
7) Cases of headache following pain procedures
Patients complained of headaches following procedures to the lumbar (5 cases [50%]) and head & neck (5 cases [50%]). Headaches can occur following dural puncture and are generally resolved with conservative treatment. Still, MLCs can occur without outcome or prognosis. Individual anatomical variations such as ligamentum flavum discontinuity and anterior spinal cord vascular supply also could be a cause [
15]. Recent measurements of dural thickness have also demonstrated that the posterior dura varies in thickness, and that the thickness of the dura at a particular spinal level is not predictable within an individual or between individuals [
16]. Dural perforation in a thick area of dura may be less likely to lead to a CSF leak than a perforation in a thin area, and may explain the unpredictable consequences of a dural perforation [
17].
Idiopathic spontaneous intracranial hypotension also would be another causative origin, unrelated to procedure [
18]. Detailed description about the kind of needle used, the drugs administered, and the anatomical position of the needle are needed for physicians to protect against MDC.
·Sample cases
Example 1: A patient with a persistent headache needed hospitalization following cervical epidural steroid injection for upper arm radicular pain.
8) Cases related to skin burns
Most cases of skin burns were caused by application of a hot bag after a pain intervention procedure. Burns occurred in the lumbar in 13 cases (68%), in the shoulder in 3 cases (16%), and on the extremities in 3 cases (16%). Nerve blockades can cause numbness, desensitizing many patients to heat. Therefore, patients with nerve blocks are vulnerable to developing skin burns. Some patients with other medical conditions (e.g., diabetes, chronic steroid use, and anticoagulant use) may also have delicate skin that is desensitized and vulnerable to heat [
19].
·Sample cases
Example 1: A patient sustained skin burns on the back from application of a hot bag applied during the recovery period following lumbar epidural steroid injection. Example 2: A patient sustained a skin burn from improper adaptation of a grounding pad used during radiofrequency medial branch neurotomy of the lumbar spine. Example 3: A patient sustained a skin burn on a toe following digital nerve block performed for peripheral neuropathy.
9) Cases involving complications occurring in other medical departments
These cases include the MDCs claimed to be pain procedures, such as deterioration of pre-existed disease or other medical complications, even though causal relationship did not confirm on medical aspect. Complications related to other medical departments occurred following treatment related to the lumbar in 4 cases (44%), the shoulder in 4 cases (44%), and the head & neck in 1 case (11%). In most cases, patients did not notify of his/her past history to their own physicians. Even when there is no evidence in support of physician negligence, an MDC can occur. Therefore, it is essential for physicians to obtain the relevant medical history in a careful and efficient manner.
·Sample cases
Example 1: A patient had a myocardial infarction, which was treated with coronary angioplasty and stent placement. The patient claims that the myocardial infarction resulted from a sudden increase in blood pressure following lumbar epidural steroid injection. Example 2: A patient who underwent steroid injection for pain management had aggravation of an existing ophthalmic disease following treatment. However, the patient did not notify the ophthalmic disease to the physician before steroid treatment.
10) Cases involving a drug allergy
Most cases involving a drug allergy occurred because of an allergic reaction to a drug used in injection therapy. The lumbar was involved in 2 cases (33%), the shoulder was involved in 2 cases (33%), the head & neck was involved in 1 case (17%), and the extremities were involved in 1 case (17%).
An anaphylactic reaction, which is accompanied by severe hypotension, can be life-threatening if not immediately treated. Introducing additive drugs (e.g., hyaluronidase) into the epidural space can cause anaphylactic allergic reactions [
20]. Nevertheless, most clinical symptoms of allergic reactions are weak and patients often spontaneously recover without any significant complications. Anesthesiologists generally manage these types of situations, which explain the smaller number of MDCs in this category. Because allergic reactions always indicate a high risk, physicians need to use caution.
·Sample case
Example 1: A patient had an allergic reaction to additive drugs used in a lumbar epidural steroid injection.
11) Cases related to diagnosis
These MDCs that occurred are related to the misdiagnosis, delayed diagnosis, and aggravation of symptoms in pain management. The lumbar was involved in 16 cases (32%), the extremities were involved in 12 cases (24%), the shoulder was involved in 8 cases (16%), the head && neck was involved in 7 cases (14%), the knee was involved in 4 cases (8%), and the thorax was involved in 3 cases (6%).
These cases accounted for one third of all MDCs and are believed to originate from "pain management's distinctiveness." Pain can have various origins, often making it difficult for both physicians and patients to identify the source properly. It is not always possible to correctly diagnosis pain disorders, especially in patients with complex, concomitant disease. Therefore, a missed or delayed diagnosis is not enough to find fault in a pain physician. There are limitations for a primary pain physician in ruling out the whole origin of pain. Therefore, it is necessary for physicians to explain that "pain management distinctiveness" to the patient to prevent MDCs. The purpose of a nerve blockade is to not only provide pain relief but also confirm a source of pain. The diagnostic value of the procedure should be clearly communicated to the patient. The physician also has to explain that symptom aggravation may occur following the procedure, which may require additional examination or transfer to a general hospital.
·Sample cases
Example 1: A patient was transferred to a general hospital because of aggravation of radicular pain, even though the patient had undergone repetitive lumbar epidural steroid injections. Example 2: A patient with a rib fracture was misdiagnosed as having upper back pain. As a result, the patient received an intercostal nerve block. Example 3: A patient with varicose veins in the lower leg had a delay in diagnosis. The patient was treated with a nerve block under the diagnosis of lumbar radiculopathy. Example 4: A patient with knee pain insisted that symptoms worsened following interferential current therapy, a type of physical therapy.
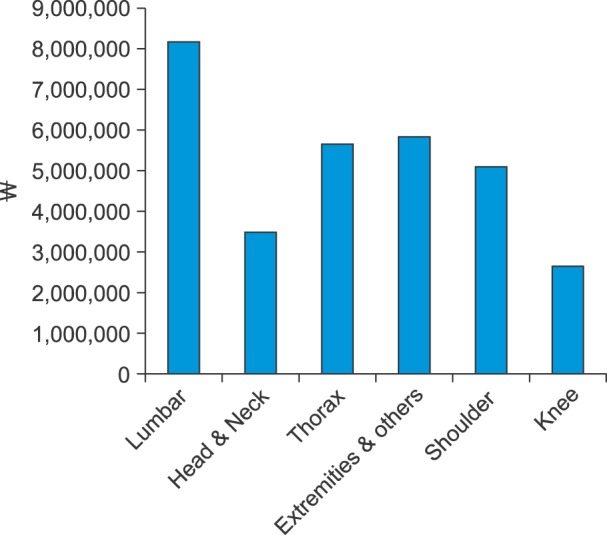
3. Average compensation costs
Average compensation costs by body part and cases' contents were calculated and are summarized in
Fig. 6 and
7. The highest average compensation cost was in cases involving the lumbar with 8,169,000 ± 8,254,743 Korean won. The lowest average compensation cost was in cases involving the knee with 2,674,000 ± 1,931,141 Korean won. The high cost of lumbar cases likely originates from a large amount of disease diversity and the introduction of new techniques that are more invasive than conventional blind, single-injection procedures. These new invasive procedures have the potential to cause severe functional disability from nerve injury, paralysis, and motor weakness. Interestingly, cases involving the knee occurred the second most often in frequency, but the compensation cost for each case was mercifully lower than that for cases involving the lumbar. Besides the lower incidence compare to lumbar, it is considered that the knee has a much simpler anatomical structure which has a high complexity and can result in severe disability from complications. Lower level of difficulty in injection technique in pain management in the knee region is considered to be another reason.
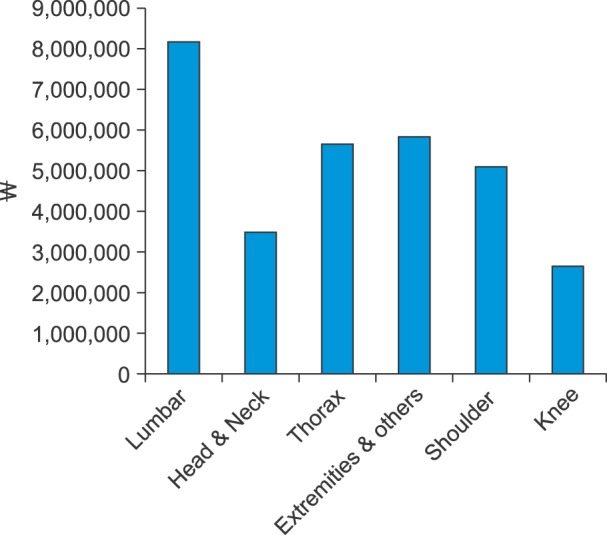 | Fig. 6Average compensation costs by the body part from 2010 to 2014. Costs presented in units of Korean "won".
|
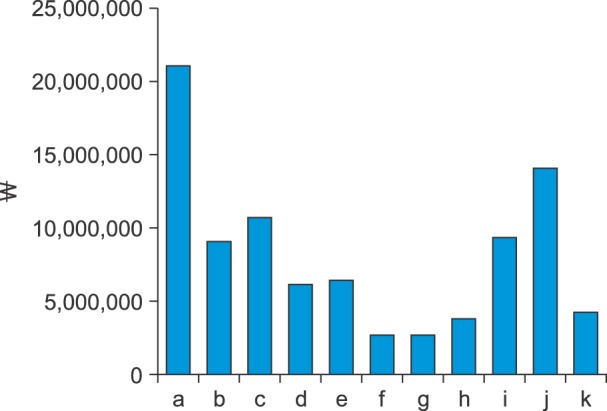
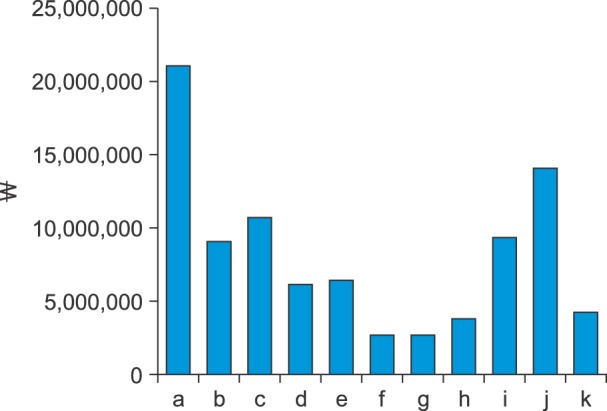 | Fig. 7Average compensation costs by medical dispute case content from 2010 to 2014. Costs presented in Korean "won". Data shown for cases involving death and/or unconsciousness (a), mild (b) and severe (c) procedurerelated infection, body injury (including nerve damage, muscle weakness, and pneumothorax; (d), bleeding or hematoma (e), procedure-related fracture (f), post-procedure headache (g), treatment-related skin burn (h), complications related to other medical departments (i), drug allergy (j), and diagnosis issues (k).
|
We also examined compensation costs by case content. The cost of cases that involved death and unconsciousness totaled 21,108,000 ± 20,361,781 Korean won, mostly because these had the worst outcomes. The total cost was 14,072,935 ± 2,530,514 Korean won for drug allergy cases, 10,672,000 ± 1,211,271 Korean won for severe infection cases, 9,374,000 ± 1,040,242 Korean won for other category cases, 9,081,000 ± 1,148,244 Korean won for mild infection cases, 6,443,000± 2,653,483 Korean won for bleeding or hematoma cases, 6,128,000 ± 7,820,630 Korean won for physical injury cases (includes nerve damage, muscle weakness and pneumothorax), 4,298,000 ± 2,709,162 Korean won for diagnosis-related cases, 3,829,060 ± 997,794 Korean won for skin burn cases, 2,652,500 ± 1,56,583 Korean won for headache cases, and 2,649,000 ± 1,474,783 Korean won for fracture cases.
The discrepancy between total compensation and MDCs' frequency is thought to reflect the likelihood of hospitalization, which has a high cost and is independent of complication severity. A patient wanting hospitalization could also be a contributor for the increasing cost. The number of cases related to headache (10 cases), other categories (9 cases), and drug allergy (6 cases) were small; hence, our estimates of absolute compensation cost may have limited accuracy.
Every physician is at a risk of malpractice owing to unexpected/unwanted results of treatment resulting from misdiagnosis or a minute mistake. In particular, clinically uncommon situations that bring unexpected struggles following casual management may occur, particularly when patients do not report distinct warning signs that they think may be minor. Recently, the MDCs began to rapidly increase in Korea. This may have resulted from the encouragement given to people to exercise their rights, new and easier access to medical information, relieved or transferred burden of proof in medical accidents, and lowered authority and/or ethics of medical doctors [
21].
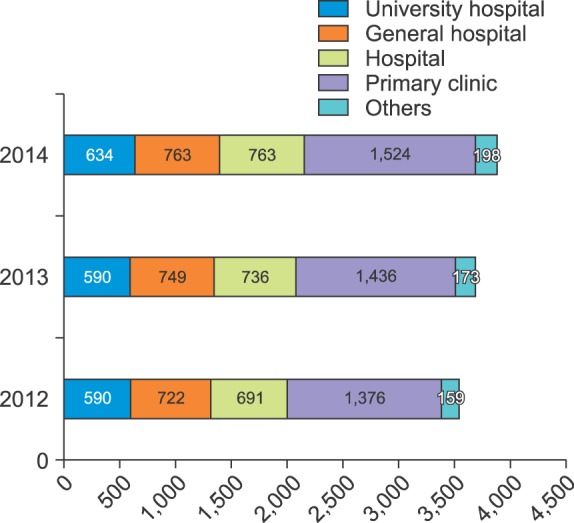
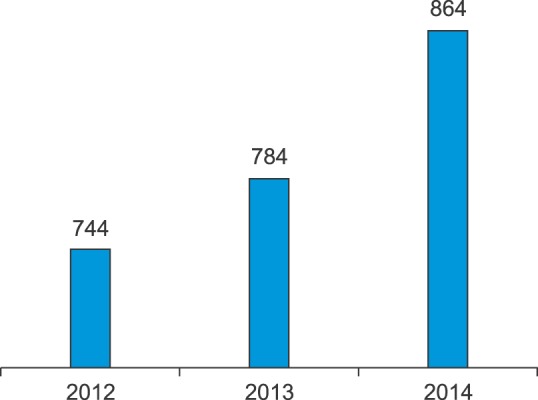
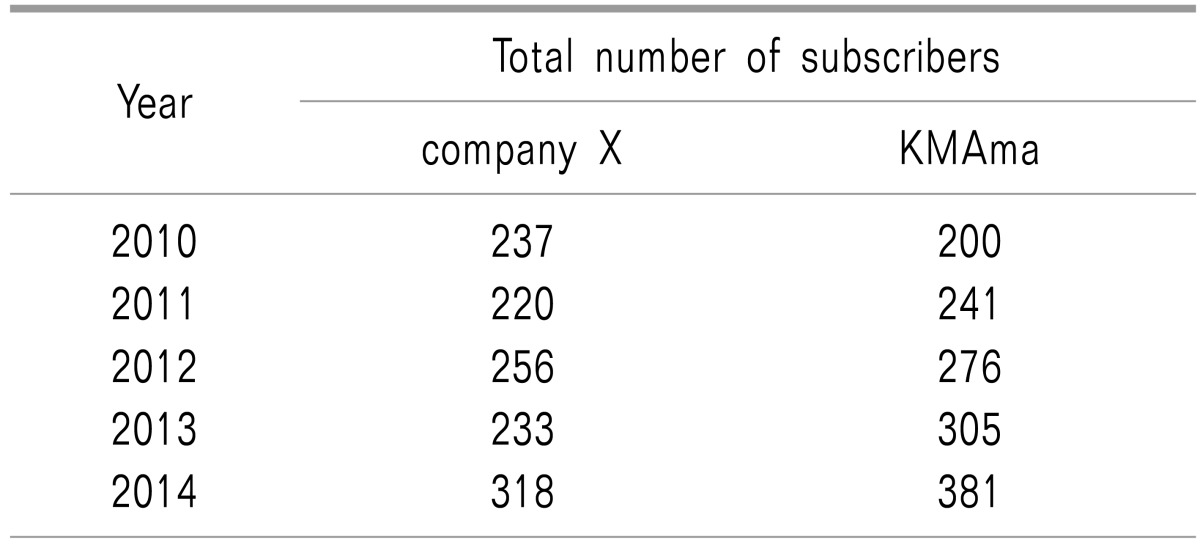
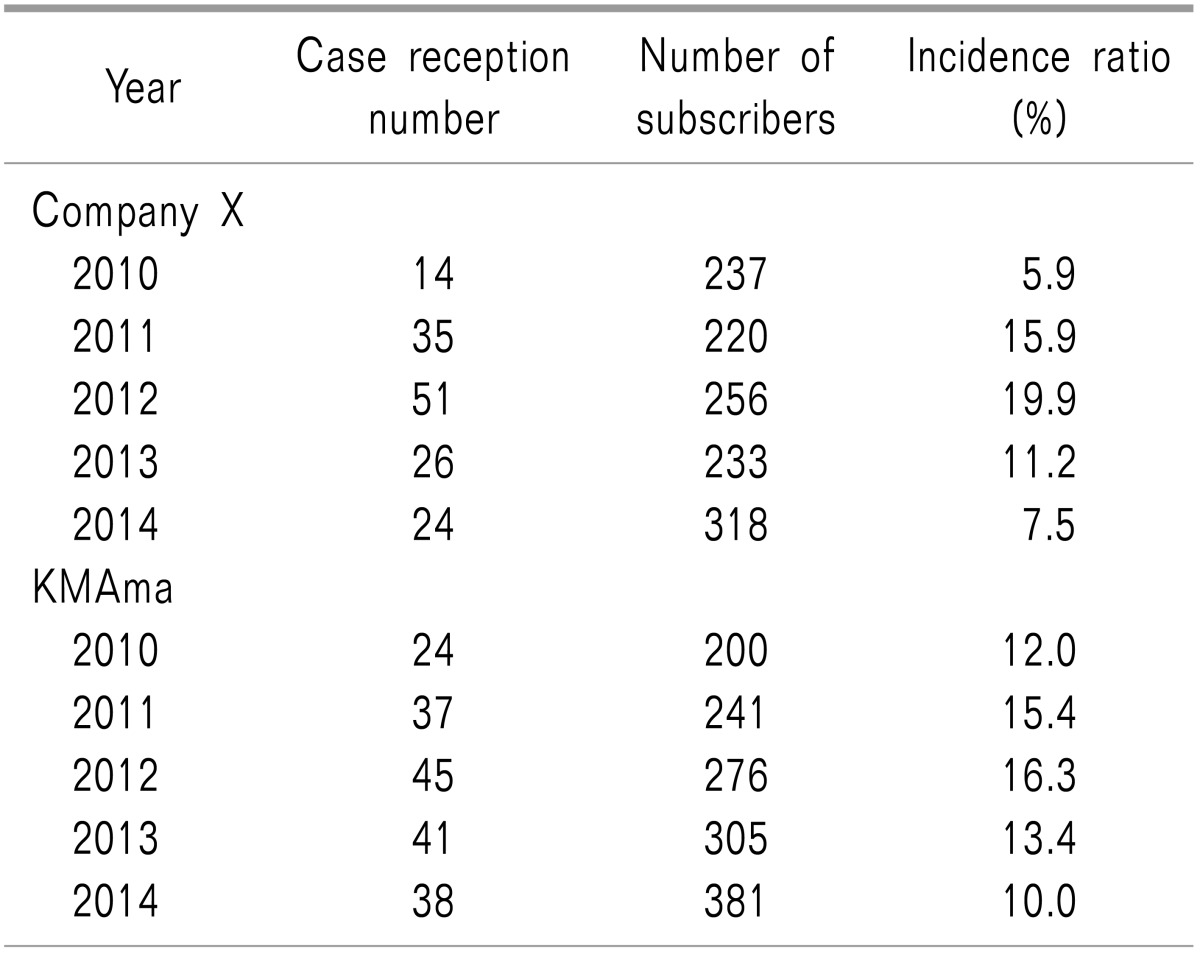
First, in Korea, the price of medical insurance, so-called "medical insurance fee," is multiplied by the Resource-Based Relative Value Scale (RBRVS) and a conversion factor. The RBRVS schema determines how much money medical providers need to pay. Factors like physician workload, medical supply costs, and MDCs costs are considered. However, MDCs cost is determined only using KMAma's data. As seen in this article, in Korea, many pain physicians also join private insurance companies, which exceed the number insured by KMAma (
Table 2 and 3). This current system does not completely reflect physician risk and can result in unreasonable pain procedure prices, which may lead to harming the patient with over-treatment and underestimating the value in pain procedure. Second, interventional treatment is invaluable in diagnosing and treating acute and chronic pain of various origins. Precise, selective, image-guided procedures performed by well-trained physicians can greatly benefit patients suffering from pain. However, in Korea, formal training for these procedures, particularly interventional techniques, only exists in board-certified residency programs for anesthesiology and pain management [
22]. Therefore, general physicians performing interventional pain management procedures should also have qualification standards, based on their specialty, to increase the likelihood of effective treatment. Third, a more systemic review of adverse events related to pain management is needed in Korea. We reviewed all case reports in the Korean Journal of Pain published between 2005 and 2014. There were 36 cases related to pain management complications or adverse events. Although they included contents related to pain procedures, including drug allergy and diagnosis issues [
232425], they only examined extremely rare cases for academic purposes. Therefore, these cases are not applicable to practical law issues affecting pain physicians. Additionally, pain specialists are offered only minimal guidance with respect to these activities, whether infrequent or frequent, in their pain practice. Although some recommendations regarding MDCs do exist for pain physicians [
1], more systemic guidelines for interventional pain treatments and strategies for reducing adverse events and to protect pain physicians in Korea from legal recourse.
This report has some limitations, such as the data provided only included limited information (e.g., age, sex, medical history, procedure description, and drug names), the causal relationship between the procedure and the adverse event could not be determined, not based on medical evidence. A consideration of the characteristics of the MDCs in Korea, which wishes cases not to be common, is also needed. Thus, incidence of complications cannot be determined because of a lack of a denominator for all adverse outcomes in Korea. Data of this report requires replication with a national sample because members of the KPS may not be representative of pain specialists nationally. Further investigations of a larger sample are needed in consideration of different practice patterns among subspecialists. Collaborative efforts between the various professional pain societies may offer an effective opportunity for accessing practice data in Korea.
Additionally, a closer review of case law trends may also provide valuable data for this evolving field. Despite of the limitations of our study, these results suggest the need for further research in forensic pain medicine, which is, indeed, a much more common practice than we expected.
Finally, we reviewed MDCs and classified reports that occurred within the past five years in Korea. For pain physicians, MDCs only have limited information available because of many barriers. However, we hope our report will be a cornerstone for helping pain physicians better understand MDCs and will encourage the creation of a more systematic set of guidelines and databases for interventional pain management in Korea. All pain physicians have the duty to exercise care and skill in both treating and diagnosing acute or chronic pain. Physicians should take care when choosing treatments and when giving advice and information to patients for making treatment decisions, based on individual patients, different warning signs and symptoms.
The ability to recognize and interpret this diversity, and subsequently act appropriately, is the cardinal reason why the board of anesthesiology and pain medicine maintains that these procedures should only be performed by properly trained physicians. Patient safety does not depend upon the elegant insertion of a needle, but in understanding what happens at its tip [
26].




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download