Abstract
Herpes zoster (HZ) is a transient disease caused by the reactivation of latent varicella zoster virus (VZV) in spinal or cranial sensory ganglia. It is characterized by a painful rash in the affected dermatome. Postherpetic neuralgia (PHN) is the most troublesome side effect associated with HZ. However, PHN is often resistant to current analgesic treatments such as antidepressants, anticonvulsants, opioids, and topical agents including lidocaine patches and capsaicin cream and can persist for several years. The risk factors for reactivation of HZ include advanced age and compromised cell-mediated immunity (CMI). Early diagnosis and treatment with antiviral agents plus intervention treatments is believed to shorten the duration and severity of acute HZ and reduce the risk of PHN. Prophylactic vaccination against VZV can be the best option to prevent or reduce the incidence of HZ and PHN. This review focuses on the pathophysiology, clinical features, and management of HZ and PHN, as well as the efficacy of the HZ vaccine.
Go to : 
Herpes zoster (HZ) is caused by reactivation of latent varicella zoster virus (VZV) in craniospinal sensory neurons and is characterized by a painful erythematous rash in the affected dermatome. Approximately 20%-30% of people will have HZ during their lifetime. The incidence of HZ increases when cell-mediated immunity (CMI) against VZV decreases due to aging or immunosuppressive disorders or medical treatments. Postherpetic neuralgia (PHN), which can last several years, is the most common side effect associated with HZ [12]. The frequency of PHN has been reported to be from 10% to 34% depending on its definition [12]. If PHN is defined as persistent pain three months after the onset of the HZ rash, the incidence of PHN is 10% to 20% [23]. The quality of life of patients experienced by patients with PHN can be negatively affected not only by the pain, but also by comorbid conditions such as fatigue and insomnia, and decreased social activities [45]. This review focuses on the pathophysiology, clinical features, and management of HZ and PHN, as well as the efficacy of the HZ vaccine.
Go to : 
After resolution of the primary infection with VZV, the virus remains latent in the spinal dorsal root ganglia (DRG) and cranial sensory ganglia. Declines in CMI against VZV may result in a higher occurrence of HZ and PHN. When CMI against VZV decreases, the virus replicates in the spinal DRG and cranial sensory ganglia and, subsequently, spreads along the peripheral nerves to the skin, leading to the painful erythematous rash in the affected dermatome [456].
The pathophysiology of PHN is poorly understood. However, it is certain that HZ affects the central and peripheral nervous systems, which can subsequently lead to the occurrence of PHN. Two main processes play roles in the development of PHN: sensitization and deafferentation [78]. After resolution of the primary infection of VZV, replication of latent VZV in the sensory ganglia leads to inflammatory neural damage, resulting in acute zoster pain and PHN. Sometimes motor paresis may occur due to the spread of infection and inflammation from the dorsal horn to the anterior horn [9]. During the course of HZ, both the peripheral and central nervous systems can be injured. In skin biopsies taken from patients with PHN, severe depletion of epidermal free nerve endings was found in the involved areas [1011]. In addition, in an autopsy study of the spinal nerves of patients who had experienced HZ, atrophy of the DRG was found only in the patients with PHN [12].
Previous research found increases in the subtype of voltage-gated sodium channels [13], alteration of voltage-gated potassium channels, and increases in transient receptor potential vanilloid 1 (TRPV1) in animal studies of a neuropathic pain model [14]. In addition, the loss of γ-aminobutyric acid (GABA) inhibitory neurons in the DRG after nerve injury causes loss of descending inhibition, leading to excessive reaction of nociceptive neurons of the spinal DRG [15]. The inflammatory mediators released from injured tissue, including substance P, bradykinin, histamine, cytokines, and ions (K+, H+) activate peripheral nociceptors directly by lowering the threshold of nociceptors, leading to peripheral sensitization [1617]. These changes also increase the ectopic discharge rate of C-fiber nociceptors. Thus, repetitive discharge of C-fibers can lead to a prolonged response of neurons in the DRG, which contributes to central sensitization. Therefore, sensitization of the peripheral and/or central nervous systems produces spontaneous pain, allodynia, and hyperalgesia [81618].
The allodynia and sensory loss in the affected dermatomes are associated with deafferentation, which results in dorsal horn reorganization [8]. The decreased number of C-fibers of the peripheral nerves, in combination with deafferentation, induces sprouting of Aβ-fibers, which normally transmit innocuous touch and pressure. Aβ-fiber rewiring in the DRG, which connects with the pain-transmitting spinothalamic tracts, produces dynamic and tactile allodynia [19].
Go to : 
HZ is characterized by unilateral painful vesicles in the affected sensory ganglion. The pain from HZ is described as burning, throbbing, paresthesia, dysesthesia, and itching. The most commonly affected site was found to be the thoracic region, followed by the ophthalmic branch of the trigeminal nerve [2021].
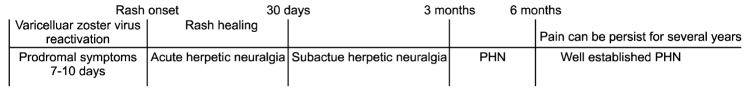
Seventy-five percent of patients with HZ experience prodromal symptoms including pain, general malaise, fever, and headache, which usually begin a few days before the rash develops. Although many clinicians have tried to distinguish acute herpetic neuralgia from chronic herpetic neuralgia, there is no definite consensus on the definition of PHN. However, from the recent studies, it appears valid to define three phases of pain following HZ: (1) acute herpetic neuralgia, defined as pain that occurs within a month after the onset of rash; (2) subacute herpetic neuralgia, defined as pain that occurs from the acute phase of HZ to the chronic phase of PHN; and (3) PHN, defined as pain that persists beyond three months after rash appearance. It was found that PHN that continues six months after the onset of rash is more likely to be obstinately persistent for several years [1921]. Therefore, such pain can be considered "well-established" PHN (Fig. 1).
The well-defined risk factors for PHN in patients with HZ include older age, the presence of prodromal pain, the extent and severity of rash, and the severity of acute HZ pain [22]. An age older than 50 and a visual analogue scale (VAS) score over 5/10 are predictive of persistent pain at three months after the appearance of HZ despite early treatment with antiviral medications. Other less replicated risk factors for PHN include female gender, location in the ophthalmic branch of the trigeminal nerve, greater neurosensory disturbance, and psychosocial distress [2324].
Diagnostic laboratory tests for HZ include polymerase chain reaction (PCR) assay, skin biopsy, immunofluorescence assay, and viral isolation. These tests are useful for patients with atypical lesions such as herpes simplex, as well as those with contact dermatitis and rash. But the results of these tests differ in terms of sensitivity, specificity, and time to obtain sample. Therefore, these tests have limitations for application in the clinical management of HZ [25].
Go to : 
The primary goals of management of HZ are to inhibit ongoing viral replication, alleviate pain, and prevent complications such as PHN. Treatments for HZ include antiviral agents, analgesics, corticosteroids, and neural blockade.
Antiviral agents such as acyclovir, famciclovir, and valacyclovir have been shown to reduce acute HZ pain, speed lesion healing, and prevent the occurrence of PHN. In clinical trials, the use of antiviral agents is one of the most important treatments of HZ. Because antiviral agents have a favorable risk-benefit ratio and are well tolerated, clinicians should prescribe them for patients with HZ as soon as possible. Based on the results of clinical trials, antiviral therapy should be initiated within 72 hours of the skin eruption [262728]. However, in clinical practice, antiviral treatment is often not initiated within three days after rash onset, and the viral replication may persist beyond three days from the skin eruption. Therefore, antiviral treatment may have benefits for immunocompromised patients, those with disseminated HZ, those who have moderate or severe pain or rash, those with involvement of non-truncal dermatomes (e.g., the face), and patients with neurological complications, even when it is initiated beyond 72 hours of rash onset [2528].
The antiviral agents can be classified into two types, according to their reliance on viral phosphorylation to be activated. Acyclovir, famciclovir, and valacyclovir are nucleoside analogues, which are phosphorylated to the active triphosphate forms that block viral DNA polymerase, leading to a decrease of replication of human herpes viruses. In general, patient compliance with valacyclovir and famciclovir is significantly improved compared to that with acyclovir, because valacyclovir and famciclovir are more bioavailable than acyclovir. Thus they require less frequent dosing than acyclovir [27].
Foscarnet, vidarabine, and cidofovir, which are not dependent on viral phosphorylation, noncompetitively block viral DNA polymerase. In clinical trials, foscarnet is effective to treat viral infection in patients who have resistance to acyclovir [29].
Treatment with corticosteroids is often used for HZ but has no beneficial effects on PHN. When combined with antiviral therapy, oral or intravenous administration of corticosteroids significantly attenuates pain from HZ, compared with treatment with antiviral therapy alone, but is not effective for the prevention of PHN [30]. The use of corticosteroids is associated with numerous side effects. Therefore clinicians may consider corticosteroids in combination with antiviral treatment for HZ patients who have severe symptoms without contraindications to the therapy [2830].
Antiviral treatment can reduce the acute pain from HZ, but most patients will require analgesics. The effective relief of this pain may reduce the risk of progression to PHN. Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can be prescribed, but there are no studies that have investigated the analgesic effects of NSAIDs on pain from HZ. Opioids have been shown to be effective in decreasing acute HZ pain [31]. In addition, adjuvant analgesics such as antidepressants and anticonvulsants are effective to reduce acute pain from HZ [28].
Interventional treatments including sympathetic blockade and neuraxial blockade have been used for the management of pain caused by HZ and the prevention of the development of PHN. However few randomized control trials (RCTs) on this subject have been conducted. Recently, from a RCT conducted in 2006, it was shown that a single epidural injection of 80 mg methylprednisolone acetate plus bupivacaine significantly reduced acute pain from HZ, but was not effective for the prevention of PHN, compared to conventional therapy with oral antivirals and analgesics [32]. However, in another study, epidural administration of bupivacaine plus methylprednisolone was significantly effective in reducing the incidence of PHN, compared to intravenous administration of acyclovir and prednisolone [33]. From a recent systemic review on the effect of intervention on HZ in general, evidence for epidural administration of local anesthetics plus steroids for the treatment of acute pain from HZ and the prevention of PHN appears to be strong [34]. Within two months of the development of HZ, epidural administration of local anesthetics plus steroids may prevent the incidence of PHN [34]. Paravertebral block (PVB) produces unilateral segmental block including the spinal nerve dorsal ramus, communicants, and the sympathetic chain. PVB is easier with a favorable side effect profile, but has similar analgesic efficacy, compared to epidural block [35]. In recent clinical trials, it was found that PVB with local anesthetics plus steroids is effective for relief of acute herpetic pain and prevention of the incidence of PHN [3637].
Sympathetic nerve block is often used for HZ patients. In a recent RCT in 2012, early sympathetic nerve block for facial HZ, in combination with antiviral agents, was found to provide significant reduction of the severity and duration of pain and to decrease the incidence of the development of PHN [38]. RCTs for evaluating the role of selective sympathetic nerve blocks in patients with HZ should be conducted in the future.
Go to : 
PHN is a type of chronic neuropathic pain. Therefore, although NSAIDs or acetaminophen are not effective, agents for the treatment of neuropathic pain are generally useful for the treatment of PHN. However, PHN is often resistant to the current pharmacologic treatments. A multimodal analgesic treatment strategy should be provided to balance the efficacy and tolerability of the medication regimen [39].
Tricyclic antidepressants (TCAs) such as tertiary amines (amitriptyline) and the secondary amines (nortriptyline and desipramine) have shown efficacy in decreasing the chronic pain of PHN and should be considered in patients when conventional analgesic therapy is not effective to control pain from HZ. It has been demonstrated that TCAs exert analgesic effects by prohibiting the reuptake of serotonin and norepinephrine at presynaptic nerve terminals and blocking sodium channels. In the clinical trials and meta-analysis of the TCAs, their number needed to treat (NNT) in the management of PHN was 2.1-2.6 [39]. However, the use of TCAs often induces a number of anticholinergic side effects including dry mouth, gastrointestinal discomfort, constipation, urinary retention, nausea, vomiting, blurred vision, confusion, and orthostatic hypotension. It also causes fatal cardiac dysrhythmias such as QT prolongation, torsades de pointes, and sudden cardiac arrest in patients with conduction abnormalities [40]. Therefore, clinicians should review a baseline electrocardiogram before initiating treatment with TCAs in elderly patients and patients with a history of cardiovascular disease or hypokalemia. These adverse effects are less pronounced at low doses of TCAs. Accordingly, TCA medication should be started at a low dose of 10 mg at bedtime titrated gradually every week to a target dose of 50-100 mg/day. Since nortriptyline and desipramine appear to be better tolerated compared to amtriptyline, they should be considered for elderly patients [28].
Duloxetine and venlafaxine are selective serotonin and norepinephrine reuptake inhibitors (SNRIs). SNRIs can be also used for the treatment of acute pain from HZ and PHN because these agents have proven analgesic efficacy in patients with painful neuropathic disorders. Clinically, SNRIs may be better tolerated than TCAs because of their favorable side effect profiles [41].
Numerous anticonvulsants have been tried to treat neuropathic pain disorders including trigeminal neuralgia and PHN. The second-generation anticonvulsant drugs, including pregabalin and gabapentin, are safe and well tolerated, compared to the first-generation anticonvulsants, such as carbamazepine and valproic acid. The exact mechanism of their analgesic action remains unknown. Both pregabalin and gabapentin work at the same receptor. They act at the α2δ subunits of voltage-gated calcium channels, with a consequent reduction in the release of excitatory neurotransmitters including glutamate. These drugs are not metabolized in the liver and are excreted unchanged in the urine. Therefore, dosage should be adjusted based on the renal function. In a clinical trial, gabapentin efficacy was demonstrated with an NNT of 2.8 for moderate improvement in PHN [42]. The dosage of gabapentin should be divided into 3 or 4 doses per day. Patients who received gabapentin reported somnolence, dizziness, peripheral edema, and ataxia. These side effects are generally short-lived, but they sometimes require dose adjustment [42]. Pregabalin is reported to have a distinct pharmacokinetic advantage over gabapentin due to its predictable and linear pharmacokinetic profile. The analgesic efficacy and adverse effect profiles of pregabalin are comparable to gabapentin, but at much lower doses. Therefore, titration of pregabalin to the therapeutic dose range is more rapid [43]. Pregabalin can be given in two divided doses per day, offering greater convenience than gabapentin [4344].
Historically, the role of opioids in the management of neuropathic pain is debatable. Recently, however, many clinical studies have demonstrated that the use of opioids is effective to ameliorate neuropathic pain including PHN [3945]. In a crossover RCT in 2002, it was demonstrated that opioids and TCAs significantly decreased pain in patients with PHN compared to placebo (38.2%, 31.9%, and 11.2% pain relief, respectively); the NNT for opioids was 2.8 and 3.7 for TCAs [46]. Opioid therapy is associated with several adverse effects including nausea, pruritus, dizziness, sedation, and constipation. In general, these side effects are short-lived except for constipation. Therefore, when prescribing opioids, constipation prophylaxis should be considered.
Tramadol, a synthetic 4-phenyl-piperidine analogue of codeine, acts as a µ-opioid receptor agonist and a serotonin and norepinephrine reuptake inhibitor. Thus, it has properties of an opioid and a TCA. In a 2003 RCT, tramadol was shown to significantly improve quality of life and relieve pain in patients with PHN, and the NNT for tramadol was 4.8 [47]. Adverse effects of tramadol included nausea, dizziness, constipation, somnolence, and headache. Concomitant use with selective serotonin reuptake inhibitors or selective monoamine oxidase inhibitor TCAs can lead to serotonin syndrome or seizures [28].
The 5% lidocaine patch produces local analgesia to the affected area without causing local anesthesia. In addition, the patch provides protection from mechanical irritation of the affected skin. In clinical trials, the lidocaine patch for PHN provided a significant reduction of pain and allodynia [4849]. Topical application of a low concentration of lidocaine is associated with minimal systemic absorption of the medication, resulting in a good safety and tolerability profile. A small portion of patients who received treatment with the lidocaine patch reported mild to moderate localized skin reactions. Within two to three weeks of initiation of lidocaine patch treatment, pain-relieving efficacy can be observed, and the treatment can provide long-term pain relief in patients with PHN [49].
Capsaicin is an alkaloid extracted from hot chili peppers. This acts as an agonist for the TRPV1 of afferent nociceptor terminals. In addition, repeated use of capsaicin causes depletion of substance P and other neuropeptides from nociceptive fibers (unmyelinated C-fibers), resulting in analgesia. The NNT for capsaicin is 3.2 [50]. Capsaicin treatment is often limited by the irritating and burning sensations it induces, especially in PHN patients with severe allodynia. However, these patients would be most likely to benefit from the use of capsaicin. Therefore, it is recommended to apply capsaicin on the affected skin following pretreatment with local anesthetics [28].
The interventional treatments including epidural block, intrathecal injection, and sympathetic nerve block have limited evidence of effective treatment of PHN. Epidural block with local anesthetics and steroids is not effective in providing long-term pain relief in patients with PHN [34]. Intrathecal administration of steroids appears to have beneficial effects in patients with PHN [51]. However, this technique increases the risk of development of adhesive arachnoiditis. Sympathetic nerve block has beneficial effects in patients with acute HZ but does not appear to provide long-term pain relief in PHN patients [34]. Longlasting pain relief by peripheral nerve block using local anesthetics has been reported, but the quality of the evidence is limited [52].
SCS has been used for the management of chronic neuropathic pain disorders [53]. Recently, in a clinical series, the effects of SCS in 28 patients with PHN and 4 patients with HZ were prospectively investigated over a median period of 29 (quartiles 9-39) months. SCS provided significant long-term pain relief in 82% of PHN patients. In addition, in the 4 patients with HZ, pain was resolved during a period of 2.5 months after SCS treatment [54]. These findings suggest that SCS can be a treatment option for the management of intractable pain from PHN and reduce the incidence of PHN.
Go to : 
Clinically significant replication of latent VZV in the spinal or cranial sensory ganglia occurs when VZV-specific CMI decreases below a critical threshold. In a large, multicenter, RCT involving approximately 38,000 healthy adults aged 60 years or older, vaccination with live attenuated VZV reduced the incidence of HZ by 51.3%, the burden of illness from HZ by 61.1%, and the risk of PHN by 66.5% [55]. The side effects of the vaccine are minor, including erythema, pain, and an itching sensation at the injection site, and fever [55]. These findings suggest that vaccination against VZV can be the first line for the prevention of HZ and PHN. This live attenuated vaccine is contraindicated in pregnant women and immunocompromised individuals.
Go to : 
The incidence of HZ increases with age. As the general population ages, the number of patients with HZ and PHN may increase substantially in the future.
PHN is the most common complication associated with HZ. It is often very difficult to treat. Early diagnosis of HZ and treatment with antiviral agents plus interventional treatments can shorten the duration and intensity of pain from HZ and prevent the incidence of PHN. In addition, prophylactic vaccination against HZV can be the best option to prevent or reduce the incidence of HZ and PHN.
Go to : 
References
1. Gauthier A, Breuer J, Carrington D, Martin M, Rémy V. Epidemiology and cost of herpes zoster and post-herpetic neuralgia in the United Kingdom. Epidemiol Infect. 2009; 137:38–47. PMID: 18466661.

2. Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007; 82:1341–1349. PMID: 17976353.

3. Arvin A. Aging, immunity, and the varicella-zoster virus. N Engl J Med. 2005; 352:2266–2267. PMID: 15930416.

4. Thyregod HG, Rowbotham MC, Peters M, Possehn J, Berro M, Petersen KL. Natural history of pain following herpes zoster. Pain. 2007; 128:148–156. PMID: 17070998.

5. Yawn BP, Gilden D. The global epidemiology of herpes zoster. Neurology. 2013; 81:928–930. PMID: 23999562.

6. Panlilio LM, Christo PJ, Raja SN. Current management of postherpetic neuralgia. Neurologist. 2002; 8:339–350. PMID: 12801435.

7. Fields HL, Rowbotham M, Baron R. Postherpetic neuralgia: irritable nociceptors and deafferentation. Neurobiol Dis. 1998; 5:209–227. PMID: 9848092.

8. Baron R. Mechanisms of postherpetic neuralgia--we are hot on the scent. Pain. 2008; 140:395–396. PMID: 19004555.
9. Chernev I, Dado D. Segmental zoster abdominal paresis (zoster pseudohernia): a review of the literature. PM R. 2013; 5:786–790. PMID: 24054853.

10. Oaklander AL. The density of remaining nerve endings in human skin with and without postherpetic neuralgia after shingles. Pain. 2001; 92:139–145. PMID: 11323135.

11. Truini A, Galeotti F, Haanpaa M, Zucchi R, Albanesi A, Biasiotta A, et al. Pathophysiology of pain in postherpetic neuralgia: a clinical and neurophysiological study. Pain. 2008; 140:405–410. PMID: 18954941.

12. Watson CP, Watt VR, Chipman M, Birkett N, Evans RJ. The prognosis with postherpetic neuralgia. Pain. 1991; 46:195–199. PMID: 1749643.

13. Garry EM, Delaney A, Anderson HA, Sirinathsinghji EC, Clapp RH, Martin WJ, et al. Varicella zoster virus induces neuropathic changes in rat dorsal root ganglia and behavioral reflex sensitisation that is attenuated by gabapentin or sodium channel blocking drugs. Pain. 2005; 118:97–111. PMID: 16213091.

14. Premkumar LS. Targeting TRPV1 as an alternative approach to narcotic analgesics to treat chronic pain conditions. AAPS J. 2010; 12:361–370. PMID: 20440589.

15. Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010; 9:807–819. PMID: 20650402.

16. Kidd BL, Urban LA. Mechanisms of inflammatory pain. Br J Anaesth. 2001; 87:3–11. PMID: 11460811.

17. Meller ST, Gebhart GF. A critical review of the afferent pathways and the potential chemical mediators involved in cardiac pain. Neuroscience. 1992; 48:501–524. PMID: 1351270.

18. Mannion RJ, Costigan M, Decosterd I, Amaya F, Ma QP, Holstege JC, et al. Neurotrophins: peripherally and centrally acting modulators of tactile stimulus-induced inflammatory pain hypersensitivity. Proc Natl Acad Sci U S A. 1999; 96:9385–9390. PMID: 10430952.

19. Dworkin RH, Gnann JW Jr, Oaklander AL, Raja SN, Schmader KE, Whitley RJ. Diagnosis and assessment of pain associated with herpes zoster and postherpetic neuralgia. J Pain. 2008; 9:S37–S44. PMID: 18166464.

20. Nahm FS, Kim SH, Kim HS, Shin JW, Yoo SH, Yoon MH, et al. Survey on the treatment of postherpetic neuralgia in Korea; multicenter study of 1,414 patients. Korean J Pain. 2013; 26:21–26. PMID: 23342203.

21. Arani RB, Soong SJ, Weiss HL, Wood MJ, Fiddian PA, Gnann JW, et al. Phase specific analysis of herpes zoster associated pain data: a new statistical approach. Stat Med. 2001; 20:2429–2439. PMID: 11512133.

22. Coen PG, Scott F, Leedham-Green M, Nia T, Jamil A, Johnson RW, et al. Predicting and preventing post-herpetic neuralgia: are current risk factors useful in clinical practice? Eur J Pain. 2006; 10:695–700. PMID: 16427792.

23. Jung BF, Johnson RW, Griffin DR, Dworkin RH. Risk factors for postherpetic neuralgia in patients with herpes zoster. Neurology. 2004; 62:1545–1551. PMID: 15136679.

24. Volpi A, Gatti A, Pica F, Bellino S, Marsella LT, Sabato AF. Clinical and psychosocial correlates of post-herpetic neuralgia. J Med Virol. 2008; 80:1646–1652. PMID: 18649332.

25. Espy MJ, Teo R, Ross TK, Svien KA, Wold AD, Uhl JR, et al. Diagnosis of varicella-zoster virus infections in the clinical laboratory by LightCycler PCR. J Clin Microbiol. 2000; 38:3187–3189. PMID: 10970354.

26. Shafran SD, Tyring SK, Ashton R, Decroix J, Forszpaniak C, Wade A, et al. Once, twice, or three times daily famciclovir compared with aciclovir for the oral treatment of herpes zoster in immunocompetent adults: a randomized, multicenter, double-blind clinical trial. J Clin Virol. 2004; 29:248–253. PMID: 15018852.

27. Shen MC, Lin HH, Lee SS, Chen YS, Chiang PC, Liu YC. Double-blind, randomized, acyclovir-controlled, parallel-group trial comparing the safety and efficacy of famciclovir and acyclovir in patients with uncomplicated herpes zoster. J Microbiol Immunol Infect. 2004; 37:75–81. PMID: 15181487.
28. Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc. 2009; 84:274–280. PMID: 19252116.

29. De Clercq E. Selective anti-herpesvirus agents. Antivir Chem Chemother. 2013; 23:93–101. PMID: 23343513.

30. Whitley RJ, Weiss H, Gnann JW Jr, Tyring S, Mertz GJ, Pappas PG, et al. Acyclovir with and without prednisone for the treatment of herpes zoster. A randomized, placebo-controlled trial. The National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. Ann Intern Med. 1996; 125:376–383. PMID: 8702088.

31. Dworkin RH, Barbano RL, Tyring SK, Betts RF, McDermott MP, Pennella-Vaughan J, et al. A randomized, placebo-controlled trial of oxycodone and of gabapentin for acute pain in herpes zoster. Pain. 2009; 142:209–217. PMID: 19195785.

32. van Wijck AJ, Opstelten W, Moons KG, van Essen GA, Stolker RJ, Kalkman CJ, et al. The PINE study of epidural steroids and local anaesthetics to prevent postherpetic neuralgia: a randomised controlled trial. Lancet. 2006; 367:219–224. PMID: 16427490.

33. Pasqualucci A, Pasqualucci V, Galla F, De Angelis V, Marzocchi V, Colussi R, et al. Prevention of post-herpetic neuralgia: acyclovir and prednisolone versus epidural local anesthetic and methylprednisolone. Acta Anaesthesiol Scand. 2000; 44:910–918. PMID: 10981565.

34. Kumar V, Krone K, Mathieu A. Neuraxial and sympathetic blocks in herpes zoster and postherpetic neuralgia: an appraisal of current evidence. Reg Anesth Pain Med. 2004; 29:454–461. PMID: 15372391.

35. Baidya DK, Khanna P, Maitra S. Analgesic efficacy and safety of thoracic paravertebral and epidural analgesia for thoracic surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2014; 18:626–635. PMID: 24488821.

36. Makharita MY, Amr YM, El-Bayoumy Y. Single paravertebral injection for acute thoracic herpes zoster: a randomized controlled trial. Pain Pract. 2015; 15:229–235. PMID: 24528531.

37. Ji G, Niu J, Shi Y, Hou L, Lu Y, Xiong L. The effectiveness of repetitive paravertebral injections with local anesthetics and steroids for the prevention of postherpetic neuralgia in patients with acute herpes zoster. Anesth Analg. 2009; 109:1651–1655. PMID: 19713253.

38. Makharita MY, Amr YM, El-Bayoumy Y. Effect of early stellate ganglion blockade for facial pain from acute herpes zoster and incidence of postherpetic neuralgia. Pain Physician. 2012; 15:467–474. PMID: 23159962.
39. Hempenstall K, Nurmikko TJ, Johnson RW, A'Hern RP, Rice AS. Analgesic therapy in postherpetic neuralgia: a quantitative systematic review. PLoS Med. 2005; 2:e164. PMID: 16013891.

40. Vieweg WV, Wood MA. Tricyclic antidepressants, QT interval prolongation, and torsade de pointes. Psychosomatics. 2004; 45:371–377. PMID: 15345781.

41. Zin CS, Nissen LM, Smith MT, O'Callaghan JP, Moore BJ. An update on the pharmacological management of postherpetic neuralgia and painful diabetic neuropathy. CNS Drugs. 2008; 22:417–442. PMID: 18399710.

42. Rowbotham M, Harden N, Stacey B, Bernstein P, Magnus-Miller L. Gabapentin for the treatment of postherpetic neuralgia: a randomized controlled trial. JAMA. 1998; 280:1837–1842. PMID: 9846778.

43. Sabatowski R, Gálvez R, Cherry DA, Jacquot F, Vincent E, Maisonobe P, et al. Pregabalin reduces pain and improves sleep and mood disturbances in patients with post-herpetic neuralgia: results of a randomised, placebo-controlled clinical trial. Pain. 2004; 109:26–35. PMID: 15082123.

44. Christo PJ, Hobelmann G, Maine DN. Post-herpetic neuralgia in older adults: evidence-based approaches to clinical management. Drugs Aging. 2007; 24:1–19. PMID: 17233544.
45. Watson CP, Moulin D, Watt-Watson J, Gordon A, Eisenhoffer J. Controlled-release oxycodone relieves neuropathic pain: a randomized controlled trial in painful diabetic neuropathy. Pain. 2003; 105:71–78. PMID: 14499422.

46. Raja SN, Haythornthwaite JA, Pappagallo M, Clark MR, Travison TG, Sabeen S, et al. Opioids versus antidepressants in postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology. 2002; 59:1015–1021. PMID: 12370455.

47. Boureau F, Legallicier P, Kabir-Ahmadi M. Tramadol in postherpetic neuralgia: a randomized, double-blind, placebo-controlled trial. Pain. 2003; 104:323–331. PMID: 12855342.

48. Rowbotham MC, Davies PS, Verkempinck C, Galer BS. Lidocaine patch: double-blind controlled study of a new treatment method for post-herpetic neuralgia. Pain. 1996; 65:39–44. PMID: 8826488.

49. Galer BS, Jensen MP, Ma T, Davies PS, Rowbotham MC. The lido caine patch 5% effectively treats all neuropathic pain qualities: results of a randomized, double-blind, vehicle-controlled, 3-week efficacy study with use of the neuropathic pain scale. Clin J Pain. 2002; 18:297–301. PMID: 12218500.

50. Watson CP, Tyler KL, Bickers DR, Millikan LE, Smith S, Coleman E. A randomized vehicle-controlled trial of topical capsaicin in the treatment of postherpetic neuralgia. Clin Ther. 1993; 15:510–526. PMID: 8364943.
51. Kotani N, Kushikata T, Hashimoto H, Kimura F, Muraoka M, Yodono M, et al. Intrathecal methylprednisolone for intractable postherpetic neuralgia. N Engl J Med. 2000; 343:1514–1519. PMID: 11087880.

52. Doi K, Nikai T, Sakura S, Saito Y. Intercostal nerve block with 5% tetracaine for chronic pain syndromes. J Clin Anesth. 2002; 14:39–41. PMID: 11880021.

53. Jeon YH. Spinal cord stimulation in pain management: a review. Korean J Pain. 2012; 25:143–150. PMID: 22787543.

54. Harke H, Gretenkort P, Ladleif HU, Koester P, Rahman S. Spinal cord stimulation in postherpetic neuralgia and in acute herpes zoster pain. Anesth Analg. 2002; 94:694–700. PMID: 11867400.

55. Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005; 352:2271–2284. PMID: 15930418.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download