Abstract
Recently, percutaneous epidural neuroplasty has become widely used to treat radicular pain caused by spinal stenosis or a herniated intervertebral disc. A 19-year-old female patient suffering from left radicular pain caused by an L4-L5 intervertebral disc herniation underwent percutaneous epidural neuroplasty of the left L5 nerve root using a Racz catheter. After the procedure, the patient complained of acute motor weakness in the right lower leg, on the opposite site to where the neuroplasty was conducted. Emergency surgery was performed, and swelling of the right L5 nerve root was discovered. The patient recovered her motor and sensory functions immediately after the surgery. Theoretically, the injection of a large volume of fluid in a patient with severe spinal stenosis during epidural neuroplasty can increase the pressure on the opposite side of the epidural space, which may cause injury of the opposite nerve by barotrauma from a closed compartment. Practitioners should be aware of this potential complication.
Go to : 
Epidural neuroplasty was introduced by Racz et al. [1] in 1989, and is widely used in the treatment of failed back surgery, spinal stenosis, or disc herniation [2,3,4]. Although the potential risks of complications from epidural neuroplasty are similar to those from other interventional procedures, complications such as bleeding, infections, or nerve damage are especially associated with epidural neuroplasty [5]. Moreover, there can be other complications associated with the procedure, such as dural puncture, catheter shearing, epidural hematoma, intravascular drug injection, meningitis, headache, or blindness. These can be caused by increased intracerebral fluid pressure, cerebral hemorrhage, adverse effects from the injected drugs, or nerve damage, as higher drug dosages are used in epidural neuroplasty than in nerve blocks, and an adhesiolysis procedure is also added [5,6]. In particular, although nerve damage is a rare complication, it can be fatal for the patient. Here we report the case of a patient who suffered from monoplegia of the opposite lower extremity following percutaneous epidural neuroplasty, and recovered after emergency discectomy.
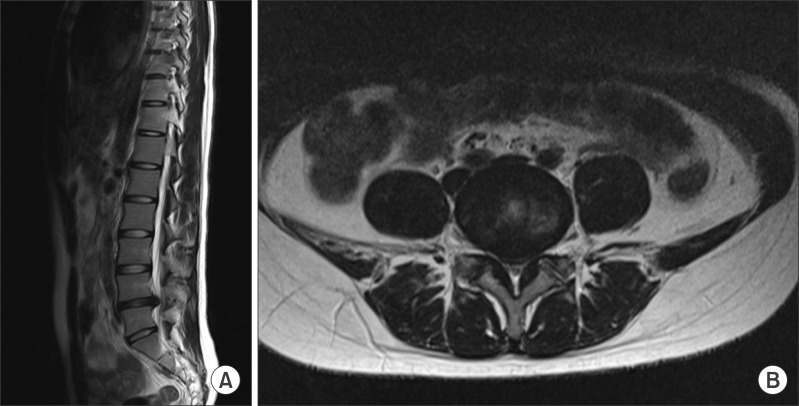
A 19-year-old patient was admitted for low back pain and radiating pain in the posterior aspect of the left leg which had begun 2 months prior. She was treated with nonsteroidal anti-inflammatory drugs, physical therapy, and an epidural block in the local hospital. However, there were no changes in her symptoms. She mainly complained of pain in the left leg, with a score of 6/10 on the visual analogue scale (VAS), and a result of 50 degrees in a passive straight leg-raising test. There were no sensory-motor abnormalities, and the tests for reflexes showed normal responses. Magnetic resonance imaging (MRI) revealed central herniation of the L4-L5 intervertebral disc, which compressed the dural sac (Fig. 1). Discectomy was suggested, as the patient complained of consistent and severe pain, the MRI findings showed severe spinal stenosis, and there were no responses to conservative treatment. However, the patient refused the surgery and wanted interventional treatment. Therefore, we decided to treat her with percutaneous epidural neuroplasty with a Racz catheter on the left L5 spinal nerve root.
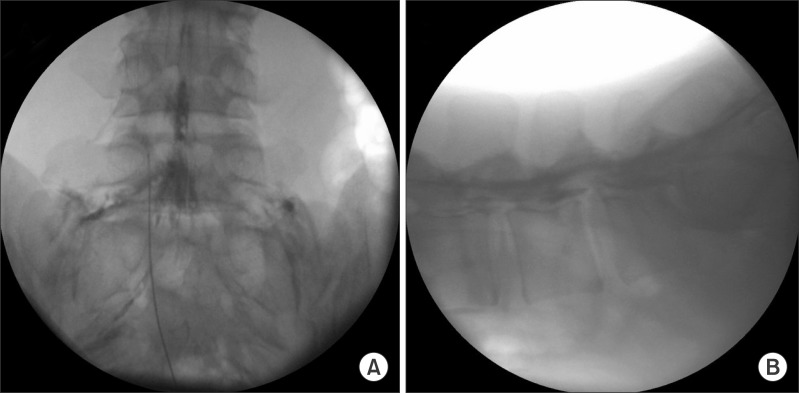
After obtaining her informed consent, she was transferred to the operation room. Prophylactic antibiotics (ceftezole 1 g) were administered intravenously after negative skin test confirmation. Routine monitoring equipment - including an electrocardiogram, blood pressure monitor, and pulse oximeter - were applied, and she was placed in the prone position on the fluoroscopy table. A pillow was inserted under the abdomen to correct the anteflexion of the lumbar vertebrae, the legs were abducted, and the feet were inverted. Following sterile preparation and draping, the location of the sacral hiatus was confirmed by fluoroscopy, and a local infiltration of 1% lidocaine was performed in the insertion area (1 inch right lateral and 2 inches caudal from the sacral hiatus). A 16-gauge RX Coudé needle was inserted through the sacral hiatus. The tip of the needle was placed between the S3 and S4 vertebrae, whose locations were confirmed by fluoroscopy with a C-arm. After confirming negative aspiration of the blood or cerebrospinal fluid (CSF), 10 ml of water-soluble contrast media were injected for the epidurogram. The epidurogram showed a filling defect of the left L5 nerve root. The Racz catheter was inserted through the needle and was advanced towards the left L5 nerve root under continuous fluoroscopy (Fig. 2). 1,500 units of hyaluronidase in 10 ml of normal saline were then injected. Additional dye (2 ml) was injected to confirm the contours of the nerve root, and 9 ml of 0.2% ropivacaine and 1 ml of 4 mg dexamethasone were injected following negative aspiration. The patient did not complain of severe pain, paresthesia, or unusual responses during the procedure. The needle was removed and sterile dressing was performed.
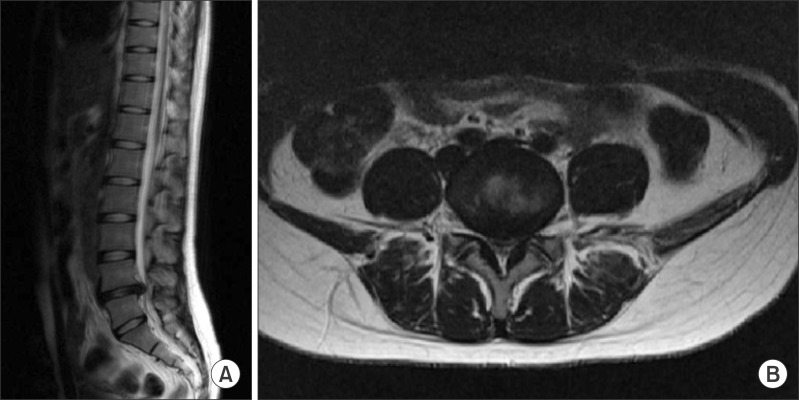
After 1 hour, the patient complained of sudden motor weakness in the right lower limb, on the site opposite to where the neuroplasty was conducted. The great toe dorsiflexion was marked as motor grade I, and the ankle dorsiflexion as motor grade II. Paresthesia and a dull sensation in the right L4-L5 dermatome had developed, but the patient did not complain of pain. At first, we suspected a temporary motor weakness caused by ropivacaine, and the symptoms were observed for one hour. However, the symptoms and signs did not change. An urgent MRI was performed, but no epidural hematoma or suspicious lesions were found (Fig. 3). Around 4 hours after the neuroplasty, the motor and sensory weakness had not improved; emergency surgery was therefore performed. Discectomy of the L4-L5 intervertebral disc was conducted. During the surgery, central and left paracentral protrusions of the disc were found, and swelling of the right L5 nerve root was also discovered. After the surgery, a physical examination was performed in the recovery room. The motor strength and sensory function of the right leg had returned to normal. In the 10-day follow-up period, there were no signs of motor or sensory abnormalities, and the patient was therefore discharged without any discomfort.
Go to : 
Bleeding, infections, or nerve damage can generally develop after epidural neuroplasty, but motor and sensory weaknesses are rare complications [5]. Acute monoplegia following epidural adhesiolysis has previously been reported in a patient with failed-back syndrome and foraminal stenosis of the L4-L5 levels [7]. However, to the best of our knowledge, there has been no report of acute motor weakness in the opposite lower extremity after percutaneous epidural neuroplasty.
There can be several reasons for unilateral motor weakness after epidural neuroplasty [7]. First, motor weakness can be caused by direct nerve injury from the epidural needle or Racz catheter during the procedure. However, this was unlikely in this case, as there were no complaints of acute severe pain, sensory abnormality, or abnormal responses during the procedure. Second, it can be caused by intrathecal or subdural injections of local anesthetics. This was also unlikely in this case, as these injections cause bilateral or patchy blocks of the motor and sensory functions. Third, epidural hematoma is also a possible cause. However, the radiologic findings showed no evidence of hematoma in this case. Fourth, although nerve damage from hypertonics can be a reason, we did not use hypertonic saline [8,9]. Finally, injection of a large volume of fluid into the epidural space may cause a transient neurological deficit [7,8,9].
Rocco et al. [9] reported that epidural injections after spinal surgery may cause complications such as cauda equine syndrome or nerve root damage as the epidural space after surgery is limited, and the injected drugs may increase the pressure and cause nerve damage either directly or by ischemia, due to decreased blood flow. Ho et al. [7] reported a case similar to ours. They presented acute right monoplegia which had occurred after epidural adhesiolysis of the bilateral L5 nerve root in a patient with failed-back surgery syndrome, with spontaneous recovery after 5 weeks. They suggested that the large volume of fluid injection might have been the reason for the transient neurological deficit, as a compartment loculated by the fluids might have compressed the nerve. They also suggested careful injection under observation of the excretion of the contrast dye through the neural foramen in order to prevent nerve injuries caused by compression from a large volume of injected drugs. In particular, if the spinal stenosis is severe, the epidural injection may increase the pressure in the epidural space, and even a mild edema around the nerve root may cause a neurologic deficit by compression of the nerve root [10].
We hypothesized that the large volume of fluid injected during the epidural neuroplasty and the severe spinal stenosis might have been the reason for the opposite motor weakness in this case, as per the previous reported case [7]. The patient in the present study presented severe spinal stenosis, with a herniated disc occupying more than 2/3 of the spinal canal. The epidurogram during the neuroplasty showed a better spread of the contrast dye in the left side, and a filling defect on the right side. Thus, the drugs injected to the right side could not be easily eliminated. Moreover, the central protrusion may have increased the pressure on the right side of the epidural space, and the closed compartment may have caused loculation, leading to barotrauma in the right L5 nerve root [7,9]. In addition, swelling of the L5 nerve root was observed during the surgery, and the motor and sensory functions returned to normal immediately after the surgery, suggesting that the latter had a decompressive effect. However, further evaluations, including measurement of the pressure and radiologic tests, are required to prove this theory.
In conclusion, we presented a rare case of unilateral motor weakness following epidural neuroplasty, on the side opposite to the lesions. The injection of a large amount of fluid during neuroplasty in a patient with spinal stenosis may cause compressive nerve damage. Practitioners should be aware of this potential complication.
Go to : 
References
1. Racz GB, Holubec JT. Racz GB, editor. Lysis of adhesions in the epidural space. In: Techniques of neurolysis. Boston (MA): Kluwer Academic Publishers;1989. p. 57–72.
2. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 2009; 12:361–378. PMID: 19305485.
3. Belozer M, Wang G. Epidural adhesiolysis for the treatment of back pain. Health Technol Assess. 2004; 5:1–19.
4. Helm Ii S, Benyamin RM, Chopra P, Deer TR, Justiz R. Percutaneous adhesiolysis in the management of chronic low back pain in post lumbar surgery syndrome and spinal stenosis: a systematic review. Pain Physician. 2012; 15:E435–E462. PMID: 22828693.
5. Lee F, Jamison DE, Hurley RW, Cohen SP. Epidural lysis of adhesions. Korean J Pain. 2014; 27:3–15. PMID: 24478895.

6. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012; 15:131–140. PMID: 22430650.
7. Ho KY, Manghnani P. Acute monoplegia after lysis of epidural adhesions: a case report. Pain Pract. 2008; 8:404–407. PMID: 18721177.

8. Bromage PR. Subarachnoid catheters and the cauda equina syndrome: hypotheses in need of trial. Anesthesiology. 1994; 80:711–712. PMID: 8141477.
9. Rocco AG, Philip JH, Boas RA, Scott D. Epidural space as a Starling resistor and elevation of inflow resistance in a diseased epidural space. Reg Anesth. 1997; 22:167–177. PMID: 9089860.

10. Chaudhari LS, Kop BR, Dhruva AJ. Paraplegia and epidural analgesia. Anaesthesia. 1978; 33:722–725. PMID: 717716.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download