Abstract
Background
To explore the relationship between persistent post-radiotherapy pain and locoregional recurrence in head and neck cancer patients.
Methods
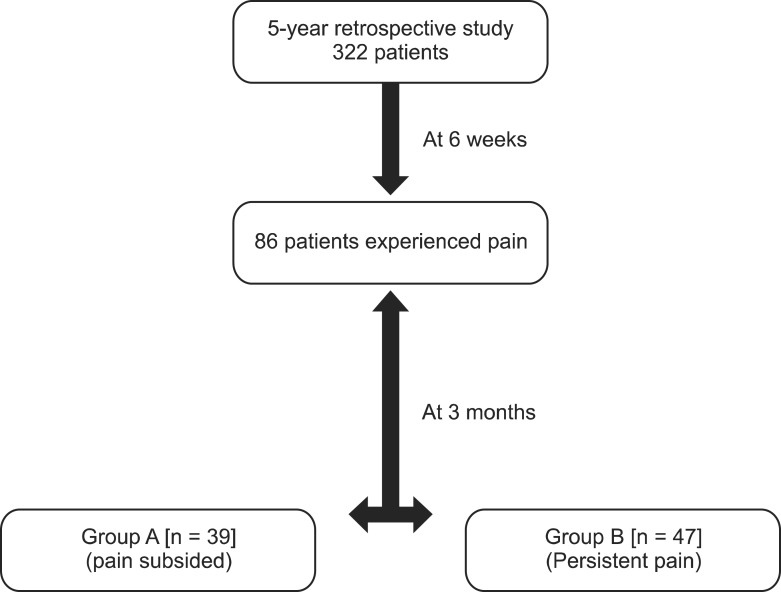
Five year retrospective data was reviewed of 86 patients of head and neck cancer treated with radiotherapy who continued to have pain at 6 weeks after completion of treatment. At follow-up after 3 months, these patients were stratified into: Group A (n = 39) constituted of patients whose pain subsided and Group B (n = 47) were patients who continued to have persistent pain.
Results
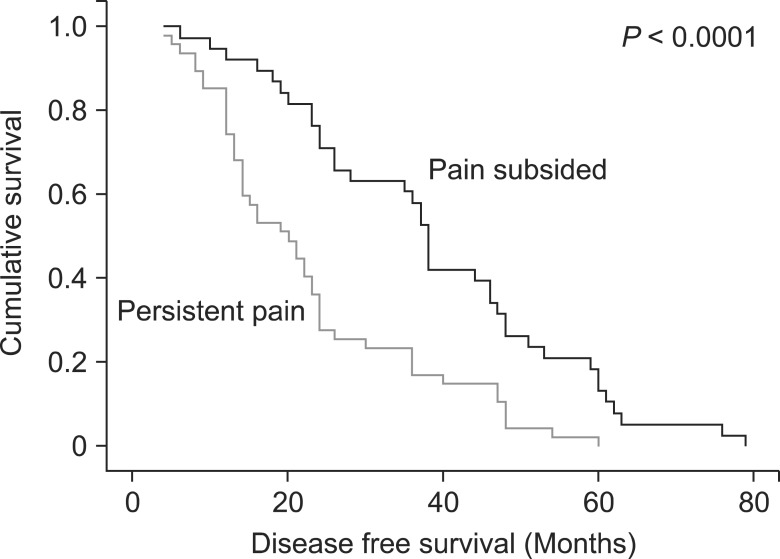
At median follow-up time of 25 months (range: 8-47), one patient (2.6%) and 18 (38.3%) patients in group A and group B had locoregional recurrence respectively (P < 0.0001). Furthermore, group B patients had higher mean pain score levels as compared to group A (P = 0.03). Patients in whom pain subsided within 3 months had statistically much greater disease-free survival in comparison to those with persistent pain (P < 0.0001).
Conclusions
Pain in head and neck cancer is an important symptom and should be considered a poor prognostic factor. In the current study, the majority of the patients with persistent pain had recurrent disease as compared to those in whom pain subsided within 3 months of post-treatment. It is suggested that patients with persistent pain need more intense follow-up and should be investigated thoroughly to detect recurrence at an early stage to provide a better quality of life.
Go to : 
Head and neck squamous cell carcinoma (HNSCC) is the sixth most common cancer worldwide, with an estimated annual burden of 633,000 incident cases and 355,000 deaths [1]. Treatment for head and neck cancer involves single or multimodality therapy employing surgery, chemotherapy and/or radiotherapy as the standard of care for these patients. Despite aggressive primary treatment, locoregional relapse accounts for approximately 80% of treatment failures.
Pain is an important but infrequently analyzed symptom in head and neck cancer. Fifty percent to 60% of patients with head and neck cancer will experience moderate to severe pain [2]. This pain may be associated with the initial presentation due to direct invasion by cancer, infiltration of pain sensitive structures, and if secondary oral infection occurs or due to recurrence, or treatment of head and neck cancer [3].
Head and neck cancer patients have nociceptive pain as a result of acute inflammation (e.g., radiation mucositis). It usually takes 6-8 weeks to resolve when they have neuropathic pain, while nerves are infiltrated or compressed by the tumour. It manifests as a sharp, intense, shocking, or shooting pain. Persistent unrelieved nociceptive pain associated with the tumour or cancer treatments (e.g., mucositis) can also lead to neuropathic pain [4].
The association of pain with recurrent head and neck cancer has been recognized, and in some cases pain may be the only indication of recurrent disease [5]. Moderate to severe post-treatment pain has been found to be associated with a lower five-year survival rate compared with those who had low pain scores [6].
Pain within the first year of treatment for head and neck cancer is an important symptom that should be appropriately monitored and managed during routine follow-up [6], as it can exacerbate problems in swallowing and speaking with a significant impact on quality of life. We herein report a retrospective audit of 86 head and neck carcinoma patients complaining of pain at 6 weeks after the completion of treatment. Our objective in doing this audit is to explore any relationship between persistent post-radiotherapy pain, after the acute radiation reactions have settled, and loco-regional recurrence in head and neck cancer patients.
Go to : 
We retrospectively reviewed the data of all head and neck cancer patients treated with radical radiotherapy (RT) or concurrent chemoradiation from 2008-2012. Eligible patients were those with histopathological diagnosis of head and neck cancer treated with radical radiotherapy with or without chemotherapy and experienced pain at 6 weeks after the completion of treatment. The patients who underwent surgery prior to radiation therapy, previously irradiated for primary head and neck malignancy and those who had undergone local excision or brachytherapy were excluded from the study. We retrieved the data of 322 patients from medical records and after scrutinizing the case records, we found that 86 (26.7%) of patients were validated for inclusion in the analysis (Fig. 1).
Patients were staged according to the 2002 classification of the American Joint Committee on Cancer (AJCC, 6th edition) Staging system [7]. All the patients received external beam radiotherapy, from a Co-60 teletherapy unit with conventional treatment techniques utilizing 2 parallel opposed lateral portals, to the primary site and regional lymphatic areas, with or without concurrent chemotherapy. A standard total dose of 60-70 Gy, 2 Gy / F, 5 days a week was delivered to all the patients, off cord at 40 Gy. During the treatment, patients were reviewed weekly by a radiation oncologist and more frequently when necessary.
Assessment of the severity of pain was done using the Numerical Rating Scale (NRS) [8] as a routine in our institution, and appropriate pain medications were prescribed according to World Health Organization (WHO) three-step analgesic ladder [9]. The patients were moved up or down the ladder based on the clinical assessment of pain.
The assessment of tumour response was performed at 3 months after the completion of treatment, including a complete physical examination, fiberoptic endoscopy and imaging (Contrast enhanced computed tomography/Magnetic resonance imaging) according to the Response Evaluation Criteria in Solid Tumours (RECIST) guidelines VERSION 1.0 [10]. Loco-regional recurrence was defined as the presence of a biopsy-proven recurrent lesion in the head and neck region after a minimum duration of 6-8 weeks after concurrent chemoradiotherapy/ radiotherapy [11]. A biopsy was performed if there was suspicion of residual or recurrent disease.
According to the follow-up policy of our institution, all patients were examined at the completion of treatment, at 6 weeks post-treatment and then followed up monthly for the first year, quarterly in the second year, and bi-annually thereafter. All the relevant details, including symptoms at presentation, tumour site, date of diagnosis, stage, histopathology and treatment details were collected. Pain scores at 3 months, details of the use of rescue treatments, the temporal components of pain, response to treatment and recurrence details as documented in a patient's case record forms were noted. The edema and acute inflammation caused by radiotherapy settles in the first 3 months post-treatment. Due to this reason, we chose to stratify the patients into two groups: Group A included 39 patients whose pain subsided within 3 months after the completion of treatment and Group B included 47 patients who continued to have persistent pain.
The data was analyzed using SPSS software, version 21 (IBM Corp, Armonk, NY). For categorical variables Chi square test was used and for continuous variable independent t-test was used. All patients were included in the survival analysis. Treatment outcome/survival rates were evaluated using the Kaplan-Meier survival analysis, including the log rank test, was performed. Disease-free survival was calculated from the date of completion of treatment to the date when local, regional, or locoregional recurrence was first recorded. Statistical significance was defined as P value less than 0.05.
Go to : 
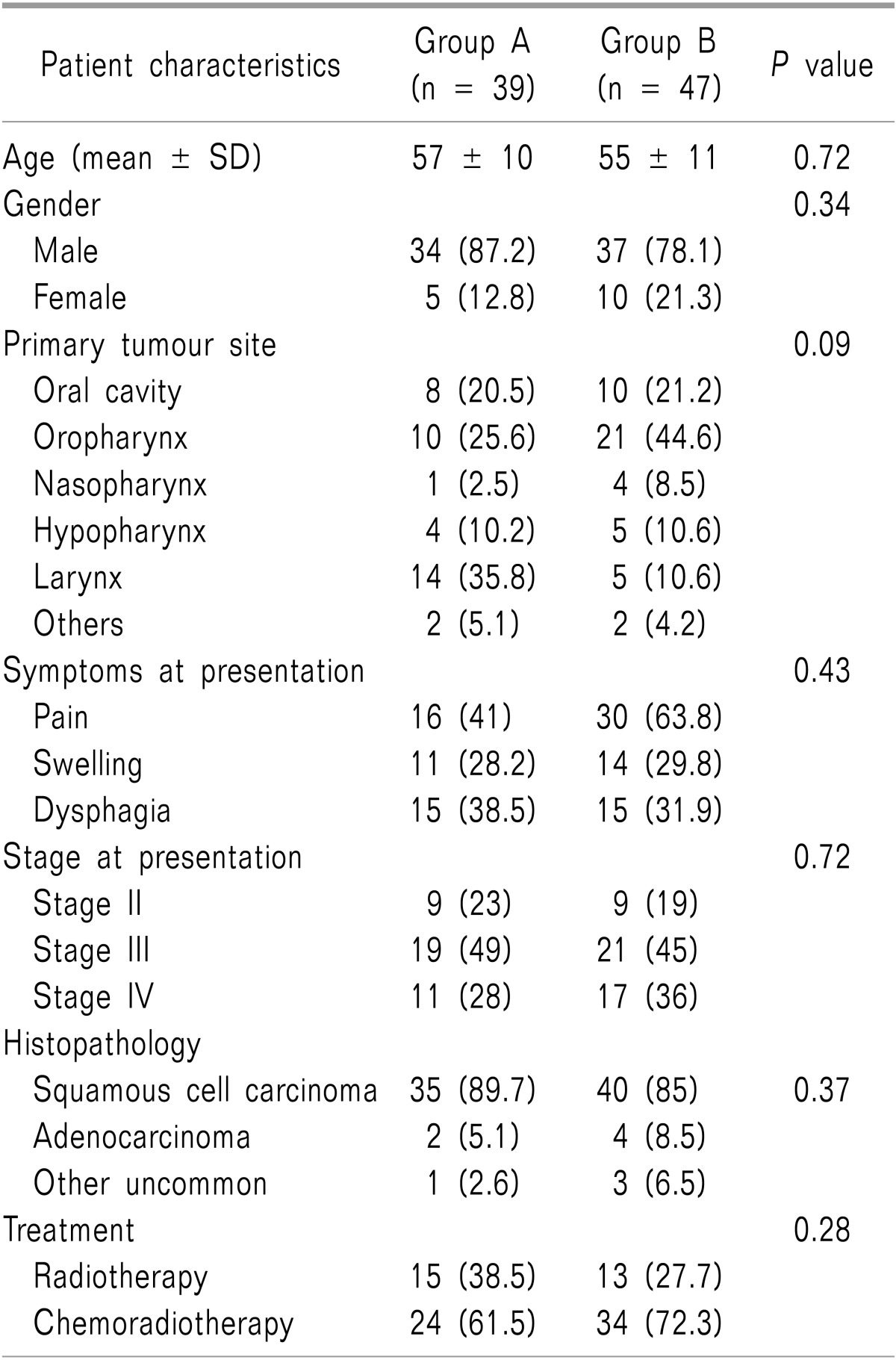
There were 71 (82.6%) males and 15 (17.4%) females studied. The mean age was 57 years ± 10 SD and 55 years ± 11 SD for group A and group B patients, respectively. The demographic details of patients in terms of gender, primary tumour site, symptoms at presentation, stage, histopathology and treatment were similar in both the groups as shown in Table 1. The median follow-up was 25 months (range: 8-47 months).
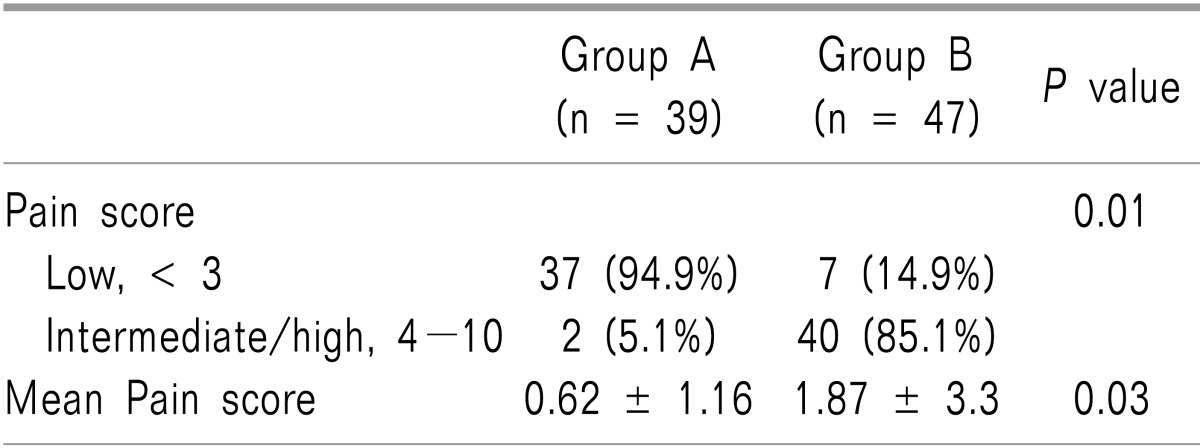
The majority of patients completed the planned course of treatment. Of the 86 patients who qualified for the study, 71 (82.6%) patients had inflammatory pain whereas 15 (17.4%) had neuropathic pain at 6 weeks after completion of treatment. Further, we found that > 60% of the patients who had neuropathic pain experienced recurrence at a later date. According to our data base, 40% of patients were prescribed WHO Step I analgesics (NSAIDS and non-opioids), 51% of patients were on Step II analgesics (weak opioids) for mild to moderate pain and 9% of patients were on Step III medications (opioids) for moderate to severe pain. On calculating the mean pain scores, group B patients showed a statistically significant higher mean pain score with a P value = 0.03 as compared with group A patients (Table 2).
At 3 months after completion of treatment, all patients were assessed for the treatment outcomes according to the RECIST criteria. The data revealed that among group A patients, 35 (92.1%) patients achieved complete response (CR) and 2 (5.3%) patients had partial response (PR). While in group B, 19 (40.4%) patients had CR and 10 (21.3%) patients had PR. At median follow-up of 25 months, only 1 (2.56%) patient in group A and 18 (38.3%) patients in group B had locoregional recurrence respectively. Amongst the 18 (38.3%) patients with locoregional failure, 13 (72.2%) had local recurrence, 4 (22.2%) had nodal failures and one patient had both local and nodal recurrence.
The reduced incidence of recurrence in group A patients translated into better DFS for group A as compared to group B patients, with a median DFS of 38 months vs. 19 months (Fig. 2).
Among the patients with persistent pain (Group B), those with age ≥ 50 years, oropharynx primary site and those with stage III and IV disease had higher incidence of locoregional recurrence. However, we could not find any statistically significant difference in univariate analysis between these prognostic factors studied and loco-regional recurrence.
Go to : 
Only very few studies have highlighted the significance of pain that persists even after completion of treatment in HNSCC. In the present study, we analyzed the association of persistent pain with locoregional recurrence in retrospectively collected data of patients with HNSCC treated with radiotherapy or chemoradiotherapy. A strong association between post-radiotherapy pain and locoregional recurrence and their negative impact on DFS was found. On the other hand, there was a significant benefit with regards to DFS in patients who did not have persistent post-radiotherapy pain. Thus, strongly supporting the evidence that pain serves as a warning signal of imminent damage for patients with head and neck cancer.
Grond et al. [12], conducted a study on the type of pain experienced by head and neck cancer patients prior to, during and after treatment. They studied 167 patients, and of these, 138 (83%) patients had cancer-related pain, 80% had soft-tissue pain, 20% had bone pain and 35% had neuropathic pain. Similarly, we found that among the total patients, 82.6% patients had inflammatory (nociceptive) pain and 17.4% experienced neuropathic pain after the treatment. More than 60% of patients with neuropathic pain had recurrence at some time during follow-up, as compared to inflammatory pain patients.
All patients in whom pain subsided following radical treatment had a low pain score (< 3), in comparison to approximately 85% patients who reported an intermediate or high level of persistent pain (P value = 0.01). The mean pain score of the patients with persistent pain was significantly greater than patients in whom pain subsided (P value = 0.03). Our results are comparable with the results observed in a study by Scharpf et al. [6], suggesting that patients with an intermediate or high pain score (4-10) are more likely to experience recurrence at a later date than those who had low pain at any point during routine follow-up.
Pain due to local recurrence is a major palliative issue in terminal head and neck cancer patients as it affects the quality of life of these patients and at times it may be the first symptom indicating recurrent disease [13]. We attributed the disappearance of pain in our patients as evidence that as the mucosal reactions completely subside and return to normalcy in 3 months duration, it leads to pain relief whereas it continued for group B patients even after the reactions have settled. Our results showed that among the patients with persistent pain, 38.3% had loco-regional recurrence as compared to 2.56% in patients in whom pain subsided (P value < 0.0001). Thus, our study provides evidence that there is a strong association between persistent pain and disease recurrence. Our results found that the median interval between the onset of pain and the diagnosis of recurrent disease was 3 months. Similar to a study by Smit et al. [5], in which they reported pain as the first symptom indicative of recurrence in 70% of patients with a median lag time of 4 months.
The treatment of the head and neck cancer patients should always be undertaken in a holistic manner and to achieve this, good pain control is of paramount importance. Better survival rates have been observed with advances in the multimodality approaches in head and neck cancer treatment. Our data indicated a statistically significant 5- year DFS benefit for patients in whom pain subsided after treatment as compared to those with persistent pain (P value < 0.0001). On further analysis, we found that various prognostic factors such as age ≥ 50 years, oropharynx cancers and those with stage III and IV disease had higher incidence of locoregional recurrence, although it did not reach statistical significance.
To the best of our knowledge, very few studies have been done in this context. The drawback of our study is that it is a retrospective audit and features a small sample size, but despite the limited sample size, the association between persistent pain and locoregional recurrence reached statistical significance.
Head and neck cancer patients experience multiple, unique, and troublesome symptoms due to the direct effect of cancer and treatment side effects which influence the nutritional status, and these in turn have a major impact on the quality of life. For a significant proportion of patients, moderate to severe pain peaks after treatment during an interval with no routine medical surveillance or intervention. It is evident from our study and other studies quoted in the literature that identifying patients experiencing persistent pain during outpatient follow-up visits would enable us to diagnose recurrent disease early in the course while it is still salvageable. Hence, we recommend a prospective study with a larger series of patients and longer follow-up to validate our findings.
Pain as a subject is still under research and its relation to locoregional recurrence is an important warning signal indicating recurrent disease in head and neck cancer patients. In summary, our data suggest that oncologists should be aware of the fact that persistent pain might point to development of recurrent disease which in turn should alert the treating physician towards early identification of patients with recurrent disease while it is salvageable. By appropriately monitoring pain and appropriate diagnostic evaluations during routine follow-ups, we may eventually contribute positively to the quality of life and better survival of head and neck cancer patients.
Go to : 
References
1. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010; 127:2893–2917. PMID: 21351269.

2. Raj PP, Phero JC. Pain control in cancer of the head and neck. In : Thawley SE, Panje WR, editors. Comprehensive management of Head and Neck Tumors. 2nd ed. Philadelphia: WB Saunders;1987. p. 42–68.
4. Epstein JB, Wilkie DJ, Fischer DJ, Kim YO, Villines D. Neuropathic and nociceptive pain in head and neck cancer patients receiving radiation therapy. Head Neck Oncol. 2009; 1:26. PMID: 19594943.

5. Smit M, Balm AJ, Hilgers FJ, Tan IB. Pain as sign of recurrent disease in head and neck squamous cell carcinoma. Head Neck. 2001; 23:372–375. PMID: 11295810.

6. Scharpf J, Karnell LH, Christensen AJ, Funk GF. The role of pain in head and neck cancer recurrence and survivorship. Arch Otolaryngol Head Neck Surg. 2009; 135:789–794. PMID: 19687400.

7. Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al. AJCC Cancer Staging Manual. 6th ed. Philadelphia, USA: Lippincott-Raven;2002. p. 33–46.
8. Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003; 3:310–316. PMID: 17166126.

9. Ventafridda V, Saita L, Ripamonti C, De Conno F. WHO guidelines for the use of analgesics in cancer pain. Int J Tissue React. 1985; 7:93–96. PMID: 2409039.
10. Therasse P. Measuring the clinical response. What does it mean? Eur J Cancer. 2002; 38:1817–1823. PMID: 12204662.

11. Chen YH, Jian JJ, Chan KY, Tsai SY, Cheng SH, Yen KC, et al. Definitive chemoirradiation for resectable head and neck cancer: treatment outcome and prognostic significance of MRI findings. Br J Radiol. 2008; 81:490–498. PMID: 18487389.

12. Grond S, Zech D, Lynch J, Diefenbach C, Schug SA, Lehmann KA. Validation of World Health Organization guidelines for pain relief in head and neck cancer. A prospective study. Ann Otol Rhinol Laryngol. 1993; 102:342–348. PMID: 7683853.

13. Cuffari L, Tesseroli de Siqueira JT, Nemr K, Rapaport A. Pain complaint as the first symptom of oral cancer: a descriptive study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:56–61. PMID: 16831673.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download