This article has been
cited by other articles in ScienceCentral.
Abstract
Background
This study sought to determine safe ranges of oblique angle, skin entry point and needle length by reviewing computed tomography (CT) scans and to evaluate the usefulness of a bent tip needle during celiac plexus block (CPB).
Methods
CT scans of 60 CPB patients were reviewed. Image of the uppermost margin of L2 vertebral body was used to measure the minimal and maximal oblique angles and the distances from the midline to skin puncture point. The imaginary needle trajectory distance was calculated by three-dimensional measurement. When the procedure was performed by using a 10° bent tip needle under a 20° oblique X-ray fluoroscopic view, the distance (GF/G'F) from the midline to the actual puncture site was measured.
Results
The imaginary safe oblique angle range was 26.4-34.2° and 27.7-36.0° on the right and left, respectively. The distance from the midline to skin puncture point was 6.1-7.6 cm on the right and 6.3-7.6 cm on the left. The needle trajectory distance at minimal angle was 9.6-11.6 cm on the right and 9.5-11.5 cm on the left. The distance of GF/G'F was 5.1-6.5 cm and 5.0-6.4 cm on the right and left, respectively. All imaginary parameters were correlated with BMI except for GF/G'F. All complications were mild and transient.
Conclusions
We identified safe values of angles and distances using a straight needle. Furthermore, using a bent tip needle under a 20° oblique fluoroscopic view, we could safely perform CPB with smaller parameter values.
Keywords: Bent tip needle, Celiac plexus block, Fluoroscopy, Retrocrural approach, Visceral pain
INTRODUCTION
At terminal stage of abdominal cancer, abdominal pain is caused by somatic, visceral, or neuropathic components. In many cases, because these three components are mixed, the abdominal pain associated with cancer can be difficult to treat [
1]. Celiac plexus block (CPB) and neurolysis are effective in treating refractory upper abdominal visceral pain caused by hepatic, stomach or pancreatic cancer [
2]. There are various guidance techniques for CPB such as X-ray fluoroscopy [
3], computed tomography (CT) [
4], and endosonography [
5]. However, fluoroscopy guided CPB was still often performed in practice. The important point is to locate the exact placement of the needle tip [
6,
7].
In practice of the CPB, the posterior retrocrural approach is the classic and commonly used approach. However, it is difficult to identify accurate anatomy using fluoroscopy in order to avoid puncture injury of the organs [
4]. The posterior retrocrural approach may cause puncture injury at the kidney, liver, pleura, and major vessels [
1]. And cancer patients have an elevated risk of major organ injury due to regional anatomic distortions [
8,
9]. If these organs are damaged, the patient may lead to serious complications. Therefore, when the block is performed using fluoroscopy, safe landmarks are needed to prevent puncture injury.
Recommendations exist for guidelines, landmarks, distance from midline to puncture site, and angle of needle insertion for the classic posterior retrocrural approach [
1,
3]. Even so, there is the possibility that organs may be injured if these guidelines are applied to people with a smaller frame. Different safe guidelines are needed for smaller individuals. Moreover, there have been no reports related to the safety and effectiveness of using a bent tip needle for CPB. Thus, in this study, we reviewed CT abdomen and fluoroscopic images of cancer pain patients to determine safe ranges of oblique angle, skin entry point and needle depth, and to evaluate the safety and effectiveness of using a bent tip needle.
MATERIALS AND METHODS
This retrospective study was approved by the institutional review board of Gangnam Severance Hospital, Yonsei University College of Medicine (#3-2014-0170).
Sixty patients (31 males, 29 females) treated with CPB for the abdominal visceral cancer pain, were included in this study. CT abdomen images with intravenous contrast (Somatom Sensation 64, Siemens Medical Solutions, Erlangen, Germany) taken for diagnosis or follow-up were reviewed on a picture archiving and communication system (PACS). All values were measured on the right and left side, respectively.
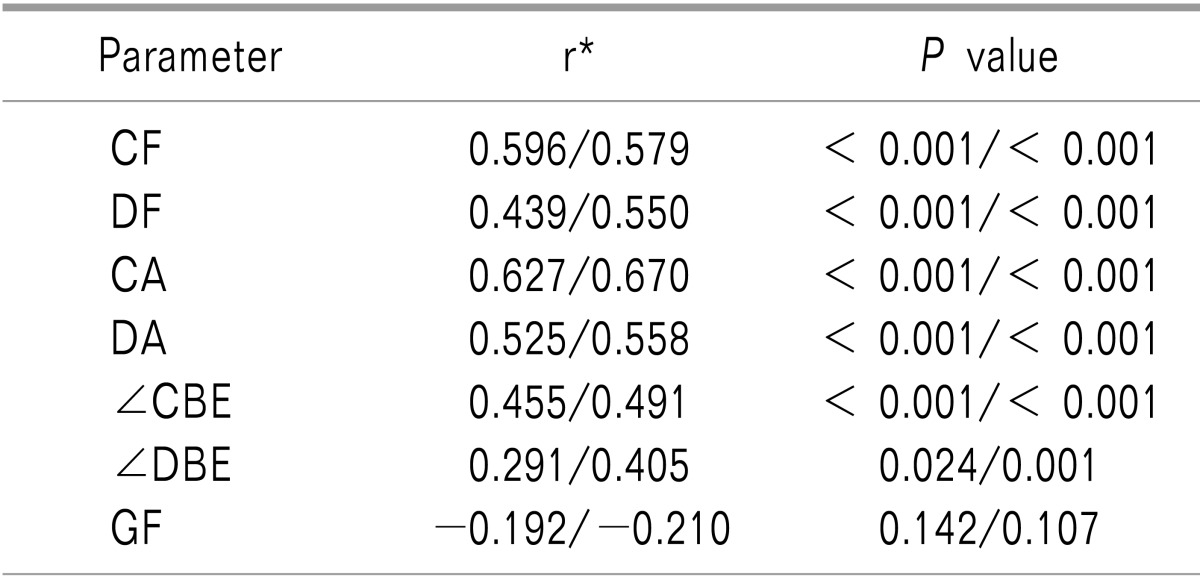
In transaxial CT abdomen images, the target of retrocrural approach was defined as the anterolateral part of the L1 vertebral body at the level of the celiac artery crossed with a vertical line connecting the mid portion of the pedicles (A) (
Fig. 1) [
7]. The uppermost margin of the L2 vertebral body was identified by scrolling the CT images. As this approach was based on previous recommendations, we measured imaginary values at this level [
3,
7]. On the image, we measured the minimum and maximum oblique angles and distances from the midline (F) to the puncture site while avoiding major abdominal organs. Each landmark was designated as follows: the anterolateral part of the L2 vertebral body crossing the vertical line of the mid portion of the pedicle, not to penetrate the crura (B), the skin surface farthest from the midline to project tangentially to B while avoiding major abdominal organs (C), the nearest skin surface to project tangentially to B while avoiding interference with osteophytes or lateral bony structures of the L2 vertebral body (D), and the skin surface crossing the vertical line of mid portion of pedicle (E). The maximum oblique angle was defined as ∠CBE, and the minimum oblique angle was defined as ∠DBE. The distances from midline to C and D were also measured (CF, DF).
The imaginary needle trajectory distance (CA, DA) was defined as the distance from the skin surface (C, D) to the target (A). To calculate this imaginary needle trajectory distance by three-dimensional measurement, the distance (AB) from A to B was directly measured on flat abdomen image of CT abdomen. Next, distances of CB and DB were also directly measured on the uppermost margin of the L2 vertebral body in transaxial CT abdomen images. As the imaginary triangles CBA and DBA are right triangles, the imaginary needle trajectory distance (CA, DA) was calculated by the Pythagorean theorem (AB2 + CB2 = CA2).
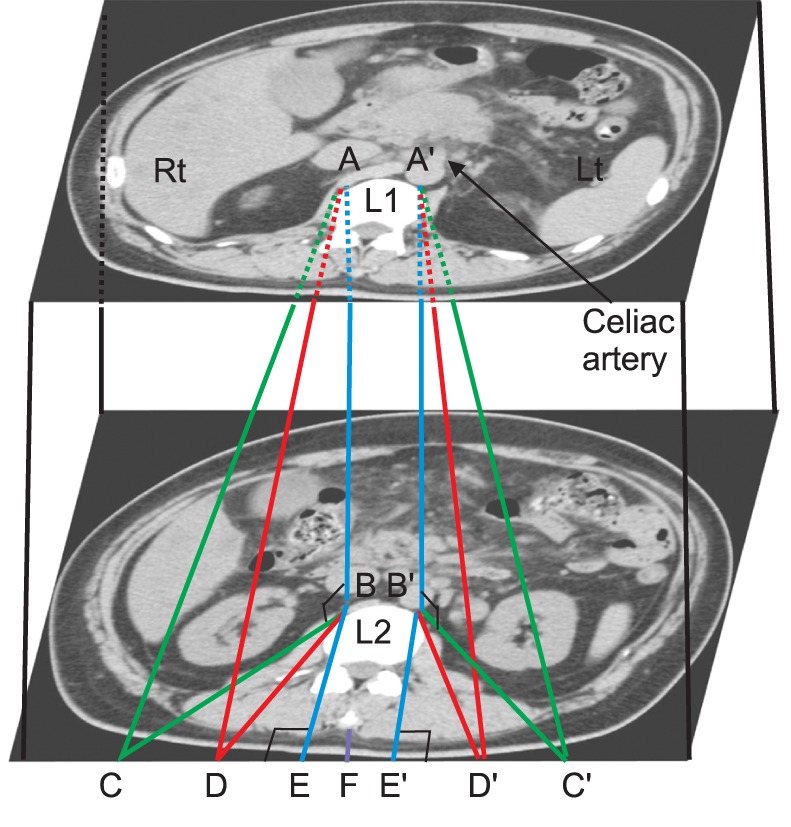
We evaluated the pre-procedure CT abdomen images and consideration that the needle length. All patients underwent CPB by a posterior retrocrural approach utilizing a 10° bent at the 1 cm tip of 22G short bevel needle. The puncture point was defined the lateral margin of the L2 upper end plate under 20° oblique angle fluoroscopic view and the needle was advanced to the target as
Fig. 2B. When the procedure was performed by this method, the distance (GF) from the midline to the actual puncture site (G) was measured by reviewing X-ray fluoroscopy images (
Fig. 2).
In addition, body mass index (BMI) was calculated for evaluation of correlation with CF, DF, CA, DA, ∠CBE, ∠ DBE, and GF. Medical records were also reviewed to record the change of visual analogue scale (VAS) before and after CPB along with any complications related to CPB.
1. Statistical analysis
All measured or calculated distances and angles were recorded as mean ± SD. The difference between the right and left was analyzed by paired t-test. The relationship between BMI and each measured value was analyzed with Pearson's correlation analysis. A P value less than 0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 18.0 (SPSS, Chicago, IL, USA).
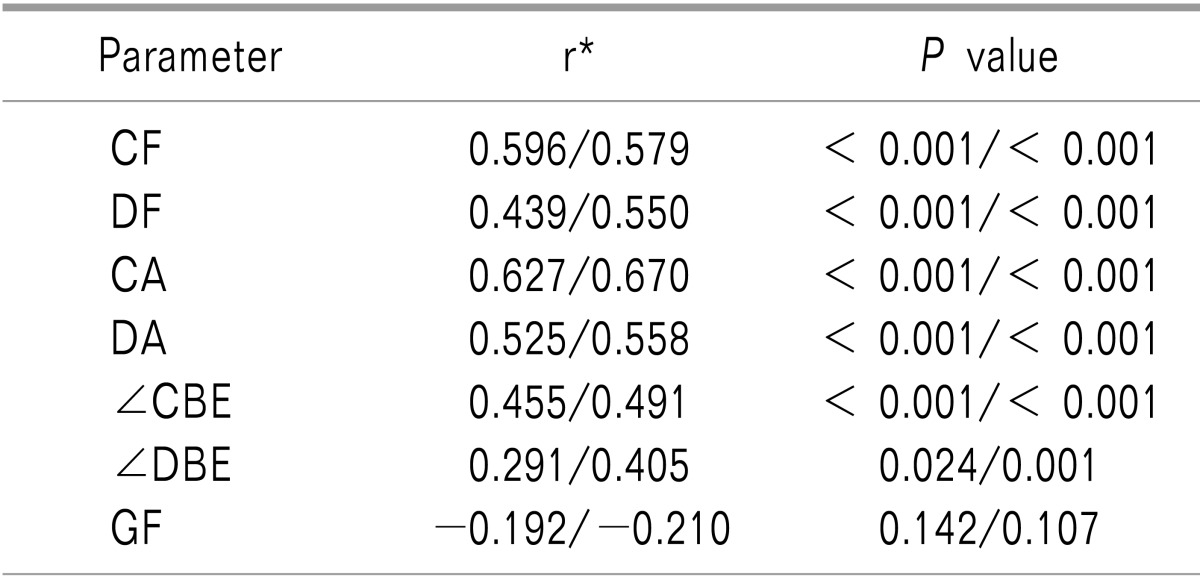
RESULTS
Patient demographic data and the difference of VAS between before and after CPB are shown in
Table 1.
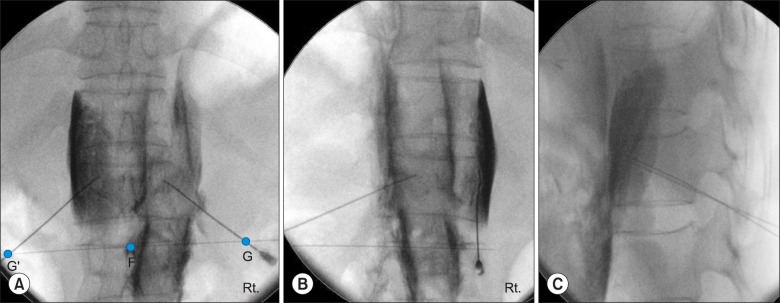
The maximum distance from midline to puncture point (CF) was 8.0 cm and 7.1 cm on the right side in males and females, and 8.3 cm and 7.2 cm on the left side (C'F) in males and females, respectively (Total 7.6 ± 1.7 cm/7.8 ± 1.7 cm, right/left). The minimum distance from midline to puncture point (DF) was 6.6 cm and 5.7 cm on the right side in males and females, and 6.8 cm and 5.8 cm on the left side (D'F) in males and females, respectively (Total 6.1 ± 1.1 cm/6.3 ± 1.2 cm, right/left).
The maximum calculated imaginary needle trajectory distance (CA) was 11.4 cm and 10.8 cm on the right side in males and females, and 11.4 cm and 10.7 cm on the left side (C'A) in males and females, respectively (Total 11.1 ± 1.2 cm/11.1 ± 1.2 cm, right/left). The minimum calculated imaginary needle trajectory distance (DA) was 10.9 cm and 10.3 cm on the right side in males and females, and 10.8 cm and 10.2 cm on the left side (D'A) in males and females, respectively (Total 10.6 ± 1.0 cm/10.5 ± 1.0 cm, right/ left).
The maximum oblique angle (∠CBE) was 34.9° ± 8.2° and 33.0° ± 7.4° on the right side in males and females, and 37.7° ± 7.5° and 34.2° ± 8.9° on the left side (∠C'BE) in males and females, respectively (Total 34.2° ± 7.8°/36.0° ± 8.3°, right/left). The minimum oblique angle (∠DBE) was 27.0° ± 5.0° and 25.6° ± 5.9° on the right side in males and females, and 28.7° ± 5.3° and 26.7° ± 5.3° on the left side (∠D'BE) in males and females, respectively (Total 26.4° ± 5.5°/27.7° ± 5.4°, right/left).
There were three patients (one on the right and two on the left) who had a maximum oblique angle that was smaller than the 25° oblique angle. In all three cases, the maximum oblique angle was limited by the kidney, but the minimum oblique angle was larger than 20°.
The distance (GF) from the midline to the actual puncture site (G) utilizing a bent tip needle under 20° oblique angle fluoroscopic view was 5.8 cm and 5.7 cm on the right side in males and females, and 5.9 cm and 5.5 cm on the left side (G'F) in male and female, respectively (Total 5.8 ± 0.7 cm/5.7 ± 0.7 cm, right/left) (
Table 2).
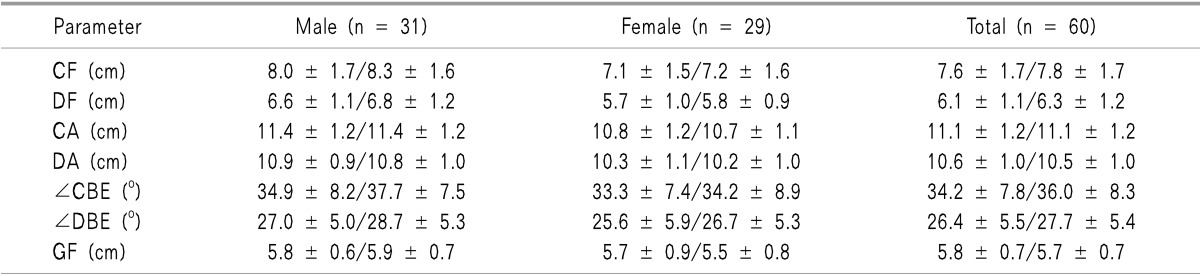
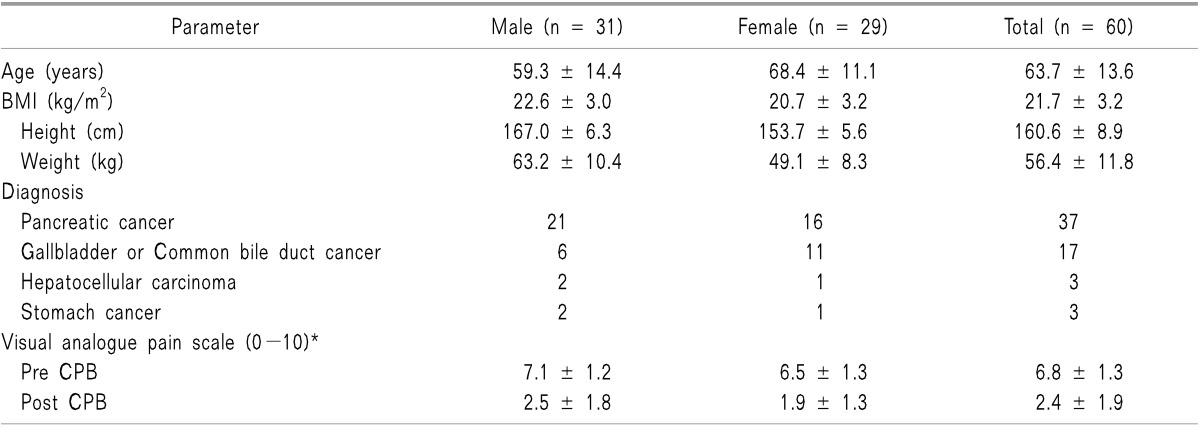
There were significant positive linear correlations between BMI and all distances and angles except GF and G'F (
Table 3). There were no significant differences between the right and left side for any of the measured parameters.
Twenty-three out of 60 patients had complications after neurolytic CPB, including hypotension in 9, nausea in 6, diarrhea in 6, alcohol intoxication in 7, and alcohol neuritis in 1. There were no serious complications such as organ puncture or bleeding, and all complications were transient and mild.
DISCUSSION
Our results from CT abdomen images showed that the minimum oblique angle was 26.4° ± 5.5° and 27.7° ± 5.4° (right and left) in total patients. We could see that this minimum angle was greater than 20° oblique angle with a 10° bent tip needle.
Most celiac ganglia are located between the lower one third of T12 and the upper two thirds of the L1 vertebral body or at the level between the celiac and splanchnic arteries [
6,
7]. Accordingly, the target of the puncture needle in retrocrural approach for CPB is the anterolateral part of the upper margin of the L1 body. When the posterior retrocrural approach is used for CPB, the kidney, liver, pleura, major vessels and other major organs may be injured during the procedure [
1]. According to reports, less than 2% of patients suffer major complications and most reported complications are transient and mild [
10,
11], but serious complications may lead to pneumothorax, pleuritis, pericarditis, hematuria, local hematoma, and arterial injury [
10,
12]. In this study, safe puncture site and oblique angle were measured by reviewing patient CT abdomen images before the procedure. In addition, the use of a 10° bent tip needle under 20° oblique angle fluoroscopic view allowed the procedure to be safely performed with smaller values than the measured parameters. Besides, there were no serious complications about major organ injury, and the complications that did occur were mild, transient, and related to the systemic absorption of alcohol or blocking of the sympathetic nerve.
Serious complications were avoided for several reasons. First, the bent needle tip could help be located to the anterolateral surface of the vertebral body in the retrocrural space. Second, we did a diagnostic block with 10 ml of local anesthetics and at least 30 minutes later followed by 10-15 ml of anhydrous ethyl alcohol at each needle. This volume is much smaller than 25 ml recommended by until recently [
3]. In doing so, we demonstrated that a safe and effective procedure could be performed with only 10 ml of anhydrous ethyl alcohol.
There are various approaches to CPB, such as the classic retrocrural approach, transdiscal approach [
13], transcrural approach [
14], transaortic approach [
15], and anterior approach [
16,
17]. Methods of guidance are also various, such as X-ray fluoroscopy [
3], CT [
4], and endosonography guidance [
5]. CT or endosonography guided CPB has advantages in identifying the location of major organs and the position of needle. CT also has disadvantages, however, such as high radiation dose, limited availability based on the resources of the treatment facility, and low cost-effectiveness. Endosonography requires specialized equipment and expertise from specialists such as gastroenterologists [
18]. For these reasons, fluoroscopy guided CPB is still often performed in practice. In this study, fluoroscopy guidance was used based on the practitioner's expertise, the facility, and better cost effectiveness relative to other guidance methods. The posterior retrocrural approach was chosen due to a classic accumulating experience and its more standardized technique compared to others. In this setting, the safe oblique angle, puncture site, and needle trajectory were identified.
The retrocrural approach was first described by Kappis and reinforced by several pioneers in pain clinic field [
19]. Moore advised that the landmarks are the sides of an isosceles triangle formed by the cephalic portion of the L1 vertebral body and the intersection of the 12th rib and lateral border of the bilateral paraspinal muscles at the level of the L2 vertebral body. These landmarks are utilized in guiding the needle. According to the suggestion, the site of needle puncture is less than 7.5 cm lateral to the midline, and the angle of needle is 45 degrees toward the midline and 15 degrees cephalad [
3]. However, these recommended values are not obvious and difficult to apply equally to patients with a small frame. Therefore, different safe values are required based on body size. In this study, the target of retrocrural approach was set at the upper anterolateral part of the L1 vertebral body, where celiac ganglia are most frequently located. We also measured imaginary values at the level of the L2 vertebral body based on existing recommendations and the results of clinical anatomical study [
6,
7]. As a result, all imaginary parameters had significant positive linear correlations with BMI.
The calculated imaginary needle trajectory distance ranged from 10.6 to 11.1 cm in all patients. Accordingly, it is appropriate to use a straight needle of 10 to 12 cm length when the procedure is performed. If using a bent tip needle, it may be sufficient to use a needle of 10 cm length except overweight patients because imaginary needle trajectory distance and angle of needle may be smaller than using a straight needle.
We found that the safe range of measured imaginary oblique angle was 25°-35° except in the three metastatic cancer patients. The safe range of the measured imaginary oblique angle stretched from the minimum oblique angle (∠DBE), which is related to avoidance of needle interference with osteophytes or lateral bony structures of the L2 vertebral body, to the maximum angle (∠CBE) that can be safely performed the procedure without injuries to other organs. Ochiai et al. [
20] could perform retrocrural celiac plexus block at the narrower angle of 15° by CT monitoring. However this angle could be possible only under CT guided image. When the procedure was performed with a bent tip needle, we could reach the target point at an oblique angle smaller than the imaginary safe range. We could fix the oblique angle to 20° based on the minimal possible angle on the pre-procedure evaluation of CT abdomen images and the bent needle tip. Accordingly, we could safely performed CPB by a posterior retrocrural approach with a bent tip needle under 20° oblique angle fluoroscopic view. In three of the enrolled patients, the maximum oblique angle was smaller than 25° and the angles of three cases were limited by the kidney. However, all three cases had a minimum oblique angle larger than 20° and did not experience kidney-related complications. Furthermore, the actual distance (GF) from the midline to the actual puncture site utilizing a 20° oblique angle was smaller than 6.3 cm (mean 5.8 cm) in all patients. These results demonstrate that the use of a bent tip needle under a 20° oblique angle fluoroscopic view allows the distance from the midline to puncture site to be much shorter than 7.5 cm.
In addition, there was a significant correlation between BMI and CF, DF, CA, DA, ∠CBE, and ∠DBE. These results show that there is a possibility that the landmarks of procedure are adjusted depending on the BMI. At the same time, there was no significant correlation between BMI and GF. Considering this result, there might be no need to care about BMI when using bent tip needle under a fixed 20° oblique angle fluoroscopic view.
Taken together, the use of a bent tip needle has several advantages. First, in this study, the safe range of the measured imaginary oblique angle was smaller than previous recommendations, and it is possible to successfully perform the procedure using a 20° oblique angle which is smaller than the safe imaginary oblique angle because the needle tip was already bent 10°. Second, because of the shorter needle trajectory distance we are able to use of a shorter needle, which is easier to handle. Third, the described bent tip needle has good controllability in minute change of the advancing needle course.
While CPB was performed in the prone or lateral decubitus position, CT abdomen images were taken in the supine position. Accordingly, the measured values may be different from the values of the actual position at the time of the procedure. However, Weber et al. [
21] reported no significant differences in anatomical measurements between supine and prone CT images.
In conclusion, the results of this study shows that a posterior retrocrural approach of CPB utilizing a bent tip needle under 20° oblique angle fluoroscopic view is safe and accurate. Our findings would help improve the safety of the classic posterior retrocrural approach for CPB.
Fig. 1
Transaxial CT abdomen images of L1 vertebral body at the level of celiac artery and at the uppermost level of the L2 vertebral body. A (A'), the anterolateral part of the L1 vertebral body crossed with a vertical line of the mid portion of the pedicle; B (B'), the upper anterolateral part of the L2 vertebral body crossing the vertical line of the mid portion of the pedicle, not to penetrate the crura; C (C'), the skin surface farthest from the midline to project tangentially to B while avoiding major abdominal organs; D (D'), the nearest skin surface to project tangentially to B while avoiding interference with osteophytes or lateral bony structures of the L2 vertebral body; E (E'), the skin surface crossing the vertical line of the mid portion of the pedicle; F: midline, Rt.: right, Lt.: left.
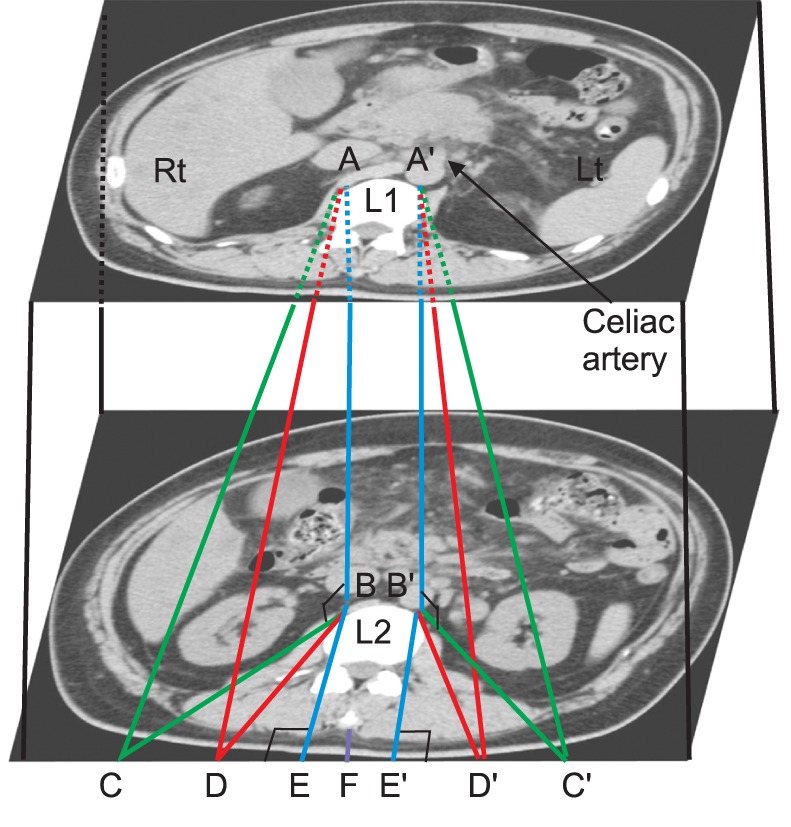
Fig. 2
X-ray fluoroscopy images ([A] Anteroposterior view, [B] Right oblique view, [C] Lateral view) of celiac plexus block by a posterior retrocrural approach that utilizes a 20° oblique angle. G (G'), the actual puncture site; F: midline, Rt.: right.
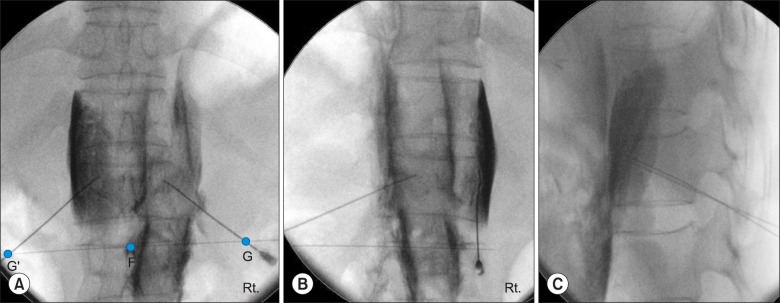
Table 1
Demographic Data
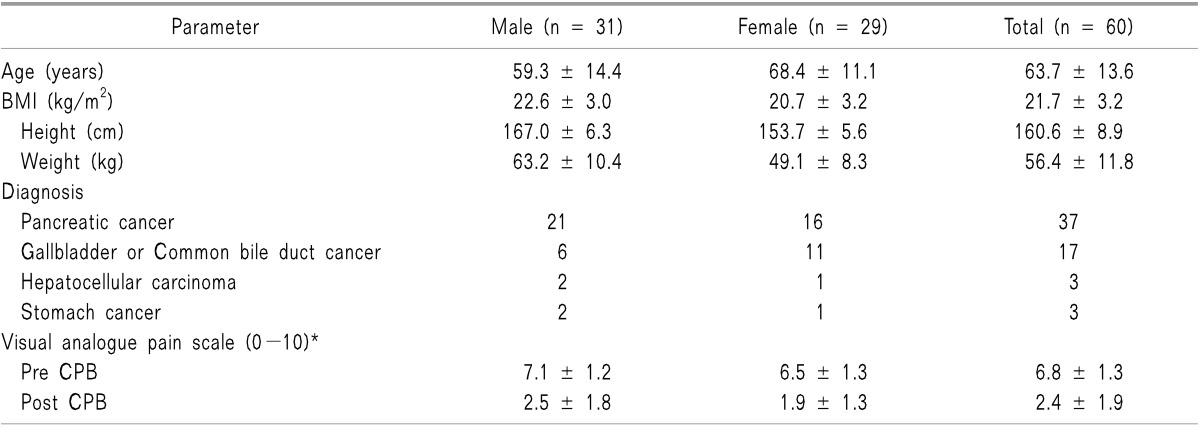
Table 2
Imaginary Puncture Point Distance, Needle Depth, and Needle Angle on CT Abdomen and Actual Puncture Point Distance on X-ray Fluoroscopy (Right/Left, Means ± SD)*
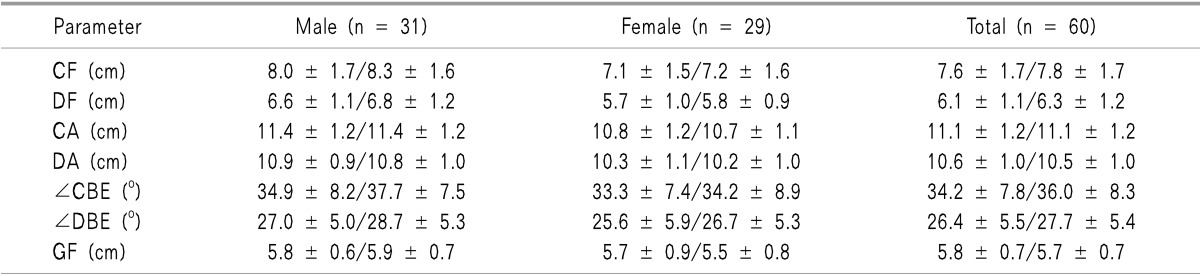
Table 3
Correlation Analysis between BMI and Each Measured Value (Right/Left)




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download