Abstract
Background
Epiduroscopic laser neural decompression (ELND) has been performed as a treatment tool for chronic refractory low back pain and/or radicular pain. There are some studies about the usefulness of epiduroscopy for post lumbar surgery syndrome, however, few studies about the effectiveness of epiduroscopy for patients without back surgery. We compared the satisfaction of patients who underwent ELND for chronic low back pain and/or radicular pain after back surgery and for the same symptoms without surgery.
Methods
We compared the degree of satisfaction of patients after ELND between who had underwent the lumbar spine surgery and who had not retrospectively by chart reviewing. We divided 39 patients who had received ELND into two groups, one is the group of patients who got the lumbar surgery (group 1), and the other is the group of patients who did not (group 2). Their medical records including age, sex, previous treatment, duration of illness, degree of symptom relief were investigated. We compared each items between two groups.
Results
The number of patients in group 1 was 17, and group 2 was 22. In group 1, 16 patients (94.1%) showed more than 'Acceptable', and 19 patients (86.4%) showed more than 'Acceptable' in group 2. There is no significant differences statistically in percentage of patients who showed more than 'Acceptable' in the satisfaction after ELND between two groups.
Go to : 
Chronic low back pain and/or radicular pain are one of major challenges of pain physicians. Various treatment modalities have been presented for chronic low back pain and/or radicular pain. Briefly, treatment modalities for chronic low back pain and/or radicular pain are divided into conservative treatments like physical therapy, pharmacotherapy and interventional treatments, and surgery. Recently, minimal invasive techniques like epiduroscopic laser neural decompression (ELND) have been introduced and used for many cases of chronic low back pain and/or radicular pain [1]. In most cases, patients with chronic low back pain and/or radicular pain receive conservative treatments or interventional treatment like nerve block at first. When it fails, surgery is often considered for next step. However, lumbar surgery has potential risks, especially, refractory chronic back pain which is called post lumbar surgery syndrome and difficult to manage.
ELND is the procedure which observes the epidural space via epiduroscope and removes lesions like protruded discs, adhesions, and fibrosis using by laser. Choy [2] reported about the treatment of lumbar disc herniation by percutaneous laser disc decompression in 1998. Since then, instruments have been advanced and pain physicians have applied the laser during the epiduroscope for the treatment of low back pain and/or radicular pain caused by herniated lumbar disc, adhesions or fibrosis in the epidural space. Most studies focused on the usefulness of epiduroscope for the patients with the post lumbar surgery syndrome [3,4]. However, there are no studies about the usefulness of epiduroscope for the patients with chronic back pain and/or radicular pain who did not get surgery, and only received medications and nerve blocks.
We were interested in the value of epiduroscopy as the treatment modality for chronic low back pain and/or radicular pain before considering surgery. This study is designed for the comparison of the satisfaction of patients who underwent ELND for chronic low back pain and/or radicular pain after back surgery and without surgery.
Go to : 
A retrospective follow-up investigation was conducted according to the medical records of thirty-nine patients who received ELND at the pain center. We performed the ELND for the patients complaining of refractory low back and/or lower extremity pain which was not improved despite any other treatments including medication, epidural steroid injection, and surgery, or in cases of which 50% or more of the pain returned within 1 week in principle. If the patient wanted to get ELND as a first therapy for low back and/or lower extremity pain, we performed ELND at once. Patients who had coagulopathy or who did not want to get ELND were excluded. ELND of all cases was performed by one pain physician. We looked into epidural space by epiduroscope via caudal approach and removed the lesions that caused low back pain and/or radiculopathy by laser. The age, sex, duration of the pain, previous treatments and degree of patients' satisfaction after the procedure were recorded for all patients. The duration of the pain was expressed as years and months. Degree of patients' satisfaction was categorized into 3 stages: 'Good', 'Acceptable', 'Bad' on the basis of the patients' comments stated in the medical records at 4 weeks after the procedure. Patients then were categorized into two groups; patients who had the history of lumbar surgery (group 1), and patients who did not (group 2). Results were represented as means ± SD or number of patients (%). Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Student T-test was used for comparison of age and duration of low back pain and/or radiculopathy before ELND between two groups. And Chi-square test was used for comparison of gender, degree of satisfaction, improvement after ELND between two groups. P values of < 0.05 were considered statistically significant.
Go to : 
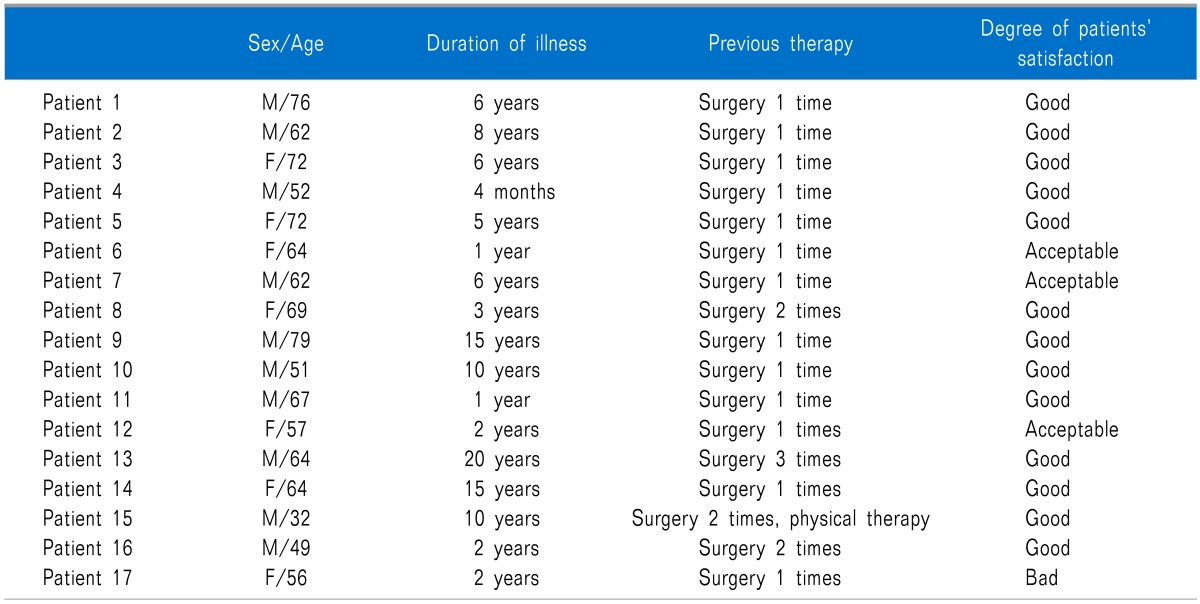
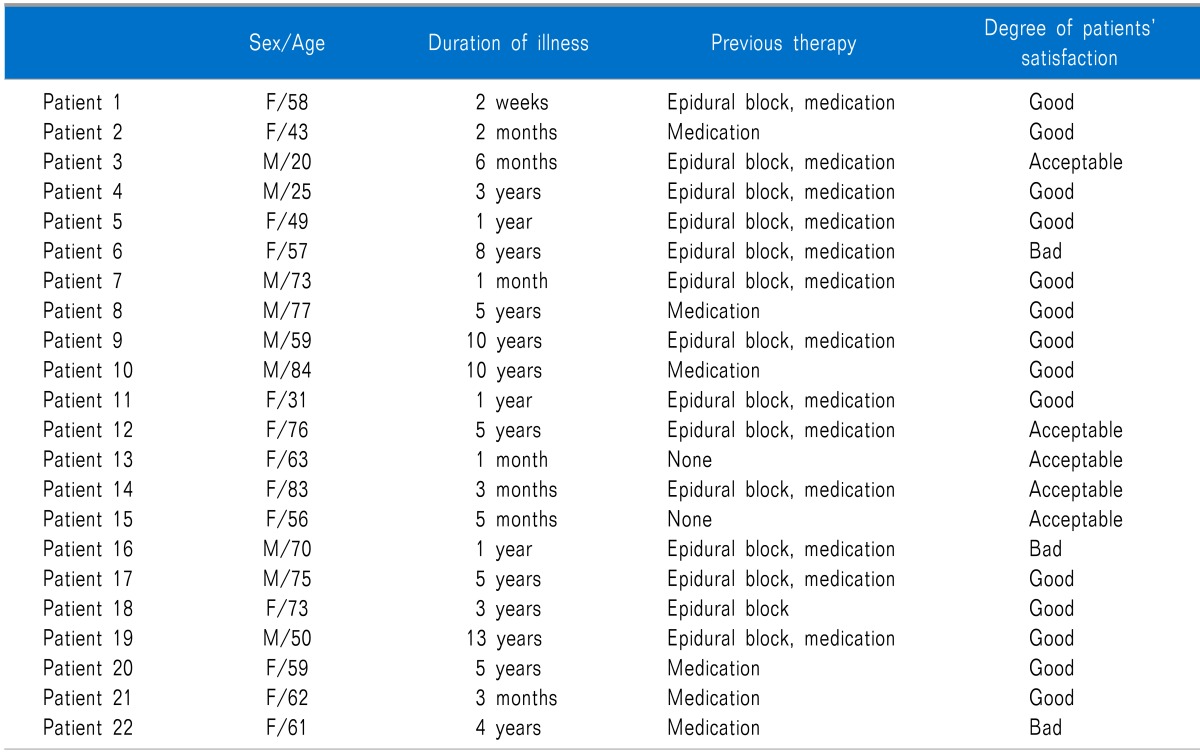
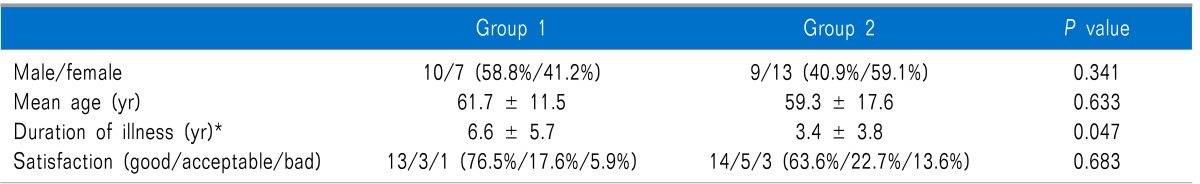
Data of group 1 and 2 patients are demonstrated in Table 1 and 2 respectively. Comparison between two groups is described in Table 3. The number of patients in group 1 was 17, and group 2 was 22. Mean age was 61.6 and 59.3 in group 1 and 2 respectively and mean duration of illness was 6.6 years and 3.4 years in group 1 and 2 respectively. There was no statistical differences in composition of sex and age between two groups, however, mean duration of illness was longer in group 1 (P = 0.047). In group 1, sixteen patients (94.1%) reported the degree of satisfaction as more than 'Acceptable', and nineteen patients in group 2 (86.3%) did. There was no statistical difference in the rate of patients who satisfied with treatment as more than 'Acceptable' after ELND between two groups (P = 0.618).
Go to : 
Patients with chronic low back pain and/or radicular pain have various and complicated causes of pain and sometimes they are refractory to many treatments. Many pain physicians primarily consider the interventional treatments such as epidural block or nerve blocks for chronic low back pain and/or radicular pain. However, the effects of the interventional treatment modalities are sometimes limited in their results.
Although lumbar surgery has been considered as a final treatment option for the low back pain and/or radicular pain, many critical risks including post lumbar surgery syndrome can recur after surgery. Post lumbar surgery syndrome, which was usually called failed back surgery syndrome (FBSS) in the past, means continuous chronic low back pain with lower limb pain even after back surgery, and the incidence of post lumbar surgery syndrome after back surgery ranges from 5% to 50% [5]. Causes of post lumbar surgery syndrome include spinal stenosis, internal disc disruption syndrome, recurrent/retained disc, and neural fibrosis [6].
ENLD has been recently introduced and considered as a new method for the treatment of not only herniated lumbar disc, spinal stenosis, and post lumbar surgery syndrome but also chronic refractory low back pain which is not well responded by other interventional treatments [7]. It is minimal invasive procedure for spine pain using epiduroscope and laser. We can observe the epidural space by epiduroscope as well as remove the lesions like herniated disc, fibrosis, and adhesion by laser. The advantages of ELND comparing with back surgery include relatively non-invasiveness, short operating time, reduction of risks related to general anesthesia, possibility of communication with the patient during the procedure (leading to reduced risks of accidental nerve damage), and short recovery time. However, the usefulness of ELND has not sufficient evidence yet. The more cases and studies are necessary for confirming the definite effectiveness of ELND especially in long term follow-up of chronic low back pain and/or radicular pain patients.
We compared the degree of satisfaction of patients with chronic low back pain and/or radicular pain after ELND who have history of back surgery or who did not. The results were that the more than 85% of patients were satisfied with ELND procedure. Both groups were more than 'Acceptable'. There was no statistical differences between two groups. When we evaluate the degree of pain, we usually use visual analogue scale (VAS). However, it is subjective scale. The degree of VAS change after treatment of pain does not always reflect the degree of satisfaction after treatment exactly. Instead of VAS, we evaluate the therapeutic effect of ELND by asking the degree of satisfaction after ELND directly. Mean duration of illness was longer in group 1. If there was statistically difference of degree of satisfaction after ELND, we had to consider that difference of duration of illness affect the difference of degree of satisfaction between two groups. However, there was no statistically difference of satisfaction after ELND between two groups, and we did not concern about the duration of illness on the difference of satisfaction after ELND. However, we need further study in that point. Some patients received epidural block a few weeks before ELND. However, we just used local anesthetics for epidural block and did not use steroid. So we assume that there is little effect of epidural block on the results of this study.
Major limitation of this study is the small sample size of patients. There are too few patients involved in this study to get statistical power. Short follow up period after ELND is also limitation of this study. ELND is a relatively new procedure for low back pain and/or radicular pain, and there is little data about the result of long-term follow-up after ELND. We surveyed about the result of ELND at 2 and 4 weeks in previous study [1], so we compared the results of ELND between two groups at 4 weeks in this study. However we need further studies for the results of long-term follow-up after ELND. And the evaluation method of patients after procedure is not enough to explain the patients' results in detail. We can only evaluate the degree of satisfaction of patients because we conducted this study by the review of the previous charts. We checked satisfaction of patients after ELND only by asking to them one of three options 'Good/Acceptable/Bad', and it makes us hard to quantify the quality of satisfaction. We did not identify the differences in sex, ages, duration of illness, and previous treatment before ELND including medication, because degrees of satisfaction did not show statistically difference between two groups. We considered that further studies are needed to confirm that epidemiologic factors affect the effectiveness of ELND.
Despite these limitations, it is worth to notice that group 2 revealed more than 85% degree of satisfaction that is similar to that of group 1. We planned this study as a preliminary study at first. Nevertheless, the patients with the chronic low back pain and/or radicular pain which did not respond to previous treatment were improved definitely after ELND in our cases. ELND is a relatively newest treatment tool for chronic low back pain and/or radicular pain and we need more studies to observe the effect of long term period after ELND. In conclusion, ELND may be one option which can give the satisfied results as more than 'Acceptable' for patients with chronic low back pain and/or radicular pain regardless of history of lumbar surgery.
Go to : 
References
1. Jo DH, Yang HJ. The survey of the patient received the epiduroscopic laser neural decompression. Korean J Pain. 2013; 26:27–31. PMID: 23342204.

2. Choy DS. Percutaneous laser disc decompression (PLDD): twelve years' experience with 752 procedures in 518 patients. J Clin Laser Med Surg. 1998; 16:325–331. PMID: 10204439.

3. Ruetten S, Meyer O, Godolias G. Epiduroscopic diagnosis and treatment of epidural adhesions in chronic back pain syndrome of patients with previous surgical treatment: first results of 31 interventions. Z Orthop Ihre Grenzgeb. 2002; 140:171–175. PMID: 12029589.

4. Hayek SM, Helm S, Benyamin RM, Singh V, Bryce DA, Smith HS. Effectiveness of spinal endoscopic adhesiolysis in post lumbar surgery syndrome: a systematic review. Pain Physician. 2009; 12:419–435. PMID: 19305488.
5. Takeshima N, Miyakawa H, Okuda K, Hattori S, Hagiwara S, Takatani J, et al. Evaluation of the therapeutic results of epiduroscopic adhesiolysis for failed back surgery syndrome. Br J Anaesth. 2009; 102:400–407. PMID: 19164308.

6. Slipman CW, Shin CH, Patel RK, Isaac Z, Huston CW, Lipetz JS, et al. Etiologies of failed back surgery syndrome. Pain Med. 2002; 3:200–214. PMID: 15099254.

7. Jo DH, Yang HJ, Kim JJ. Approach for epiduroscopic laser neural decompression in case of the sacral canal stenosis. Korean J Pain. 2013; 26:392–395. PMID: 24156007.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download