Abstract
Background
Epidural steroid injections are an accepted procedure for the conservative management of chronic backache caused by lumbar disc pathology. The purpose of this study was to evaluate the epidurographic findings for the midline, transforaminal and parasagittal approaches in lumbar epidural steroid injections, and correlating them with the clinical improvement.
Methods
Sixty chronic lower back pain patients with unilateral radiculitis from a herniated/degenerated disc were enrolled. After screening the patients according to the exclusion criteria and randomly allocating them to 3 groups of 20 patients, fluoroscopic contrast enhanced epidural steroids were injected via midline (group 1), transforaminal (group 2) and parasagittal interlaminar (group 3) approaches at the level of the pathology. The fluoroscopic patterns of the three groups were studied and correlated with the clinical improvement measured by the VAS over the next 3 months; any incidences of complications were recorded.
Results
The transforaminal group presented better results in terms of VAS reduction than the midline and parasagittal approach groups (P < 0.05). The epidurography showed a better ventral spread for both the transforaminal (P < 0.001) and the paramedian approaches (P < 0.05), as compared to the midline approach. The nerve root filling was greater in the transforaminal group (P < 0.001) than in the other two groups. The ventral spread of the contrast agent was associated with improvement in the VAS score and this difference was statistically significant in group 1 (P < 0.05), and highly significant in groups 2 and 3 (P < 0.001). In all the groups, any complications observed were transient and minor.
Conclusions
The midline and paramedian approaches are technically easier and statistically comparable, but clinically less efficacious than the transforaminal approach. The incidence of ventral spread and nerve root delineation show a definite correlation with clinical improvement. However, an longer follow-up period is advisable for a better evaluation of the actual outcom.
Go to : 
Lower backache is the most common form of chronic pain, with a particular prevalence in the 30-55 age group. Despite the advances in our understanding of the pathophysiology of backache, the pharmacology of analgesics, and the development of more effective techniques, the management of low backache still presents a challenge to pain physicians.
Epidural steroid injections have been used in the treatment of lumbar radicular pain syndromes since 1952. These injections have been performed blind, using an interlaminar loss of resistance technique with a 13-30% incidence of improper localization of the space [1]. The problems encountered with blind epidural injections include erroneous placement of the needle, difficulty in entering the epidural space, the risk of a dural puncture, post dural puncture headaches, a rare but serious risk of spinal cord trauma, and the risk of intrathecal steroid injections causing adhesive arachnoiditis and intravascular injection even after negative aspiration [2].
Epidurography, which was accidently discovered in 1921, is currently used to improve the accuracy of the epidural space localization. Epidurography-aided fluoroscopic injections are now extensively used by spinal interventionists. [2] The fluoroscopic verification of the needle placement and contrast injection has greatly improved the steroid delivery while reducing the risks [3].
Midline interlaminar and transforaminal (TF) lumbar epidural steroid injections (LESI) have been the accepted forms of treatment, especially where the conservative care of low back pain in lumbar disc disease is concerned [4]. In the midline interlaminar approach, the placement of the needle in the dorsal epidural space under fluoroscopic guidance is relatively easy and safe; but the spread of the injectate into the lateral and ventral epidural spaces may be minimal due to the presence of epidural ligaments/scar tissue. Hence, the clinical efficacy is limited [5]. Therefore, the transforaminal approach is more efficacious as it injects the concentrated steroid and anaesthetic solution selectively at the pathologic site or along the DRG. Although considered more target-specific, this approach is associated with several disadvantages including intraneural injection, neural trauma, intravascular injection, and spinal cord trauma [6,7].
The parasagittal interlaminar epidural approach places the drug solution at the lateral most part of the interlaminar space instead of the usual midline interlaminar approach. The drug spreads anteriorly into the ventral epidural space, to the ventrolateral margin of the nerve root and the dura; thus it is associated with an improved clinical outcome [4]. It is also a suitable and reliable alternative to both the transforaminal and midline approaches, which make it difficult to position the needle into the foramina, especially in patients with foraminal stenosis, spondylolisthesis, scoliosis, or previous surgery.
No study has yet compared the fluoroscopic findings and clinical benefits of delivering the drug solution ventrally via the three techniques for epidural injections. Thus, the present study aims to evaluate the epidurographic findings for the midline, transforaminal and parasagittal epidural approaches in the treatment of lower back pain, correlating them with clinical improvement.
Go to : 
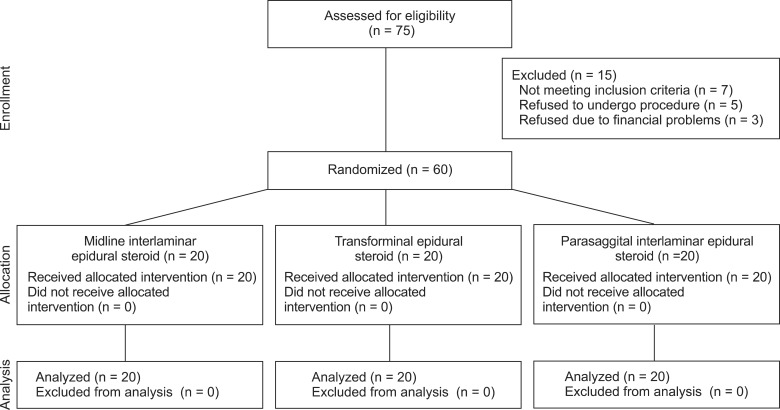
After obtaining approval from the hospital ethics committee, 75 patients between 18 and 70 years old suffering from lower backache due to a discogenic pathology were selected. The inclusion criteria included a unilevel or multi-level unilateral disc protrusion with leg radiation of minimum 4 weeks' duration unrelieved by conventional treatment. Patients with a history of backache without leg radiation, previous spinal surgery, LESI in the past year, allergy to the drugs used, concurrent use of systemic steroid medications, opioid habituation, current pregnancy, and a neurological deficit were excluded. After obtaining the patients' informed consent and applying a thorough selection process (Fig. 1), the participants underwent a clinical evaluation including history-taking, a physical examination, and an MRI of the lumbosacral spine. The level of pain was evaluated using the visual analogue scale (VAS) and the patients' general condition, vitality, diabetes status or the presence of any kind of infection in the body were also assessed.
Accounting for an alpha error of 0.05, sixty patients with low backache were found sufficient to guarantee the 85% power of the study. The 60 patients selected were then randomly divided into three groups of 20 each, using computerized random number generation by author SS (Fig. 1). The intervertebral level and right versus left sides were determined preoperatively according to the clinical examination and diagnostic imaging studies.
All the epidural injections, including contrast and steroid injections, were performed by a single consultant (RG); whereas author SK, who was blinded to the procedure, carried out the observations. These procedures were performed under C-arm fluoroscopic guidance; after the I/V cannula insertion, ringer's lactate was initiated as a maintenance fluid. Minimal mandatory monitoring, including non invasive blood pressure, ECG and pulse oximetry, was carried out throughout the procedure. Mild sedation was provided with 0.03 mg/kg of midazolam.
The patients were placed in the prone position with a bolster placed under the abdomen (between the iliac crests) to reverse the lumbar lordosis and for the comfort of the patient. After fluoroscopic confirmation of the intervertebral level and site of the injection, the skin was anaesthetized with 1% lidocaine.
For the midline approach, the fluoroscopic centering and squaring of the targeted vertebra was achieved with appropriate craniocaudal tilting of the C-arm. Then, a 18 G 3.5 inch Tuohy epidural needle was inserted at the midpoint of the interlaminar space. It was further advanced in the lateral view and guided into the vertebral canal using loss of resistance to air. Similarly, for the parasagittal approach the same protocol was followed except that the entry point was in the lateral most part of the epidural space, and a paramedian end-on orientation was maintained throughout the procedure. After negative aspiration, 1 ml of iohexol 300 was injected to assess the intravascular flush using real time fluoroscopy and the contrast spread in the ventral epidural space. With another 1 ml the dispersal pattern of the contrast, delineation of the nerve roots, and ventral and nerve root filling were observed.
In the transforaminal approach, additionally the image intensifier was oriented in the oblique view (10-20 degree) to attain the Scotty dog image. The marker was placed caudally at the 6 o'clock position of the target pedicle, which is located slightly above the superior articular process. A spinal needle (Quincke 23G) with a slightly angled tip was then directed along the X-ray beam to attain an end-on needle position. The needle was advanced until the final needle-tip target was within the foramen (superior aspect) in the true lateral view. After negative aspiration, the appropriate location of the needle was first confirmed by injecting 0.5 ml of contrast liquid. If paresthesia was encountered, the needle was slightly withdrawn and redirected to the center of the foramen. This was followed by an injection of another 1.5 ml of contrast liquid in order to observe the epidurographic flow patterns.
After confirmation of the needle position, the epidural injection for all the patients was performed using bupivacaine (0.25%), triamcinolone acetate (40 mg), hyaluronidase (1,500 IU) and tramadol (50 mg), with a total volume of 3ml in all three groups. In case the procedure could not be accomplished because of technical challenges, the patients were re-scheduled for the same procedure one week later. The patients who required re-insertion of the needle on the same sitting or a repeat procedure were counted in the number of attempts. After the procedure, the patients were placed in the supine position and their vitals were checked.
After observation in the recovery room, the patients were discharged on the same day with instructions to take ciprofloxacin 500 mg and a combination of aceclofenac 500 mg and serratiopeptidase 15mg thrice daily on a regular basis for five days. They were asked to continue pregabalin 75 mg at night until their next follow-up appointment. All the patients were monitored for periprocedural complications such as paraesthesia, persistent nerve root irritation, numbness, leg weakness, vasovagal attacks, local anaesthetics toxicity, postural headaches, voiding difficulties, hematoma, hypotension, hypertension, bradycardia or tachycardia, and treatment was instituted accordingly.
The post-injection evaluation included a VAS evaluation recorded 1 week, 1 month and 3 months after the injection. The evaluation also took account of the percentage of improvement in the VAS scores. The physiotherapy started as soon as the patients were relieved of the pain.
At the 1 month follow-up mark, the patients were sent to physiotherapy, which consisted in a stretching and strengthening exercise program.
The results of the study were analyzed statistically using a chi square test for non-parametric data and a student's t-test and ANOVA test for parametric data. For the intragroup comparison, a student's t-test was used; for the intergroup comparison, we used an ANOVA and post hoc test.
Go to : 
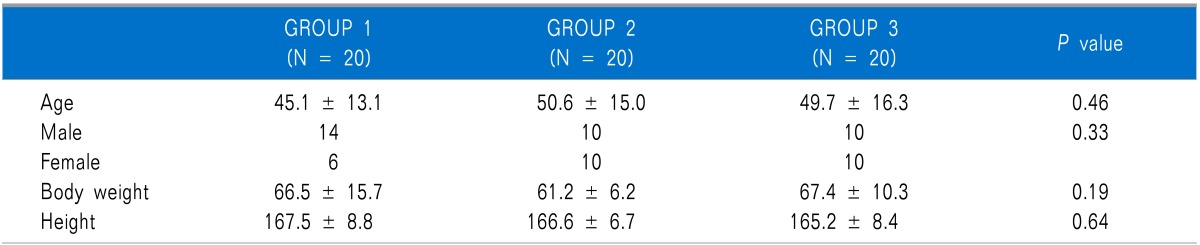
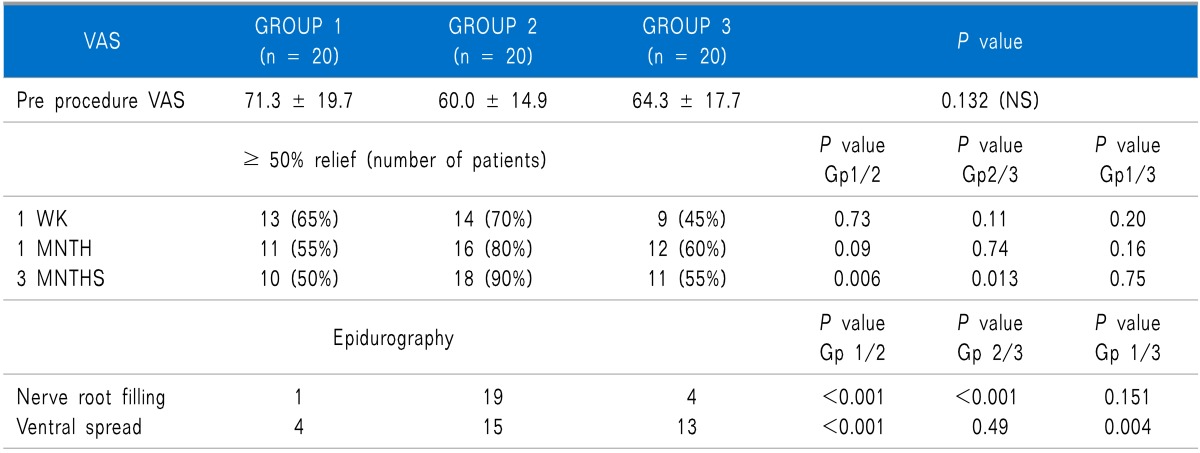
The patients in all three groups were comparable in terms of age, sex, weight, height, MRI findings, and pre procedural mean pain scores (Tables 1 and 2).
A comparison of the number of patients who had experienced a ≥ 50% improvement in their VAS score was done using an ANOVA test. A statistically insignificant but clinically greater number of patients showed a ≥ 50% improvement in their VAS score in group 2 (transforaminal) at the 1 week and 1 month follow-up marks, as compared to the midline and parasagittal approaches. However, at the 3-month follow-up mark, group 2 (transforaminal - 18 patients) showed statistically better results than group 1 (midline - 10 patients) and group 3 (parasagittal - 11 patients). Thus, the patients in the transforaminal approach had better results in terms of reduction of the VAS overall than those in the midline and parasagittal approaches (P < 0.05) (Table 2).
On the epidurography, the ventral spread was statistically comparable for group 2 (transforaminal - 15/20) and group 3 (parasagittal - 13/20), and highly significant for both when compared to that of group 1 (midline - 4/20) (Table 2). The nerve root filling was also significantly greater in group 2 (19/20) than groups 1 (1/20) and 3 (4/20).
As shown in Table 3, the percentage of improvement in the VAS score at the 3-month follow-up mark was studied in those patients in whom ventral spread had been present and was compared with the percentage of improvement in the VAS score of those patients in whom ventral spread had not occurred, using a paired t-test for all three groups. The improvement in VAS percentage was found to be significant in group 1 (midline) and highly significant (P value < 0.001) in group 2 (transforaminal) and group 3 (parasagittal).
The mean number of attempts required to achieve the target site per patient was compared for the three groups. A larger number of attempts had been required in group 2 (transforaminal) than group 1 (midline) and group 3 (parasagittal). The results were statistically significant between group 2 and group 1 (P-0.015) and were insignificant between group 1 and group 3 (P-0.509) and group 2 and group 3 (P-0.185).
The complications experienced by patients in all three groups were only minor and transient. No intrathecal, intravascular injection or other major complications were observed in any of the groups. Upon intergroup comparison, all complications - including numbness, motor weakness, muscle spasms, heaviness etc - were statistically insignificant, except for incidences of allergic reaction to the contrast liquid, which were significantly more prevalent in group 1 (5 patients) than group 2 (0 patient). The allergic reaction observed was not attributable to any particular approach, as this reaction is caused by the patient's intrinsic characteristics.
Go to : 
Lower back pain is an important clinical, social, economic and public health problem affecting the population indiscriminately. Lumbar disc pathology is the most frequent cause. The proposed mechanisms for pain relief in therapeutic LESI include the reduction or dilution of the inflammatory mediators, decrease of the edema, interruption of the pain transmission and possible nerve membrane stabilization [8]. Although epidural injections have enjoyed a long history of efficacy and safety in treating lower back pain as well as lower extremity pain, their use remains controversial.
The conventional midline LESI approach offers the benefits of being a simple, easy and time-tested technique. However, it is currently being condemned because of its documented short-term relief, attributable to the lack of appropriate ventral spread [4]. Further studies from various authors have proposed new techniques and approaches with different time frames but the struggle to find an ideal technique presenting good and long-lasting clinical benefits whilst devoid of any serious potential complications is ongoing.
Our study shows better clinical relief, calculated in terms of the number of patients with a ≥ 50% improvement in VAS score, in the transforaminal group at each follow-up point, than in the midline and paramedian groups. Rados et al. found similar results of a ≥ 50% improvement in VAS Score at the 4-6 weeks follow-up mark, which is comparable to our study [9]. Various other studies have also shown sustained benefits over the long term [6,9,10,11].
The ventral spread ranged from 20% in the midline group, to 75% in the transforaminal group, and 65% in the parasagittal group. However, other studies have shown a much higher incidence of ventral spread, varying between 36% in the midline approach, 100% in the parasagittal approach, and 75-100% in the transforaminal approach [2,4,12]. The various factors responsible could be the volume of contrast liquid used (2 ml in our study vs 5 ml in others), the variation in the techniques, the use of an epidural catheter, and the site of the target in the intervertebral foraminal approach [13]. Nerve root filling indicates the targeted delivery of the drug, thus improving the outcome of the patients. In our study, the highest level of nerve root filling (95%) was observed in the transforaminal group. Manchikanti et al. also found 97% nerve root filling in lumbar transforaminal injections [14].
The clinical correlation of the ventral spread revealed a better outcome in the patients from each group in whom ventral spread of the contrast agent was found. This interrelation had only been previously compared within the transforaminal group, favoring its supero-anterior approach by a retrospective cross-sectional study [15].
Complications such as numbness, motor weakness, allergic reaction to the contrast liquid, or muscle spasms were transient and minor [6,9,16]. We found that the mean number of attempts required per patient to reach the target site was higher in the transforaminal than in the midline and paramedian groups. In the transforaminal group, the direction of the needle towards the target site required more adjustments than in the midline and paramedian groups. However, the needle size being smaller (size 23 G), the muscle spasms and heaviness noted were much lower in the transforaminal group compared to the midline group (Touhy-18 G). However, this difference was statistically insignificant (P > 0.05) among the three groups.
Limitations of the study:
1. One of the study's potential limitations is that the contrast and drug injected were of different viscosity and may therefore have had different epidural flow characteristics. We assumed the contrast flow to be parallel to the drug solution flow.
2. Another limitation lies in the fact that we used the same contrast volume for the three groups so as to maintain similar concentrations. However, using volumes as high as 2 ml in the TF group could lead to a loss of selectivity at the desired pathological site. On the other hand, a volume of 2 ml may not be adequate for ML/PM.
3. It is difficult to differentiate the nerve root filling from the ventral spread, so the final outcome cannot be attributed to a single finding. A large-scale study would be required to categorize only the nerve root filling, ventral spread and combined findings in the three groups and compare them with the clinical outcome.
In conclusion, the midline and paramedian approaches are technically easier and statistically comparable, but clinically less efficacious than the transforaminal approach. The incidence of ventral spread and nerve root delineation show a definite correlation with clinical improvement. However, a longer follow-up period is advisable for a better evaluation of the actual outcome.
Go to : 
References
1. Mehta M, Salmon N. Extradural block. Confirmation of the injection site by X-ray monitoring. Anaesthesia. 1985; 40:1009–1012. PMID: 4061788.

2. Botwin KP, Natalicchio J, Hanna A. Fluoroscopic guided lumbar interlaminar epidural injections: a prospective evaluation of epidurography contrast patterns and anatomical review of the epidural space. Pain Physician. 2004; 7:77–80. PMID: 16868616.
3. McLain RF, Kapural L, Mekhail NA. Epidural steroid therapy for back and leg pain: mechanisms of action and efficacy. Spine J. 2005; 5:191–201. PMID: 15749619.

4. Candido KD, Raghavendra MS, Chinthagada M, Badiee S, Trepashko DW. A prospective evaluation of iodinated contrast flow patterns with fluoroscopically guided lumbar epidural steroid injections: the lateral parasagittal interlaminar epidural approach versus the transforaminal epidural approach. Anesth Analg. 2008; 106:638–644. PMID: 18227326.

5. Rosenberg SK, Grabinsky A, Kooser C, Boswell MV. Effectiveness of transforaminal epidural steroid injections in low back pain: a one year experience. Pain Physician. 2002; 5:266–270. PMID: 16902652.
6. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine (Phila Pa 1976). 2002; 27:11–16. PMID: 11805628.
7. Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009; 12:233–251. PMID: 19165306.
8. Furman MB, Lee TS, Mehta A, Simon JI, Cano WG. Contrast flow selectivity during transforaminal lumbosacral epidural steroid injections. Pain Physician. 2008; 11:855–861. PMID: 19057631.
9. Rados I, Sakic K, Fingler M, Kapural L. Efficacy of interlaminar vs transforaminal epidural steroid injection for the treatment of chronic unilateral radicular pain: prospective, randomized study. Pain Med. 2011; 12:1316–1321. PMID: 21914118.

10. Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic transforaminal lumbar epidural steroids: an outcome study. Arch Phys Med Rehabil. 1998; 79:1362–1366. PMID: 9821894.

11. Smith CC, Booker T, Schaufele MK, Weiss P. Interlaminar versus transforaminal epidural steroid injections for the treatment of symptomatic lumbar spinal stenosis. Pain Med. 2010; 11:1511–1515. PMID: 20735751.

12. Botwin K, Natalicchio J, Brown LA. Epidurography contrast patterns with fluoroscopic guided lumbar transforaminal epidural injections:a prospective evaluation. Pain Physician. 2004; 7:211–215. PMID: 16868594.
13. Choi YK, Barbella JD. Evaluation of epidurographic contrast patterns with fluoroscopic-guided lumbar interlaminar ventral epidural injection. Pain Pract. 2009; 9:275–281. PMID: 19490461.

14. Manchikanti L, Cash KA, Pampati V, Damron KS, McManus CD. Evaluation of lumbar transforaminal epidural injections with needle placement and contrast flow patterns: a prospective, descriptive report. Pain Physician. 2004; 7:217–223. PMID: 16868595.
15. Desai MJ, Shah B, Sayal PK. Epidural contrast flow patterns of transforaminal epidural steroid injections stratified by commonly used final needle-tip position. Pain Med. 2011; 12:864–870. PMID: 21539705.

16. Yang SC, Fu TS, Lai PL, Niu CC, Chen LH, Chen WJ. Transforaminal epidural steroid injection for discectomy candidates: an outcome study with a minimum of two-year follow-up. Chang Gung Med J. 2006; 29:93–99. PMID: 16642732.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download