This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Epidural blocks are widely used for the management of acute and chronic pain. The technique of loss of resistance is frequently adopted to determine the epidural space. A discontinuity of the ligamentum flavum may increase the risk of failure to identify the epidural space. The purpose of this study was to investigate the anatomic variations of the cervical and high thoracic ligamentum flavum in embalmed cadavers.
Methods
Vertebral column specimens of 15 human cadavers were obtained. After vertebral arches were detached from pedicles, the dural sac and epidural connective tissue were removed. The ligamentum flavum from C3 to T6 was directly examined anteriorly.
Results
The incidence of midline gaps in the ligamentum flavum was 87%-100% between C3 and T2. The incidence decreased below this level and was the lowest at T4-T5 (8%). Among the levels with a gap, the location of a gap in the caudal third of the ligamentum flavum was more frequent than in the middle or cephalic portion of the ligamentum flavum.
Conclusions
The cervical and high thoracic ligamentum flavum frequently has midline intervals with various features, especially in the caudal portion of the intervertebral space. Therefore, the ligamentum flavum is not always reliable as a perceptible barrier to identify the epidural space at these vertebral levels. Additionally, it may be more useful to insert the needle into the cephalic portion of the intervertebral space than in the caudal portion.
Go to :

Keywords: epidural analgesia, epidural space, ligamentum flavum
INTRODUCTION
Epidural blocks are widely used for the management of acute and chronic pain [
1,
2,
3]. The technique of loss of resistance is frequently adopted to determine the epidural space. If a needle is advanced along the pathway into the epidural space, an increase in resistance is readily apparent when the ligamentum flavum (LF) is penetrated. A sudden loss of resistance will be encountered when the tip of the needle enters the epidural space [
4].
One of the important problems during an epidural block is the failure to identify the epidural space. The discontinuity of the LF may increase the potential risk of spinal cord injury due to an accidental dural puncture. The incidence of LF midline gaps reportedly increases at the cervical and high thoracic levels compared with lumbar levels [
5,
6]. The purpose of this study was to investigate the anatomic variations of the cervical and high thoracic LF in embalmed cadavers.
Go to :

MATERIALS AND METHODS
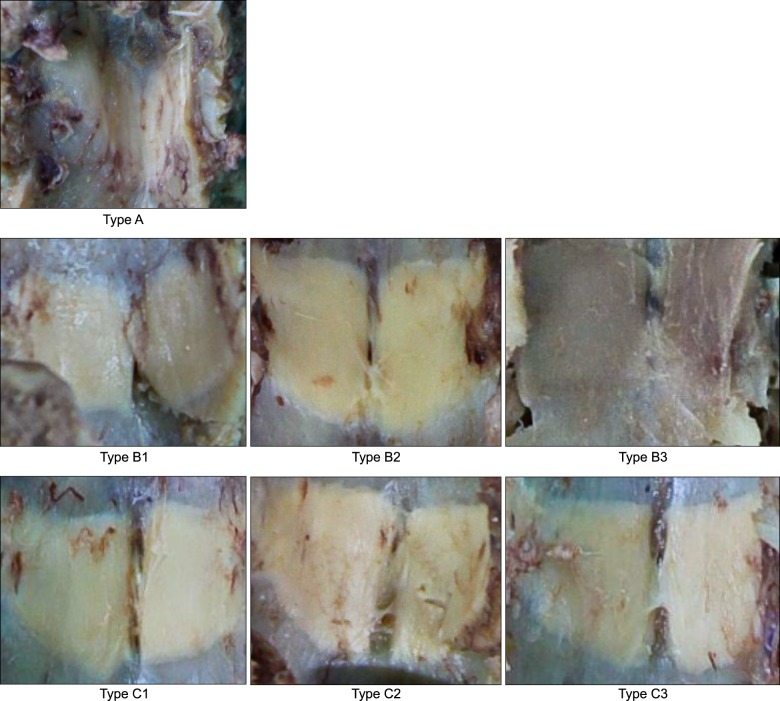
Specimens of cervical and high thoracic vertebral column were obtained from human adult cadavers preserved in a mixture of formaldehyde and carbol (
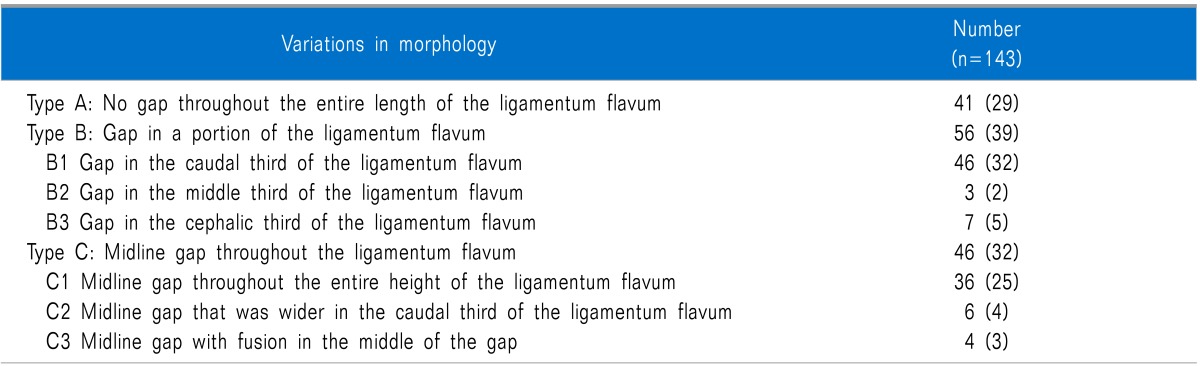
Fig. 1). After vertebral arches were detached from the pedicles, the dural sac and epidural connective tissue were removed. The LF from C3 to T6 was directly examined from the anterior. The gaps of LF in the midline were classified as depicted in
Fig. 2 and described subsequently. Type A was no gap throughout the entire length of LF. Type B was a gap in a portion of LF (B1, gap in the caudal third of LF; B2, gap in the middle third of LF; B3, gap in the cephalic third of LF). Type C was a midline gap throughout LF (C1, midline gap throughout the entire height of LF; C2, midline gap wider in the caudal third of LF; C3, midline gap with a fusion in the middle of the gap).
 | Fig. 1Dissected cervical and high thoracic vertebral column examined anteriorly. Midline gaps of ligamentum flavum are shown. 
|
 | Fig. 2Classification of the midline gap in the ligamentum flavum. Type A is no gap throughout the entire length of LF. Type B is a gap in a portion of LF (B1: gap in the caudal third of LF, B2: gap in the middle third of LF, B3: gap in the cephalic third of LF). Type C is a midline gap throughout LF (C1: midline gap throughout the entire height of LF, C2: midline gap wider in the caudal third of LF, C3: midline gap with a fusion in the middle of the gap). 
|
Go to :

RESULTS
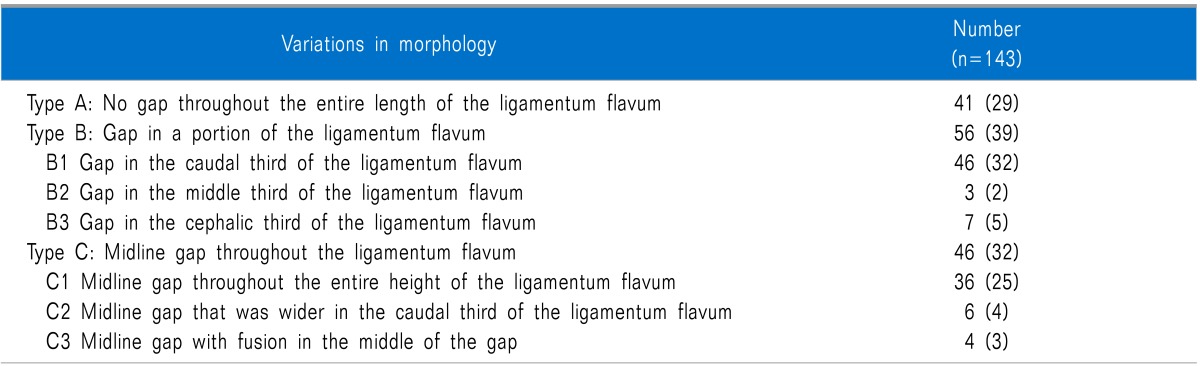
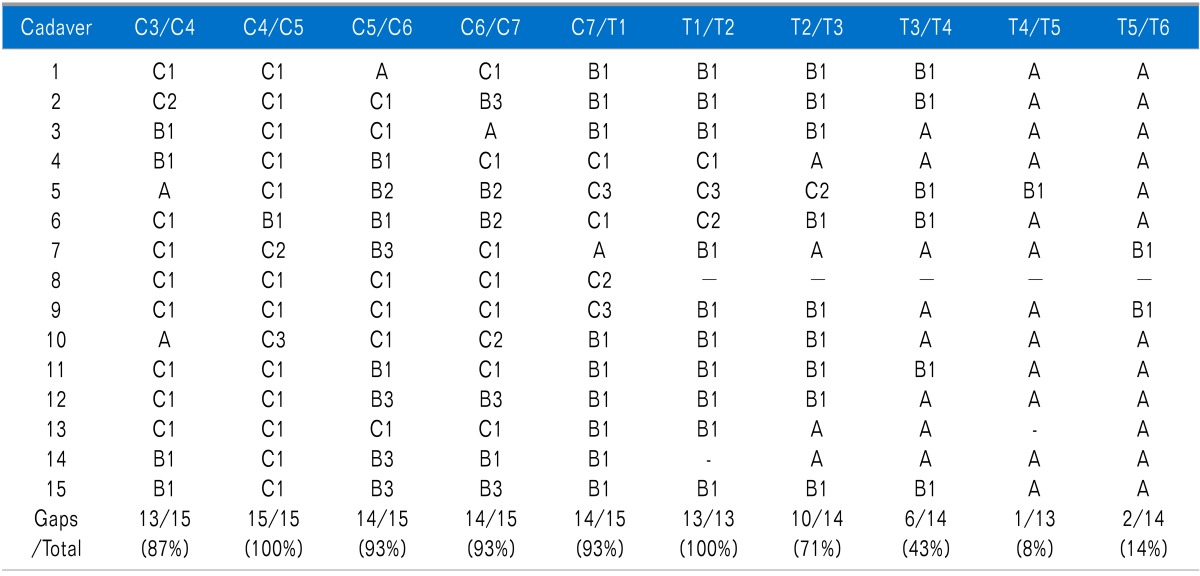
Vertebral column specimens of 15 human cadavers were examined. A total of 150 LF levels were investigated from C3 to T6. Of them, seven levels were excluded from analysis due to damage by pathologic lesion or dissection. The anatomic variations of LF at the investigated levels are shown in
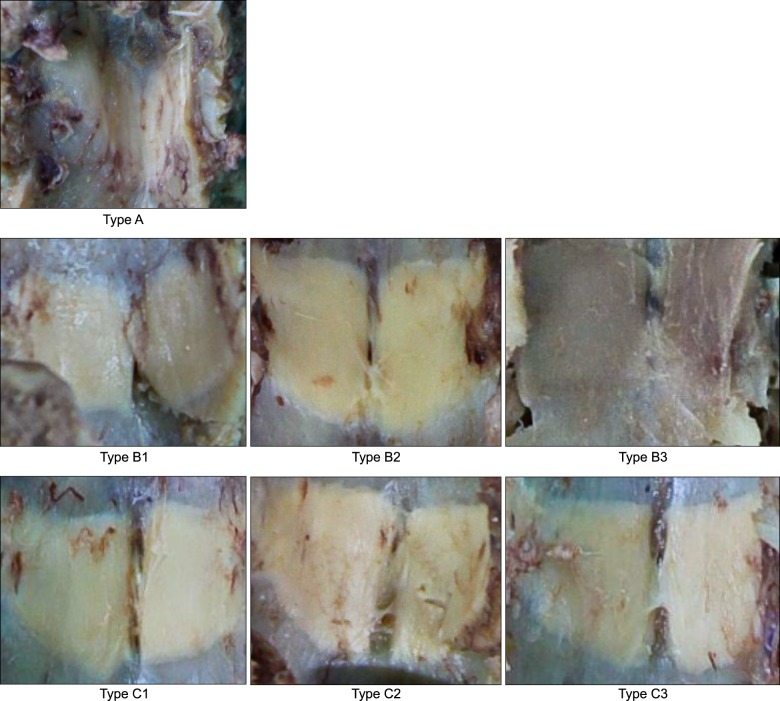
Table 1. Of the 143 investigated levels, 41 (29%) featured no gap, 56 (39%) featured a gap in a portion of the LF and 46 (32%) featured a midline gap throughout the LF (
Table 2).
Table 1
Anatomic Variations of the Ligamentum Flavum at the Investigated Levels
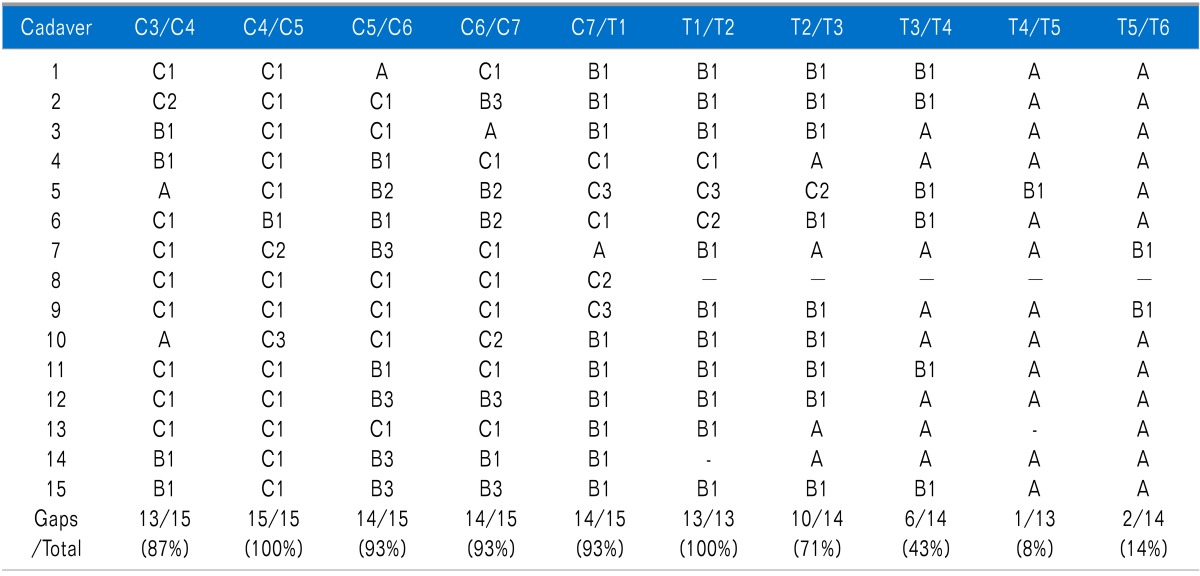

Table 2
Incidences of Anatomic Variations in the Cervical and High Thoracic Ligamentum Flavum

Go to :

DISCUSSION
Epidural blocks with local anesthetics and steroids are widely used in pain clinics due to the effect of rapid pain relief and improved blood circulation. Complications after epidural block include spinal cord injury, hematoma, abscess and transverse myelitis. Of these, the incidence of an accidental dural puncture has been estimated to be not more than 0.5%. However, not to recognize a dural puncture should always be carefully avoided, because an accidental intrathecal injection promptly induces a total spinal anesthesia with loss of consciousness, hypotension and apnea [
7].
The LF connects the lamina of the adjacent vertebra with the vertebral canal. These ligaments are thin and broad in the cervical region, thicker in the thoracic region and thickest in the lumbar region. They have a high content of elastin under tension, which preserves normal curvatures of the vertebral column and assists with straightening of the column after flexing [
8,
9,
10]. Developmentally, LF is a paired structure identified at 12 weeks of gestational age. With growth, the right and left sides of LF fuse in the midline or are partially united with intervals, which permits veins to connect vertebral venous plexuses. In some cases, interspinous ligament fills the intervals [
9,
11].
Incidences of LF midline gaps depending on vertebral levels have been variously reported. Zarzur [
12] dissected 10 lumbar vertebral columns and found that the right and left LF joined in the midline without gaps. However, in another study the gaps were most frequently present at L1-L2 (22%) and were rarer below this level (0-11%) [
6]. The incidence is increased in the cervical and thoracic levels. Lirk et al. [
5,
13] reported that LF discontinued in the midline up to 74% in cervical and up to 35% in thoracic levels. Incidences were reported to be the highest at C5-C6 and T10-T11.
In our study, most of LF between C3 and T2 (87-100%) appeared to have midline gaps. The incidence decreased below this level and was lowest at T4-T5 (8%). All of the 15 harvested specimens had at least one type of gap at any location. The incidences of midline gap seem to be higher in our study than in prior studies. Ethnic differences may be the reason for this discrepancy. However, more studies are needed to clarify this issue.
There were various anatomic features of midline gaps, such as location and shape of gaps. Of all investigated levels, 39% appeared as a gap in a portion of the LF and 32% appeared as a midline gap throughout the LF. Among the levels with a gap, the location of a gap in the caudal third of the LF was more frequent than in the middle or cephalic portion of the LF. Therefore, a midline approach for a cervical and high thoracic epidural block could pose a potential risk of failure to recognize a loss of resistance. The risk could be further increased if the needle is inserted into the caudal portion of the intervertebral space.
We investigated the anatomy of LF in embalmed cadavers. It is unclear if the gaps of embalmed cadavers would result in an actual difficulty to identify a loss of resistance in the clinical practice. However, several clinical studies have shown the advantage of a paramedian approach to identify the epidural space. Joo et al. [
3] monitored intra-needle pressure changes at the moment of entering the epidural space during cervical epidural block. They found that the absence of an abrupt pressure decrease was more frequently observed when using the median approach compared with the paramedian approach (51.5% vs.17.6%). Blomberg et al. [
2] reported that the paramedian approach was associated with a lower frequency of difficulties in the identification of the epidural space for a lumbar epidural block than the midline approach. The gaps in LF could be one of the reasons for these absences of a loss of resistance.
There are some limitations of this study. First, we could not eliminate potential artifacts resulting from the embalming process. There is a possibility of shrinking and loss of water in the tissue of cadavers, which could lead to structural differences between living bodies and cadavers. However, it is unlikely to be an important factor, because changes due to an embalming process usually have a minimal effect on the routine investigation of structural pathologies [
14]. Another limitation is the possibility of any damage to the LF during the dissection, although we performed all dissections with great care. Also, the small number of specimens could be a limitation of this study.
In conclusion, the cervical and high thoracic LF frequently has midline intervals with various features, especially in the caudal portion of the intervertebral space. Therefore, one should keep in mind that the LF is not always reliable as a perceptible barrier to identify the epidural space at these vertebral levels. Additionally, it may be more useful to insert the needle into the cephalic portion of the intervertebral space than in the caudal portion.
Go to :






 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download