Abstract
Amputation neuroma can cause very serious, intractable pain. Many treatment modalities are suggested for painful neuroma. Pharmacologic treatment shows a limited effect on eliminating the pain, and surgical treatment has a high recurrence rate. We applied pulsed radiofrequency treatment at the neuroma stalk under ultrasonography guidance. The long-term outcome was very successful, prompting us to report this case.
Symptoms following dismemberment include phantom limb sensation, phantom pain, and stump pain [1]. Stump neuroma, which is one of the causes of stump pain, is a non-neoplastic proliferation located at the terminals of the damaged nerves that occurs as part of the normal nerve damage recovery process, and is usually found one to twelve months after amputation [2]. When pulsating burning, cramping, pricking, and electric shock-like pain persist after the initial recovery stage, stump neuroma should be suspected [1]. In the case we report, pulsed radiofrequency treatment was considered as a treatment method by virtue of its low neuroma recurrence rate and low risk of complication after the procedure. The treatment was performed on a patient who complained of a pain due to stump neuroma which was not controlled by a conservative treatment.
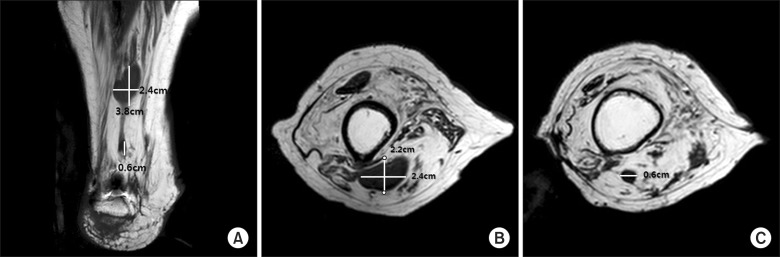
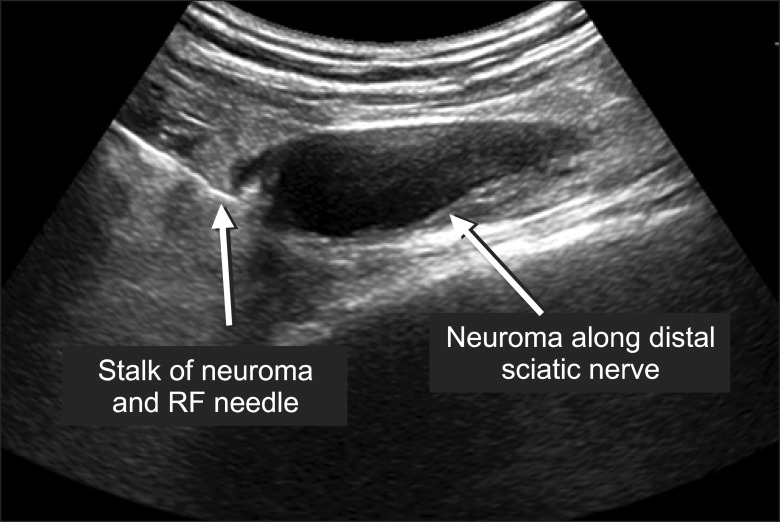
A 75-year-old male patient who had undergone above-knee amputation 50 years before visited the institution with a chief complaint of pain in the right leg stump, which had been exacerbated in the past 30 years. The underlying diseases of the patient were hypertension, atrial fibrillation, bronchial asthma, and lumbar spinal stenosis. At the time of the visit, the patient scored 8-9/10 on the visual analogue scale (VAS). Even though his orthosis had been re-adjusted many times, the incidence of a breakthrough pain had increased and the patient had therefore become unable to wear it. The physical examination did not reveal any infection or ulcer at the stump, but a palpable mass was found. The Tinel's sign test proved positive. Magnetic resonance imaging (MRI) revealed the first neuroma measuring 8 × 2.4 × 2.2 cm at the proximal part of the sciatic nerve and the second one of about 0.6 cm at the proximal part of the tibial nerve, 2.8 cm below the first neuroma (Fig. 1). 1% lidocaine 5 cc was injected under ultrasound guidance around the neuroma [3], following which the pain was decreased (VAS 2-3/10) and the symptoms evidenced by the Tinel's sign test disappeared. The plain radiograph did not permit any particular findings. In order to differentiate stump pain caused by neuroma from radiating pain caused by lumbar spinal stenosis, an electromyography (EMG) and a nerve conduction velocity (NCV) test were performed. The results showed that bilateral radiculopathy was mainly confined to the left side, while the right leg pain was localized to the stump, and the decrease of the stump pain from the ultrasound-guided injection of the local anesthetic was significant. Therefore, the patient was diagnosed with stump pain from stump neuroma and was subsequently referred to the Department of Orthopedics to receive surgical treatment. However, considering the high recurrence rate after excision of a neuroma, the potential complications of massive dissection, and the associated difficulties in the recovery of the damaged stump, a conservative treatment was recommended instead. Although codeine phosphate 20 mg/d, Ibuprofen 400 mg/d, acetaminophen 500 mg/d, and gabapentine 600 mg/d were administered for two weeks, there was no improvement in the symptoms. Rather, side effects from the drugs became manifest, and the drug treatment therefore had to be discontinued. In light of this, we decided to perform ultrasound-guided pulsed radiofrequency ablation at the first neuroma stalk of the sciatic nerve. Under ultrasound guidance, a 10 cm-long needle with a 5 mm active tip was installed as closely as possible to the distal part of the sciatic nerve neuroma stalk [4], whose diameter was about 6 mm (Fig. 2). After 3 mL of 0.5% mepivacaine HCL were injected, pulsed radiofrequency ablation was performed three times at 42℃ for 120 seconds each, and 10 mg triamcinolone were then injected. One week after the pulsed radiofrequency ablation, the Tinel's sign test was negative, and the patient's pain had decreased to a VAS score of 2-3/10. In particular, the incidence of the breakthrough pain which occurred when the patient wore the orthosis was decreased to a level of 30% or less, and the VAS score was also significantly decreased to 4-5/10. The effect of the pulsed radiofrequency ablation has persisted without any exacerbation of the symptoms during the follow-up period of the past six months.
The patient in this case report did not receive any particular treatment for the stump pain which had first become severe 20 years after his above-knee amputation. When the patient became unable to wear the orthosis due to the exacerbated pain, he visited the Pain Clinic. On the basis of the results of the tests performed during his visit, he was diagnosed with stump neuroma. His pain was decreased by about 70-80% after pulsed radiofrequency ablation was performed at the neuroma stalk. This case was therefore a successful one. In the case of dismemberment, the tunnel through which the axon fiber of the proximal part is extended is not formed by Schwann cells, and neurotrophins are not generated. As a result, the axon fiber of the proximal part may extend in random directions to form a bulbous neuroma [5,6]. The case where transplantation of a toe to an amputated finger with a painful neuroma not only recovered the functions of the hand but also eliminated the pain caused by the neuroma supported the hypothesis that neuroma is caused by the loss of a target organ to which the axon fiber of the proximal damaged nerve extends [7]. However, since a case has been reported in which a neuroma was caused even after a diagnostic biopsy of the nerve, it is presumed that many mechanisms are involved in the formation of a neuroma [5]. Ultrasound enables us to examine the abnormalities of a soft tissue which are not visible through magnetic resonance imaging (MRI) or computerized tomography (CT) due to the compactness of the tissue [6]. The ultrasound technique also makes it possible to verify inflammatory changes such as fluid collection in a soft tissue. Ultrasound may be used to verify the correlation between a neuroma and a proximal nerve, to determine the surgical range in a surgical approach so as to minimize dissection, and to perform diagnostic nerve block through injection of a local anesthetic, as well as neurolysis through injection of a neurolytic such as phenol. Nerve fiber growth may be inhibited by the injection of alcohol, steroid, formalin, pepsin, nitrogen mustard, hydrochloric acid, and phenol, and the repeated injection of procaine to a neuroma is also recommended for pain oppression [5]. In a surgery, ligation, electrocautery, and freezing of the nerve stumps are employed to reduce the size of the neuroma, and a laser-based method has recently been found effective [5]. In a case report where the decrease in the VAS score was compared after a surgical neuroma excision and after ultrasound-guided neurolysis, the VAS score appeared to be decreased more significantly after ultrasound-guided neurolysis [8]. There is a case report in which stump pain was effectively treated through neurolysis of a stump neuroma stalk by using a neurolytic. However, in the study on neurolysis of a stump neuroma stalk by using phenol, it was reported that the dose of the used neurolytic affected the result. Therefore, the use of a large amount of neurolytic was considered as a potential successful treatment for the giant neuroma in this case. However, determining the dose of an appropriate neurolytic was difficult, and possible side effects such as local soft tissue necrosis caused by a neurolytic were also an important concern [9]. Although there is no existing case-to-case comparative study comparing the use of a neurolytic with pulsed radiofrequency ablation in the treatment of pain caused by a stump neuroma, there is a case in which pulsed radiofrequency ablation was performed on the Morton`s neuroma patient group, which is a subject group for a surgical treatment, and the VAS score was decreased by more than 70% in 85% of the patients [10], as well as a case in which pulsed radiofrequency ablation performed for the treatment of a stump neuroma produced excellent results [1]. Since pulsed radiofrequency treatment is a non-neurodestructive method, we assumed that pulsed radiofrequency ablation may present a low risk of symptom recurrence due to recombination of the remaining stalks in the ablated distal part with the proximal nerve and the formation of a new neuroma at the neurolyzed terminals, which can occur in the case of neurolysis using a neurolytic. These considerations led us to perform pulsed radiofrequency ablation for the treatment of the stump neuroma [6,7,9]. There are reports of cases in which pulsed radiofrequency ablation was performed directly on a neuroma and results similar to those obtained in this study were obtained; however, there is scarcely a case of pulsed radiofrequency ablation of a neuroma stalk as performed in this case [1].
Dismemberment patients are continuously generated by traffic accidents, industrial accidents, wars and other causes, and their age is very variable. In addition, dismemberment patients often complain of phantom limb, phantom pain, or stump pain. As evidenced in this case, performing ultrasound-guided pulsed radiofrequency ablation on a patient complaining of a dismemberment stump pain may be of great help in decreasing the patient's pain [1].
References
1. Restrepo-Garces CE, Marinov A, McHardy P, Faclier G, Avila A. Pulsed radiofrequency under ultrasound guidance for persistent stump-neuroma pain. Pain Pract. 2011; 11:98–102. PMID: 20642489.

2. Sehirlioglu A, Ozturk C, Yazicioglu K, Tugcu I, Yilmaz B, Goktepe AS. Painful neuroma requiring surgical excision after lower limb amputation caused by landmine explosions. Int Orthop. 2009; 33:533–536. PMID: 17940765.

3. Thomas AJ, Bull MJ, Howard AC, Saleh M. Peri operative ultrasound guided needle localisation of amputation stump neuroma. Injury. 1999; 30:689–691. PMID: 10707244.

4. Ernberg LA, Adler RS, Lane J. Ultrasound in the detection and treatment of a painful stump neuroma. Skeletal Radiol. 2003; 32:306–309. PMID: 12719933.

5. Lewin-Kowalik J, Marcol W, Kotulska K, Mandera M, Klimczak A. Prevention and management of painful neuroma. Neurol Med Chir (Tokyo). 2006; 46:62–67. PMID: 16498214.

6. Provost N, Bonaldi VM, Sarazin L, Cho KH, Chhem RK. Amputation stump neuroma: ultrasound features. J Clin Ultrasound. 1997; 25:85–89. PMID: 9023697.

7. Zhang F, Hu EC, Chen W, Lineaweaver WC. Treatment of painful neuroma of amputated phalanx with distal toe transfer: a case report. South Med J. 2006; 99:85–89. PMID: 16466129.

8. Gruber H, Glodny B, Kopf H, Bendix N, Galiano K, Strasak A, et al. Practical experience with sonographically guided phenol instillation of stump neuroma: predictors of effects, success, and outcome. AJR Am J Roentgenol. 2008; 190:1263–1269. PMID: 18430842.

9. Gruber H, Kovacs P, Peer S, Frischhut B, Bodner G. Sonographically guided phenol injection in painful stump neuroma. AJR Am J Roentgenol. 2004; 182:952–954. PMID: 15039170.

10. Chuter GS, Chua YP, Connell DA, Blackney MC. Ultrasoundguided radiofrequency ablation in the management of interdigital (Morton's) neuroma. Skeletal Radiol. 2013; 42:107–111. PMID: 23073898.

Fig. 1
T1-weighted MR coronal image of right lower extremity. About 3.8 × 2.4 × 2.2 cm sized mass along distal sciatic nerve and proximal tibial nerve, posteirormid thigh. About 0.6 cm sized second small nodular mass along distal tibial nerve (2.8 cm under the upper mass). (A) Coronal view, (B) Sagital view (neuroma along distal sciatic nerve), (C) Sagital view (neuroma along distal tibial nerve).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download