Abstract
Background
Knowledge of the anatomical variation of the vertebral artery has clinical importance not only for the performance of interventional or surgical procedures itself but also to ensure their safety. We conducted a study of the anatomical variation by reviewing multi-detector computed tomography (MDCT) images of the cervical spine from 460 Korean patients.
Methods
16-row MDCT data from 460 patients were used in this study. We observed 920 vertebral arteries. Examination points included level of entrance of the artery into the transverse foramen of the cervical vertebra, origin site of the vertebral artery, course of a vertebral artery with aberrant entrance.
Result
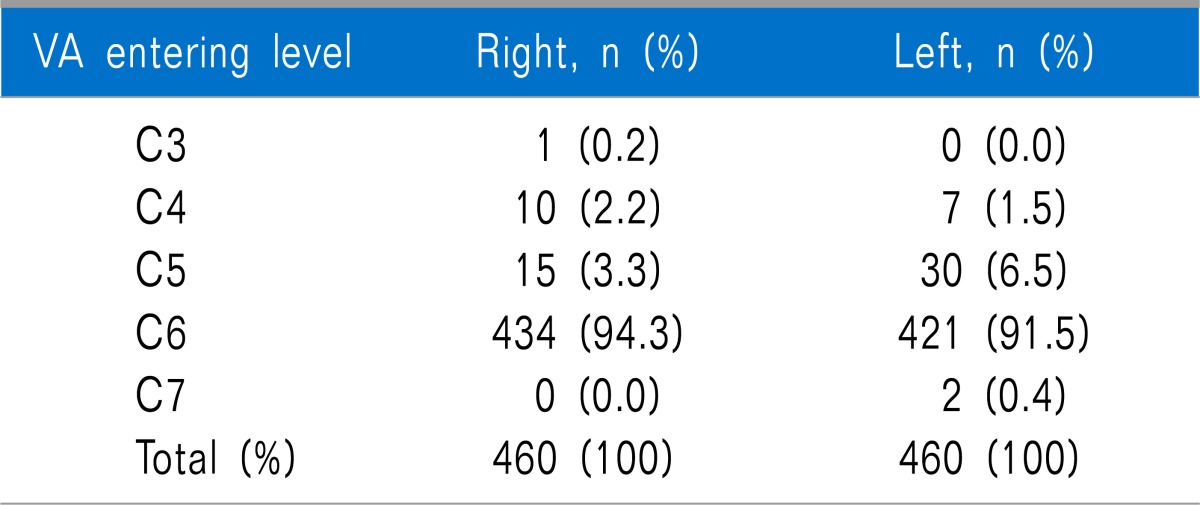
The vertebral artery in 2 (0.2%) cases in this study entered into the transverse foramen of the 7th cervical vertebra from the left. In 45 (4.9%) cases, the vertebral artery entered into the transverse foramen of the 5th cervical vertebra. Of these, the entrance was on the right in 15 (1.6%) and on the left in 30 (3.3%). We found 17 (1.8%) cases in which the artery entered into the transverse foramen of the 4th cervical vertebra, 10 (1.1%) on the right and 7 (0.7%) on the left side. As is commonly acknowledged, the 6th cervical vertebra was the most common site of entry; the vertebral artery entered the transverse foramen of the 6th cervical vertebra in the remaining 855 (93.0%) cases, on the right in 434 (47.2%) and on the left in 421 (45.8%).
Go to : 
Cervical transforaminal epidural block under C-arm guidance is an effective therapeutic intervention in patients with cervical pain. Known complications include infection, hemorrhage, intravascular injection, and damage to the internal carotid vein, internal carotid artery, and vertebral artery. Damage to the cervical vertebral artery usually occurs during operations involving the cervical vertebra, and its incidence is reported to be 0.3-0.5%. Complications associated with an injury to the cervical vertebral artery are arterial dissection, thrombus, vascular spasm, fistula, pseudoaneurysm, cerebral ischemia, and death [1,2,3,4]. The vertebral artery, which originates from the subclavian artery and enters into the intracranial space via the dura mater at C1 after traveling through the transverse foramina of the cervical vertebrae from C6, is a critical artery in perfusion of the brainstem and cerebellum [2]. The vertebral artery is composed of 4 segments: The first segment (V1 segment) begins at the origin on the subclavian artery and extends to the transverse foramen, the second (V2 segment) runs from C6 to the C2 transverse process, third (V3 segment) extends from C2 to the foramen magnum, and the fourth (V4 segment) runs from the dura to the vertebrobasilar junction (Fig. 1). Although anatomical variations in the vertebral arteries have been already reported, these reports are mostly based on Western populations, and there have not been reports on the variation in the Korean population [5,6]. Therefore, this study was conducted to explore anatomical variations of the V1 and V2 segments of the vertebral artery encountered in procedures involving the cervical region in a pain clinic in the Korean population.
Go to : 
Four hundred sixty adult males and females were studied from February 2007 to August 2008 at a single institution. After IRB (201404009) approval, a retrospective study on anatomical variations of the vertebral artery was performed based on data from computed tomography angiography (CT-A). Patients with previously confirmed or suspected vertebral artery disease were excluded from the study. We evaluated the levels at which the vertebral arteries from February 2007 to August 2008 entered the transverse foramina and the presence of a retrothyroid course by using 5 mm-thickness axial planes and 3 mm-thickness coronal planes of 16-row multi-detector computed tomography (MDCT). SPSS (version 20.0) was used for statistical analysis. The chi-square test was used for evaluation of differences in atypical courses between the right and left sides of the vertebral artery, and a P-value < 0.05 was considered to be statistically significant.
Go to : 
The mean age of patients was 65 years, and the male-to-female ratio was 1:1.1. The vertebral artery was observed to enter the transverse foramen at C6 in 434 patients (93.4%) on the right side and in 421 patients (92%) on the left side. In cases of an atypical course of the vertebral artery entering a transverse foramen other than C6, entry was seen on the right side in 26 (5.7%) cases and on the left side in 39 (8%) (Table 1, Fig. 2).
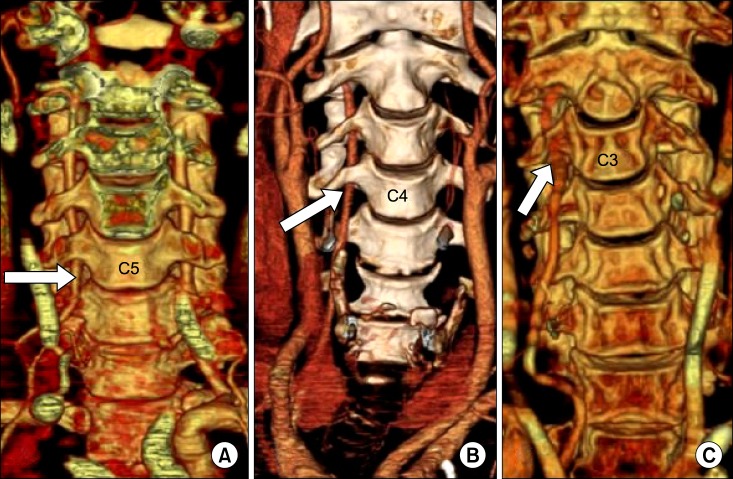
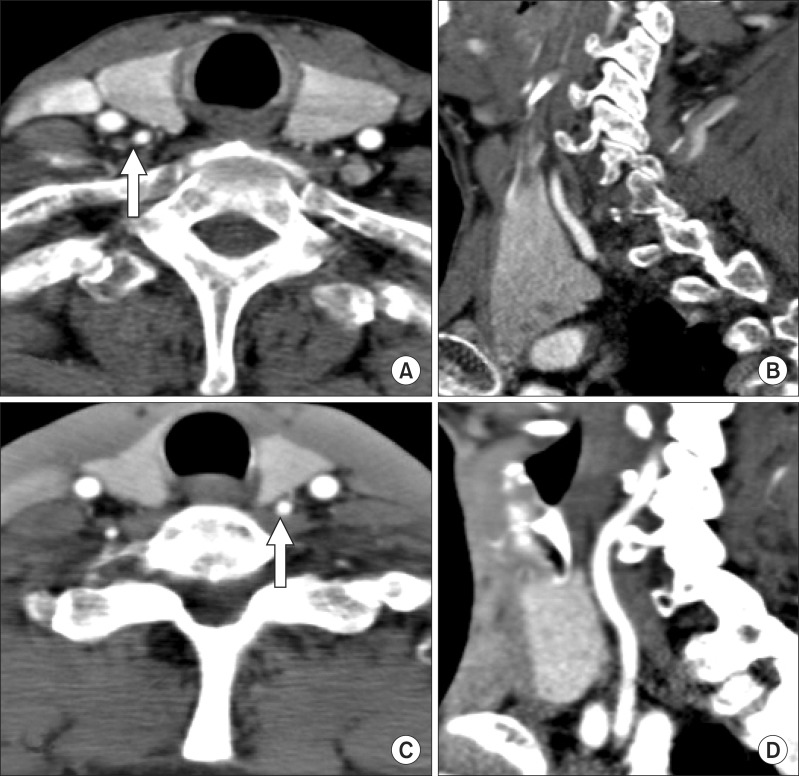
Among 18 of the 26 patients who had atypical courses of the vertebral artery on the right side, a retrothyroid course was evident in 9 out of 15 (80%), 8 out of 10 (2.2%), and 1 (100%) in C5, C4, and C3, respectively (Fig. 3). Five of the 37 patients who demonstrated atypical courses of the vertebral artery on the left side at levels above C6 had retrothyroid courses. Differences in the incidence of atypical course of the vertebral artery between left and right showed no statistical significance (Fig. 3).
Go to : 
This study evaluated the courses of 920 vertebral arteries from 460 Korean participants and concluded that the typical course of the vertebral artery, with entrance at C6, was observed in 92.9% of cases and that an atypical course occurred in 7.1% of cases.
The vertebral artery injury mainly occurs in surgical procedures involving cervical vertebrae and only rarely in selective cervical transforaminal epidural block. However there are a few reports about death in cervical transforaminal epidural block that it is considered a relatively safe procedure [2,3,4]. A recent report from Korea showed a successful selective cervical transforaminal epidural block of C6 under CT guidance in a patient with an atypical course of the vertebral artery known from previously performed magnetic resonance imaging (MRI) [5].
From analysis of MRI and contrast-enhanced CT images, Hong et al. [6] reported that the typical course of the vertebral artery entering at C6 was observed in 95% of cases, a result slightly higher than that of our study, but their findings were identical to our study in that the most common atypical course originated at C5 and that an atypical course of the vertebral artery was more prevalent on the left side. However, in this study, the difference between right and left in atypical course was statistically insignificant. It was confirmed that the anatomical variation of the vertebral artery was variable in its origin from C7 to C3 [3]. Bruneau et al. [7] also reported similar results to those of our study, finding that the typical course, with the artery entering the transverse foramen at C6, was observed in 93% of cases and that the atypical courses varied from C3 to C7.
Due to an increase in the number of patients visiting pain clinics for cervical pain, various types of procedures are being performed according to the causes of the pain. Because procedures usually performed at pain clinics involve cervical levels from C2 to C7, the V2 segment within the transverse foramina is often considered a safe zone in terms of anatomical classification of the vertebral artery. However, as is evident in this study, stellate ganglion block and cervical transforaminal epidural block also require cautionary measures due to atypical courses of the vertebral artery, even though they are widely accepted to be safe procedures. Nucleoplasty, endoscopic anterior discectomy, and microscopic anterior foraminotomy, in particular, are performed in areas anterior to the V2 segment. For example, in cervical nucleoplasty, an introducer needle is inserted into the affected disc at the anterolateral side of neck after securing routes for the needle by manual transposition of the internal carotid artery, esophagus, and trachea under C-arm guidance. From the results of this study, due to atypical courses of the vertebral artery, including retrothyroid courses, operators should be aware that the possibility of injury to the vertebral artery increases when a large diameter needle is inserted into the cervical vertebrae.
Kim et al. [8] explained that the size of the vertebral artery is proportional to the area of the ipsilateral transverse foramen and that significant differences in size between the right and left transverse foramina may indicate hypoplasia or atresia of the vertebral artery or an atypical course of the vertebral artery at a level above. Therefore, if the vertebral artery or transverse foramina show substantial differences in size between the two sides when evaluating MRI or CT images before procedures involving the cervical vertebrae, careful evaluation for an atypical vertebral artery should be performed. Vertebral angiography, CT angiography, and MR angiography can be used to evaluate the course of the vertebral artery.
In conclusion, an atypical course of the vertebral artery in segments V1 and V2 should be evaluated with MRI or CT images before carrying out procedures at the anterior cervical vertebrae.
Go to : 
ACKNOWLEDGEMENTS
This research was supported by the 2014 scientific promotion program funded by Jeju National University.
Go to : 
References
1. Park HK, Jho HD. The management of vertebral artery injury in anterior cervical spine operation: a systematic review of published cases. Eur Spine J. 2012; 21:2475–2485. PMID: 22790563.

2. Rozin L, Rozin R, Koehler SA, Shakir A, Ladham S, Barmada M, et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol. 2003; 24:351–355. PMID: 14634474.

3. Wallace MA, Fukui MB, Williams RL, Ku A, Baghai P. Complications of cervical selective nerve root blocks performed with fluoroscopic guidance. AJR Am J Roentgenol. 2007; 188:1218–1221. PMID: 17449763.

4. Inamasu J, Guiot BH. Iatrogenic vertebral artery injury. Acta Neurol Scand. 2005; 112:349–357. PMID: 16281916.

5. Jung H, Lim JA, Park KB, Hong SW, Kwak KH, Park JM. Computed tomography-guided cervical selective transforaminal epidural block for a patient with bilateral anatomical variations of vertebral artery -a case report-. Korean J Anesthesiol. 2013; 65:468–472. PMID: 24363853.

6. Hong JT, Park DK, Lee MJ, Kim SW, An HS. Anatomical variations of the vertebral artery segment in the lower cervical spine: analysis by three-dimensional computed tomography angiography. Spine (Phila Pa 1976). 2008; 33:2422–2426. PMID: 18923317.

7. Bruneau M, Cornelius JF, Marneffe V, Triffaux M, George B. Anatomical variations of the V2 segment of the vertebral artery. Neurosurgery. 2006; 59:ONS20–ONS24. PMID: 16888547.

8. Kim C, Lee SH, Park SS, Kim BJ, Ryu WS, Kim CK, et al. A Quantitative Comparison of the Vertebral Artery and Transverse Foramen Using CT Angiography. J Clin Neurol. 2012; 8:259–264. PMID: 23323133.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download