INTRODUCTION
C-arm fluoroscope is an important piece of equipment for interventional pain management. It is a very useful tool for safe, precise and comfortable interventional pain treatment. However, its unwanted radiation exposure is inevitable for physicians, nurses and the radiographers of the fluoroscope [
1,
2]. Most studies on fluoroscopic radiation exposure have been on the exposure of physicians [
3,
4,
5,
6]. Although a physician may be the nearest to the radiation source during C-arm fluoroscope-guided interventions, the radiographer is also near the fluoroscope. Several radiographers are shadow gazers, and they have a risk of cumulative radiation exposure during their work. Therefore, it is important to take into consideration the radiation safety of radiographers in C-arm fluoroscope-guided pain interventions.
There are several factors that are related to the radiation exposure of a radiographer such as the physician, distance from the radiation source, skill of the radiographer, time of X-ray exposure, kind of interventional procedure, wearing radiation protection and so on [
1,
2,
6,
7].
We prospectively tested the differences in radiation exposure of radiographers related to their location.
Go to :

MATERIALS AND METHODS
This was a prospective observational study on radiation exposure of radiographers in C-arm fluoroscope-guided interventional management from October 2012 to January 2013. We measured the effective dose (ED) using a portable digital dosimeter on the radiographers' left chest (DPM-127, Hitachi Aloka Medical, Ltd., Tokyo, Japan) and the side of the table (DPM-227, Hitachi Aloka Medical, Ltd., Tokyo, Japan). For measuring the ED, the height of the fluoroscope was adjusted until the operating table was centered between the X-ray generator and the image intensifier [
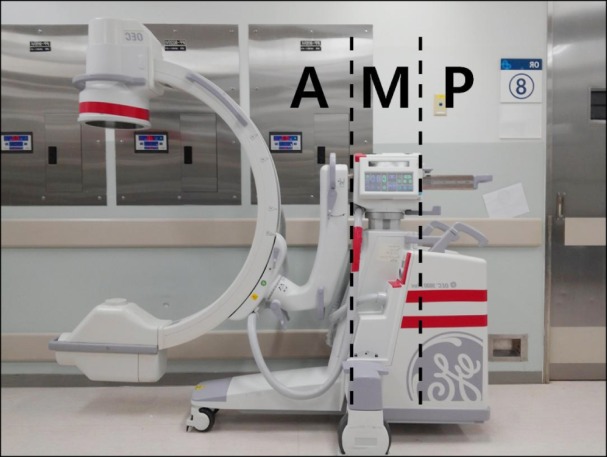
1]. The X-ray field of the fluoroscope was also adjusted at the center of the operating table. In each procedure, we observed the location of the radiographer when the radiographer used the C-arm fluoroscope (OEC 9800PLUS GE healthcare, Salt Lake City, Utah) for the first X-ray image in each procedure, and then, the locations were classified according to Groups A, M and P (
Fig. 1). According to the location of the dosimeter on the radiographer's chest, if it was located besides the mobile support structure of the fluoroscope, the location was M. If it was located in front of the mobile support structure, the location was A. If it was located behind the mobile support structure, the location was P. To maintain a regular distance from the X-ray generator to Groups A, M and P during the procedure, we situated the C-arm of the fluoroscope at the closest position from the mobile support structure shown in
Fig. 1.
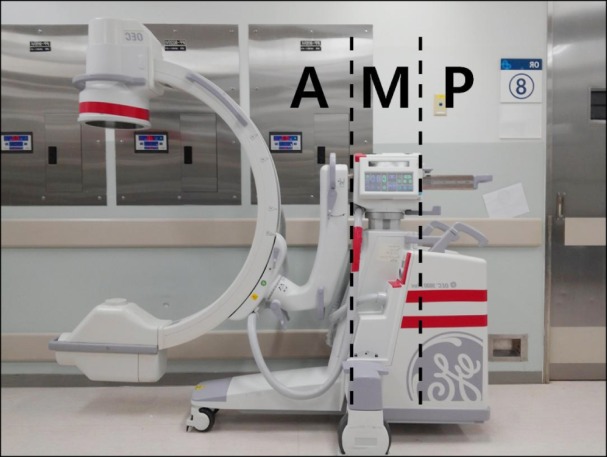 | Fig. 1The Group A, M and P according to the location of dosimeter at radiographer's left chest. 
|
In each procedure, data on age, height, weight, sex, time of X-ray exposure from the fluoroscope, radiation absorbed dose (RAD) from the fluoroscope, and ED at the radiographer's chest and the side of the table were collected.
Statistical analyses were performed on SPSS version 17. Age, height, weight, time of X-ray exposure, RAD, ED and ED ratio (ED on the radiographer's chest/ED at the side of the table) were analyzed by ANOVA and Turkey's multiple comparison tests. Sex was analyzed by chi-square test. A P < 0.05 was considered to be statistically significant.
Go to :

RESULTS
Three hundred and eleven cases were included in this study. There were 51 cases for Group A, 116 cases for Group M and 144 cases for Group P. We performed 55 cases of medial branch block, 50 cases of epidural steroid injection, 137 cases transforaminal epidural steroid injection and 69 cases of other procedures such as radiofrequency treatment, sympathetic ganglion block or neurolysis, vertebroplasty or kyphoplasty, trigeminal nerve block and so on.
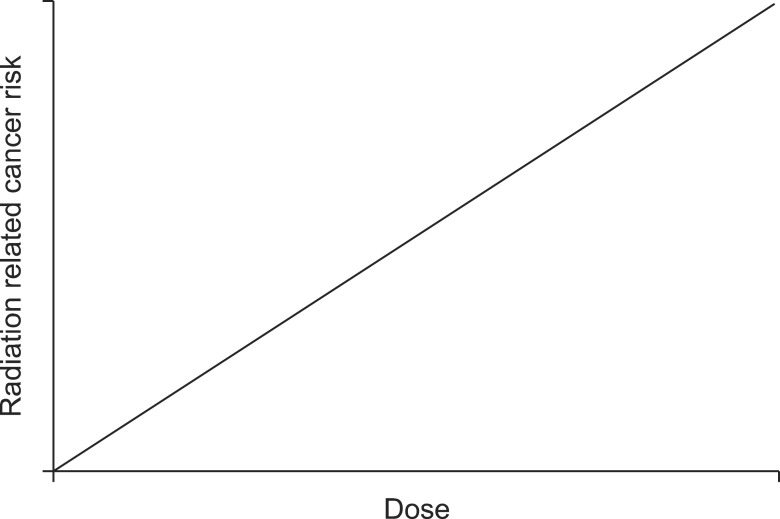
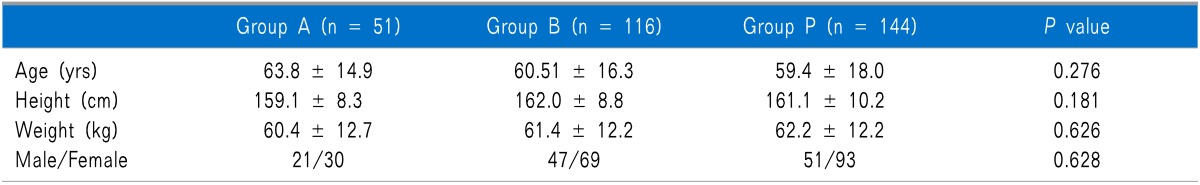
No significant differences were noted in the demographic data such as age, height, weight, male to female ratio, time of X-ray exposure (Group A, 21.1 ± 10.8 sec; Group M, 34.7 ± 53.7 sec; Group P, 30.9 ± 32.6 sec;
P = 0.179), RAD (Group A, 180.5 ± 208.2 radcm
2; Group M, 181.6 ± 205.2 radcm
2; Group P, 154.2 ± 218.9 radcm
2;
P = 0.539) and ED at the side of the table (Group A, 20.7 ± 29.6 µSv; Group M, 24.0 ± 218.9 µSv; Group P, 27.4 ± 51.4 µSv;
P = 0.569) (
Table 1,
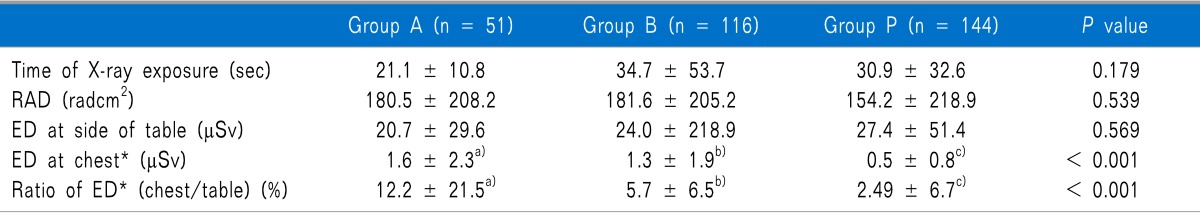
2). There were no statistical differences in ED at the chest between Groups A (1.6 ± 2.3 µSv) and M (1.3 ± 1.9 µSv;
P = 0.344). Group P (0.5 ± 0.8 µSv) had the lowest ED of all the groups (Group A, 1.6 ± 2.3 µSv; Group M, 1.3 ± 1.9 µSv;
P < 0.001) (
Table 2). The ED ratio (ED on the radiographer's chest/ED at the side of the table) of Group A was the highest of all the groups and the ED radio of Group P was the lowest of all the groups (Group A, 12.2 ± 21.5%; Group M, 5.7 ± 6.5%; Group P, 2.5 ± 6.7%;
P < 0.001) (
Table 2).
Table 1
Demographic Characteristics
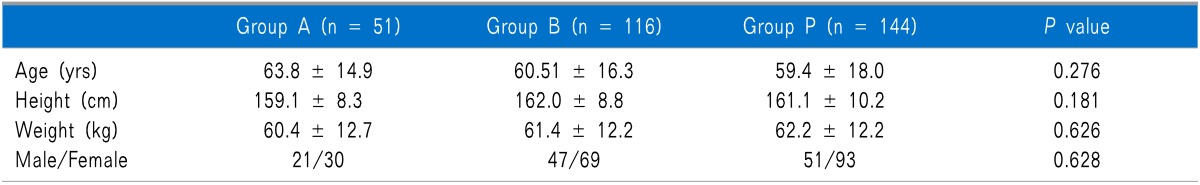

Table 2
Comparisons of Radiation in Each Group

Go to :

DISCUSSION
In this study, the ED ratio of Group P was the lowest and that of Group A was the highest of all the groups. This result means that the distance from the radiation source is an important factor in radiation exposure to radiographers in C-arm fluoroscope-guided pain interventions. The radiation exposure decreased according to the distance from the radiation source. Radiation exposure is inversely proportional to the square of the distance [
6]. It is a simple and important rule in radiation safety. However, radiation is not seen by the naked eye of medical staff. Therefore, most radiographers may not know their exact radiation exposure related to their position. In this study, we did not analyze the radiation exposure of the radiographers according to their exact distance from radiation source but according to their location in front of, besides, and behind the mobile support structure of the fluoroscope classified as Groups A, M, and P, respectively. When radiographers use the C-arm fluoroscope, they do not measure their distance from the radiation source. However, it is easy to know that the position of the radiographer is Group A, M, or P when they use the C-arm fluoroscope. The mean ED ratio of Group M was 46.7% of that of Group A and that of group P was 43.9% of that of Group M. The mean ED ratio of Group P was 20.5% of that of Group A. Therefore, according to the position of the radiographer, the radiation exposure can be decreased by about 80%. The differences in the distance between each group are not large. The distance from the center of the X-ray field to the border of Group A and M was 110 cm. The distance from the border of Group A and M to the border of Group M and P was only 29 cm. One feet (ft) in length is the mean width between the starting point and ending point of one human step. This is 30.48 cm. Let us suppose a certain radiographer stands at the rear of Group A. If he takes a step backwards from the position, his radiation exposure can be decreased by about 53% (the location will change from Group A to Group M). If he takes two steps backwards, his radiation can be decreased by about 80% (The location will change from Group A to Group P).
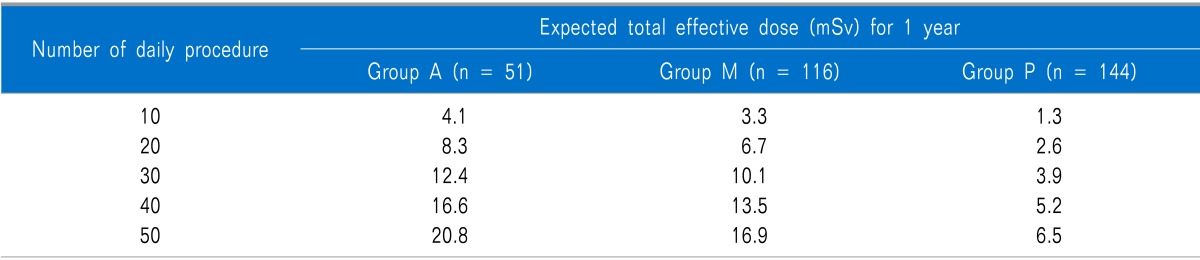
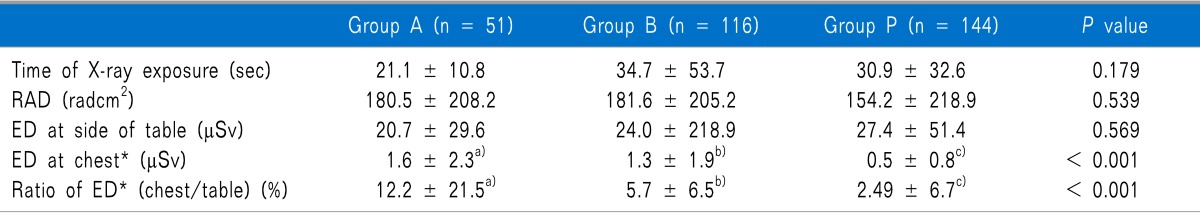
The mean ED at the radiographer's chest per procedure was 1.6 µSv in Group A, 1.3 µSv in Group M, and 0.5 µSv in Group P. If 20 blocks are performed per day from Monday to Friday, the ED at the radiographer's chest could be 6.7 mSv for one year in Group M (
Table 3). The National Council on Radiation Protection and Measurement (NCRP) recommended annual permissible dose for whole body related to occupational exposure is 10 mSv for lifetime exposure, and the accumulation dose for 1 year must not be over 50 mSv in any single year [
8]. If the number of daily procedures in Group A is over 25, the radiation exposure of the radiographer's chest for one year could be over 10.4 mSv. If the number of daily procedure in Group M is over 30, the radiation exposure of the radiographer's chest for one year could be over 10.1 mSv (
Table 3). If the number of daily procedures in Group P is over 80, the radiation exposure of the radiographer's chest for one year could be over 10.4 mSv. In this study, the ED was measured outside of the apron. Therefore, the radiation exposure of the radiographer's chest on the apron could be lower than the ED in this study. In previous studies, some medical workers did not wear a radiation-protective apron, and others only wore a radiation-protective kilt without a vest [
2,
9]. If radiographers do not use radiation-protective devices, their radiation exposure for one year could exceed 10 mSv according to their position and the number of procedures. The most widely used radiation-protective device is the apron [
2,
9]. Although a radiographer wears an apron, radiation exposure of his/her head, eyes, face, neck, hands, feet for one year could exceed 10 mSv according to his/her position and the number of procedures. It is difficult for a radiographer to control the number of daily procedures done. However, he/she can easily control his/her position. Therefore, two steps behind the mobile support structure of the fluoroscope is important for a radiographer during C-arm fluoroscopy guided pain interventions. It is helpful to use a foot-switch or hand-held module to maintain a long distance from the radiation source.
Table 3
Accumulation of Radiation Exposure at Chest for 1 Year According to the Number of Daily Procedure in Each Group

Radiographers are located in an area of relatively low intensity scatter radiation while checking a lateral view of the C-arm fluoroscope [
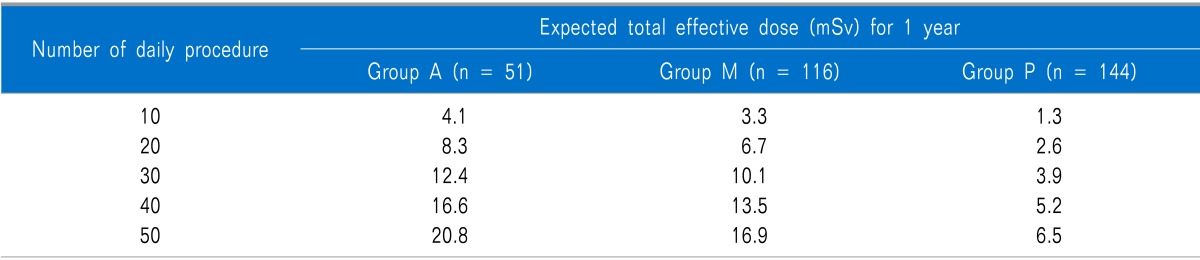
10] because the X-ray generator is the radiation source, and they stand on the opposite side of the radiation source. However, this study shows that the radiographer's accumulation exposure could exceed the annual permissible dose according to his/her position and the number of daily procedures. Although the exposure of the radiographer is lower than 10 mSv per year, this cannot guarantee his/her radiation safety [
11,
12]. The hypothesis of the linear no-threshold (LNT) model introduces the concept on the risk of cancer related to radiation exposure, and the LNT model is the most widely used one [
11,
12,
13] (
Fig. 2). The LNT model assumes that cancer risk increases with the amount of radiation exposure, and there is cancer risk even at low doses [
12,
13]. Although the LNT model is a hypothesis, it shows that minimizing radiation exposure is important in radiation safety.
 | Fig. 2Graph of linear no threshold model. 
|
There have been some previous studies on the radiation exposure of radiographers [
14,
15,
16]. However, we cannot find any studies about the exposure of radiographers especially in fluoroscopy-guided pain interventions. For the radiation safety of radiographers, the main principles are same as that of physicians' radiation safety such as reducing the X-ray time, increasing the distance from the radiation source and using radiation protective gear as shielding [
5,
17]. The methods for reducing radiation exposure are to decrease the fluoroscopy time, decrease the number of fluoroscopic images, use a collimator, use the pulsed or low dose mode, use protective shielding, maintaining a long distance from the radiation source, obtaining the appropriate training and wearing dosimeters (to know personal exposure dose) [
1,
7,
18,
19,
20]. With these methods, radiographers can actively use protective shielding, personal dosimeters, and long distances from radiation sources as measures to reduce radiation exposure. They can also passively control a decrease in the number of fluoroscopic images and in the fluoroscopy time by verifying the correct position of the C-arm fluoroscopy before taking a radiograph.
This study has some limitations. We used the location of the radiographer when the radiographer used the C-arm fluoroscope for the first X-ray image. During the procedure, the radiographer might not stand in one location. It could bias this study. Although the radiographer moved when he/she used the C-arm fluoroscope, his/her location tended to be near of his/her first location. Therefore, we assumed that the radiographer's first location was the standard location. The range of Groups A, M and P was different. In Group P, the radiographer's farther distance from the radiation source could decrease his/her ED by more than the results of this study. However, the radiographer could push the button for a radiograph near the C-arm fluoroscope, and the distance from the radiation source to the radiographer in Group P is limited. In this study, we did not investigate the ED for each kind of intervention. Therefore, the mean ED may be different at other pain clinics. However, the mean ED in this study could be a good reference point for radiographers' exposure. To our knowledge, this is the first study on radiographers' radiation exposure in pain interventions.
In conclusion, radiographers can use several methods to reduce their radiation exposure. With these methods, they can easily reduce their radiation exposure by changing their position. It takes no money or devices to reduce exposure. Two steps behind the mobile support structure of the fluoroscope can effectively decrease the radiation exposure of radiographers by about 80%.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download