Abstract
Background
According to the reports of the World Health Organization 20% of world population suffer from pain and 33% of them suffer to some extent that they cannot live independently.
Methods
This is a cross-sectional study which was conducted in the emergency department (ED) of Valiasr Hospital of Arak, Iran, in order to determine the causes of delay in prescription of analgesics and to construct a model for prediction of circumstances that aggravate oligoanalgesia. Data were collected during a period of 7 days.
Results
Totally, 952 patients participated in this study. In order to reduce their pain intensity, 392 patients (42%) were treated. Physicians and nurses recorded the intensity of pain for 66.3% and 41.37% of patients, respectively. The mean (SD) of pain intensity according to visual analogue scale (VAS) was 8.7 (1.5) which reached to 4.4 (2.3) thirty minutes after analgesics prescription. Median and mean (SD) of delay time in injection of analgesics after the physician's order were 60.0 and 45.6 (63.35) minutes, respectively. The linear regression model suggested that when the attending physician was male or intern and patient was from rural areas the delay was longer.
Go to : 
Pain is a sign of tissue damage and a signal for organisms which need to take action for healing and recovery. According to the reports of World Health Organization, 20% of world population suffers the pain with no reason and 33% of them suffer from pain to some extent that they cannot live independently. In the United States of America the annual expenses of pain related disabilities are about 79 billion dollars [1].
For the first time Wilson and Pendleton introduced the term "oligoanalgesia". It means lack of pain diagnosis or inadequate treatment of pain. This problem has different causes but the main reason is not questioning the patients. Even in cases that physicians ask the patient often they do not trust the patient about the pain intensity [2].
One of the significant problems of physicians in dealing with pain is the lack of courses on dealing with acute pain in their curriculum resources, while just a few hours of teaching can make an important contribution to solving this problem. Physicians consider the pain as a sign to help them in diagnosis and they do not consider it as a separate pathology. However, from the patients' view pain is the most important complaint that needs to be treated quickly [3].
Pain is different from affliction. Affliction is a mixture of both pain and feelings and the related anxiety makes it more annoying for the patient. Poor pain control causes more afflictions and also results in more sensitivity towards the repetition of pain in further bouts; consequently, the patient's affliction regularly increases [4]. In some previous studies, patients' satisfaction had no significant relationship with the amount of pain reduction. The patients' expectations from pain reduction based on the type of disease is related to their satisfaction and those who expect steeper decline in pain, usually are not satisfied with the quality of treatment [5].
Unfortunately, many patients are ashamed of declaring their pain and they believe that it is not good behavior to ask for narcotics [6]. Chronic pain in our region has previously studied [7]. However, acute pain is not sufficiently addressed. Our knowledge about the diagnosis and treatment of pain in emergency departments (EDs) has been developing during the past decade and inadequate treatment of pain has gained more attention. It should be noted that the main cause of visits to EDs is pain which is usually acute [8].
Many studies in different EDs reported that pain was prevalent at the time of visit. One study at France in 2003 showed that 78% of patients had pain when they arrived at the ED and in 54% of them it was acute. Seventy seven percent of the patients had complaints due to inadequate prescription of analgesics and most of them did not get any analgesics during the transfer to the hospital by ambulance or in triage [9].
An extensive study in the United States demonstrated that 78% of emergency visits were due to pain and in 70% of case the intensity of pain was from moderate to acute; however, only 40% of the patients received analgesics. The time between their entrance into the ED and the prescription of narcotics was on average 90 minutes [10]. In another study in Holland, 91% of traumatic patients who attended the ED had pain, while only 19% of them received analgesics of which 60% of cases systemic analgesics were prescribed and 40% only received local analgesics. Two-thirds of patients declared that their pain got worse during the treatment and hospitalization [11]. In another study in the United States, 35% of patients suffered from severe pain even up to 30 minutes after admittance to the ED [12]. Many studies showed that emergency physicians did not precisely assess the intensity of pain, and they usually believed that "pain was whatever the patient mentioned" [13].
Due to the fact that many patients in EDs suffer from oligoanalgesia with its side effects such as stress, atelectasis, release of catecholamines and tachycardia, the experience of hospitalization becomes a nightmare for them. The satisfaction of patients is significantly related with their pain control; however, emergency conditions such as overcrowding, shortage of narcotics, presence of substance abuser patients and many other factors makes it hard to concentrate on pain control as a treatment priority. Therefore, evaluation of implicating factors and determination of a model which predicts conditions that aggravate oligoanalgesia can improve management of patients. Hence, to eliminate the instigating factors in oligoanalgesia and to mend the defects, we decided to assess analgesic administration bottlenecks in our ED and to construct a model for prediction of circumstances that predict why there are delay in administration of analgesics?
Go to : 
In this cross-sectional study, data were collected 24 hours a day during a period of seven days between April 14 and 21, 2013 by three trained interns. The patients who had objective pain and were hospitalized in ED participated in the study after signing an informed consent form. Patients with restlessness or any other problems who did not want to collaborate and those who were still hospitalized at the end of the shift without getting narcotics were omitted from the study. Furthermore, patients who came at the end of a shift so that the follow-up was continued until the next shift were also omitted from the study.
This study was performed in the ED of Valiasr Hospital in Arak, Iran. The Hospital is the oldest and biggest in the city which was established in 1950 with 280 beds and an annual patient turnover of more than 40000. It is a public hospital and is affiliated to Arak University of Medical Sciences. Due to the high number of admissions in the emergency ward, patients are visited frequently with no predetermined time schedule. In most visits a nurse accompanies the physicians and transfers the orders to patients' Kardex. Only written orders are acceptable and depending on the workload and crowdedness there might be a variable lag between the time of order and its actual implementation. In each shift there are ten nurses in the emergency ward and the number does not change in the evenings or holidays.
Based on a study by Todd et al. [10] with a mean time to analgesic application of 90 ± 160.3 minutes and a range of 0-962 min, sample size for this study was estimated 1007 cases but finally 952 cases were collected during the one-week period. The population included all hospitalized patients in ED of Valiasr Hospital who had pain and restlessness during the study. The sampling was performed after settlement of interns of each shift in the emergency room. The intern who was responsible for data gathering registered the first patient coming with objective pain and restlessness as the first sample of that shift. If the patient was eager to participate in the study he/she would have to sign the consent letter and then data were recorded through observation and interview. After the examination of each patient the next patient who was qualified to participate in study was chosen as the next sample. In order to eliminate the possible effect of week-days and different shifts on the quality of data, the samples were chosen during three eight-hour shifts of morning, afternoon and night.
In order to remove the possible problems of data gathering tools and executive problems of study, a preliminary study was performed before data gathering. During this pilot study, the interns in charge of data gathering executed all the tasks under the supervision of the study's main author in three different shifts of morning, afternoon and night and they got familiar with the details of data collection.
The interns in charge of data gathering were available in the emergency during each shift. If the physicians, nurses and other staff were informed of the study's details, then the quality of data would be affected, for instance it would affect the prescription of narcotics; as a result, they were told that the study was about the prevalence and intensity of pain among emergency patients and the staff were unaware about the main objective of the research.
The interns stayed in the emergency ward and each time a patient was visited they recorded the time and checked if any analgesic was ordered. Afterwards, they would stay on alert until the drug was administered by the nurse. The time interval between order and administration were recorded.
In each shift (morning, afternoon, and night) the responsible intern looked after the new comer patients and if a patient had pain and restlessness the intern would assess the pain intensity bases on "Visual Analog Scale" (VAS) of pain intensity. This scale has ten levels. Zero stands for no pain and ten stands for the most imaginable acute pain. Then, according to the patient and his/her accompanying person and studying the patient's file the questionnaire was completed by the intern.
The collected data in this study consisted of background information of the patient such as the cause of hospitalization, age, sex, level of education, place of residence, ethnicity, and some information about the process of health care services in emergency such as the time of hospitalization in emergency, the time of first analgesic order and its type and dose, and the interval between the order and administration. Due to the ever-present shortage of narcotics in emergency wards and especially due to the PRN (Pro re nata) prescription orders, nurses sometimes administer another drugs or the same drug with lower dose or even distilled water, thus the actual injected drug and its dosage was also checked. For patients with loss of consciousness who were not able to answer during monitoring, the pain that needs analgesia was assessed based on increase in heart rate and blood pressure, and sweating, and their response to narcotics were evaluated according to these vital signs. Since many ethnic groups live in Iran, other effective factors in the treatment quality including the patient's language or dialect and the physician's acquaintance with patient's language were also recorded. The number of hospitalized patients in emergency and the number of physicians and nurses in the emergency at admission time were also documented. The prescription protocol of analgesia in our hospital triage was the injection of short-acting narcotics especially "Fentanyl" which has a short half-life and loses effect in a short period. In practice, in triage only those who had fractures got fentanyl before transferring to radiology ward, and after their return and inspection of the X-ray by emergency physician they were transferred to the emergency ward. By this time, the effect of fentanyl had been long gone; consequently there was no need to keep record of prescribed analgesics in triage before transferring to the ED. The record of all consumed drugs in the last 24 hours was kept. The names of specialist, resident, intern and the nurse who had direct contribution to patient's treatment were recorded and then in co-ordination with hospital's training office and nursing office the duration of their work experiences and their fields were extracted. Out of 1007 patients, 952 cases (95.5%) were employed in the study and 55 patients refused to participate.
In this study, "causes of delayed analgesic prescription" is pertaining to the concept of causes of delayed analgesic administration after patients' entrance to the ED until prescription. "Causes of delayed injection after the physician's order" stands for the causes of analgesic injection after physician prescription.
Descriptive statistical analysis for quantitative variables was evaluated by mean and standard deviation and it was assessed for the ordinal and categorical variables by absolute and relative frequency. To determine the relationship between quantitative variables, t-test and one way ANOVA were used. In order to specify the final model of causes of delay in analgesics prescription, the linear regression was used through stepwise method. All variables with P less than 0.2 (consist of patient's gender, age, residential place, ethnicity and triage code and also the physician's working day and shift, besides his/her gender, field of specialty, seniority and working experience) were entered in the model. Finally, according to the highest R2, feasibility and clinical usefulness, some variables remained in the model. All analysis was done by SPSS 20.0.
Go to : 
Totally, of 952 patients who entered the study, 560 patients (58%) did not receive any analgesics and the remaining 392 patients (42%) were treated to relieve their pain. In the treated group, 134 patients (34.2%) were woman. The mean (SD) of participants' age were 37.8 (18.6) years, and 261 patients (66.6%) lived in cities and 131 patients (33.4%) lived in rural area. Certain diagnoses of patients consisted of: general surgery in 91 (23.2%), renal diseases: 41 (10.5%), orthopedics: 66 (16.8%), neurological diseases: 26 (6.6%), neurosurgery: 93 (23.7%) and other diseases in 75 patients (19.1%). Only 61 patients (15.6%) had chronic pain and 331 patients (84.4%) came to the ED due to acute pain. Physicians and nurses recorded the pain intensity in 66.3% and 41.37% of patients, respectively. The mean (SD) of pain intensity according to VAS was 8.7 (1.5), with minimum and maximum of 5 and 10, respectively which reached to 4.4 (2.3) with minimum and maximum of 0 and 10, respectively after 30 minutes of analgesic administration. Median, mean and standard deviation of delay time in injection of analgesics after the physicians order were 60.0, 45.6 and 63.4 minutes, respectively.
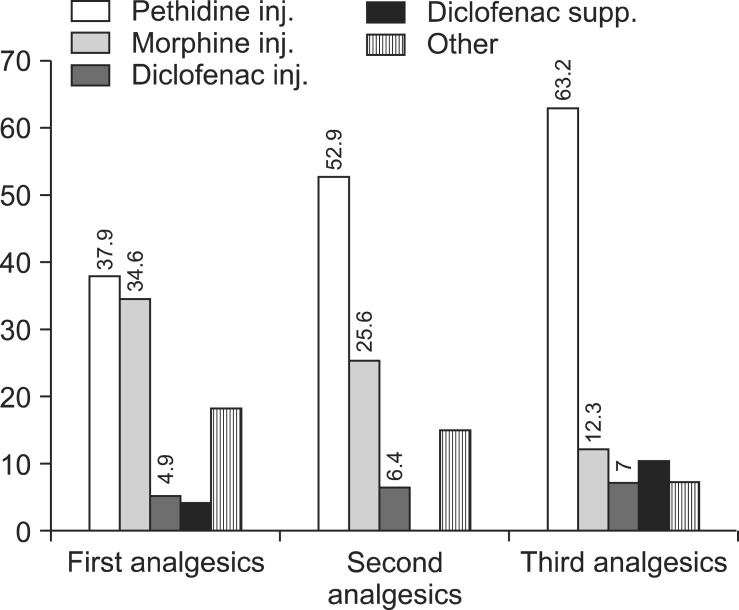
Fig. 1 shows that pethidine was the most prescribed analgesic among others. Moreover, the proportion of pethidine administration from the first stage up to the third stage of treatment had an increasing trend.
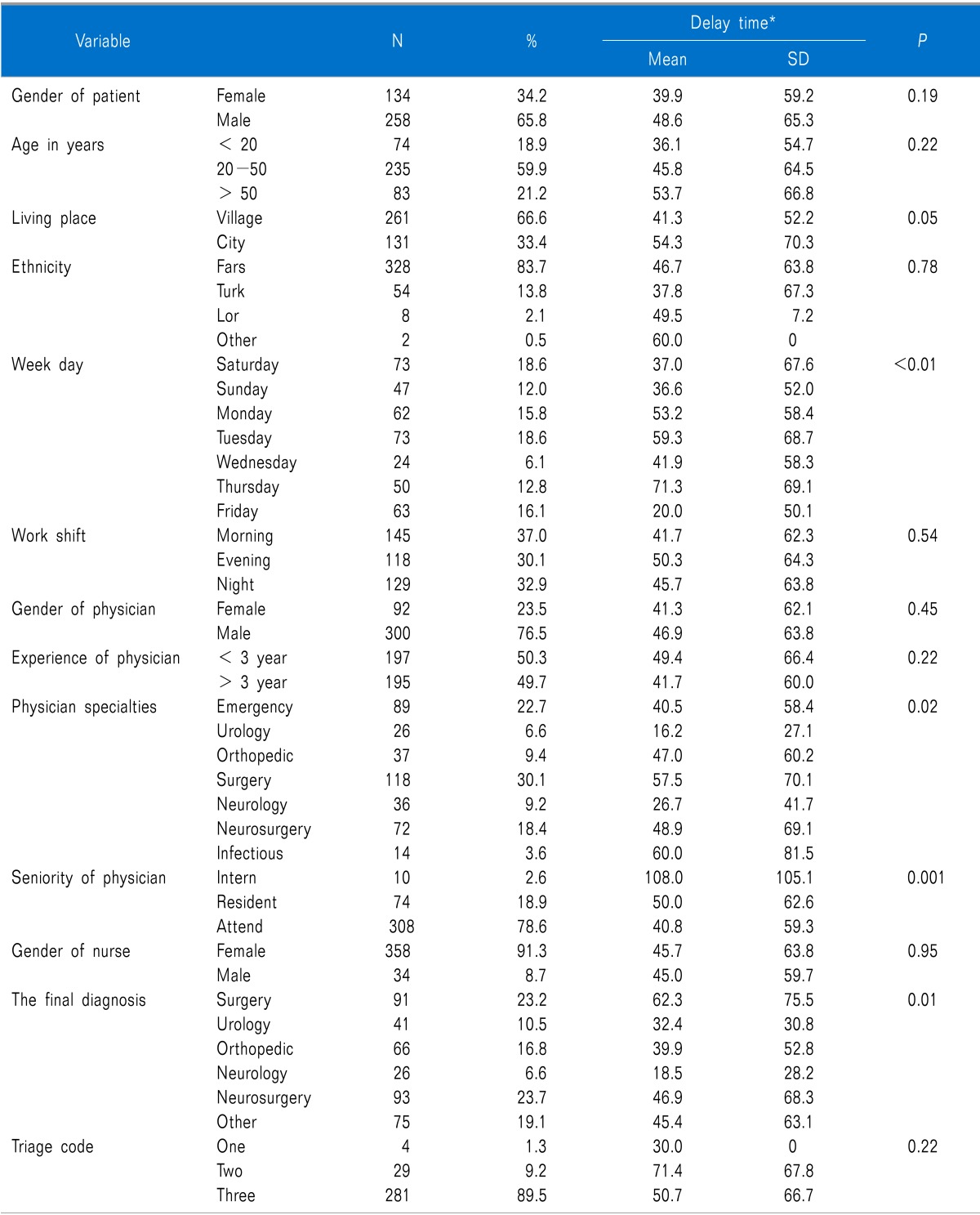
Table 1 demonstrates that there is a significant difference between mean "delayed time between prescription and administration" according to physicians' working day, field of specialty, scientific degree (seniority) and certain diagnoses of disease. In Friday, which is the weekend holyday in Iran, the delay was at its minimum and maximum delay occurred during Thursday (P < 0.0001). The urologists had the least trend in delay and the infectious disease specialists had the highest trend (P = 0.02). Based on seniority, interns had the highest delay and fellows had the lowest trend (P < 0.0001). The minimum delay was related to renal colic patients and the maximum time to administration occurred inpatients suspected of having acute abdomen (P = 0.01). There was also a borderline relationship between residential place and "delayed time between prescription and administration".
Table 2 shows the final model of causes of "delayed time between prescription and administration". This table demonstrates that after elimination of confounding variables' effect, there was statistically significant difference in the mean "delayed time between prescription and administration" only according to the patients' residential place (P = 0.002), physician's scientific degree (seniority) (P = 0.001) and physicians' sex. "Delayed time between prescription and administration" in rural patients was more than urban patients. In comparison to residents and professors, the interns had more delay in treatment and also male physicians had more delay than female physicians. This table also shows that the physicians' scientific degree, physicians' sex and the patients' residential place had more important role in finalizing the model, respectively.
Go to : 
This study showed that the mean and median of "delayed time between prescription and administration" were 45.6 and 60 minutes, respectively. According to the study of Arendts and Fry [14] the median of delay time in analgesics treatment was 53 minutes in an emergency center in Australia. The study of Todd et al. [10] in the United State of America showed that the mean delay time in seven emergency centers of U.S.A was 90 minutes and also the study of Wheeler et al. [15] demonstrated that the mean of this index was 60.0 minutes in an emergency center of New York City. So, the results of this study show that comparing to similar studies, the delay time in this study is better, but in comparison to the guidelines of this field such as British Association of Accident and Emergency Medicine (BAAEM) this study shows that pain management regarding the injection time of analgesics is far from international standards. According to the guidelines of BAAEM all patients with acute pain (VAS > 6) should get an analgesic in less than twenty minutes [16]. Therefore, the reason for this setback in our study should be studied and some actions are needed to resolve the problem.
In this study, there was no significant relationship between the patients' age and delay time; however, many studies including the study of Wheeler et al. [15] in USA showed that between the ages of 10 and 65, with advancing age the delay decreased. In their study, below the age of 10 years and over 65 years the delay increased which was probably due to the fear of side effects on these two age groups or maybe they were not able to clearly describe their pain intensity.
In a study by Lord et al. [17] in Australia there was no difference between men and women. But, in the study of Chen et al. [18] in Pennsylvania the median of delay time among woman was 16 minutes more than men.
In our emergency center the mean of "delayed time between prescription and administration" for men and women were 48.6 and 39.8 minutes, respectively and the difference was not statistically significant. The reason for this difference might be related to the small number of female patients in the women's ward and the high number of traumatic and more critically ill patients in the men's ward.
This study showed that the relationship between the physician's sex and "delayed time between prescription and administration" was not statistically significant in the preliminary test; but, it became significant after elimination of confounding variables. Besides, the distribution of different kinds of prescribed drugs by male and female physicians was different. Female physicians prescribed pethidine for 70.7% of cases and male physicians prescribed morphine for 40.9% of cases. Moreover, different studies including the studies of Marquié et al. [19] and Weisse et al. [20] showed that the relationship between physician's sex and delay time in analgesics injection was statistically significant, with female physicians having maximum delay time for male patients. According to their studies, it might be due to the fact that during the interview with male patients, female physicians were more stressed and they felt that those patients were aggressive; as a result both the physician and patient talked in an offensive tone.
In our study, there was not significant relationship between patients' education and "delayed time between prescription and administration", but in regard to getting or not getting any drugs, patients with academic degree received analgesics 50% more than patients without academic degree and it might be due to their appearance and socio-economical status which made them receive better services. There was also a significant relationship between the patients' education and their satisfaction of analgesia. Those with higher levels of education were more satisfied with emergency services. This could be due to their better understanding of the situation and their lower expectations.
There was also a borderline relationship between the patients residential place and "delayed time between prescription and administration" (P = 0.05). But after the omission of confounding variables this relationship became statistically significant. This variable was one of the few variables which found a place in regression model. "Delayed time between prescription and administration" among rural patients was more than urban patients and it could be due to the cultural differences between the two groups and also due to lower expectations of rural patients from the ED's staff.
In present study, the ethnicity of patients including Fars, Lor, Turk and other ethnicities which included less than 1% of patients was evaluated, and there was no significant relationship between this variable and delay in analgesics prescription. However, the lowest delay time was seen among the Lor patients and that could be due to their culture, probable lower pain threshold, and the usual agitated behavior of their accompanying family members. Several studies including the study of Wheeler et al. [15] showed that there was a significant difference in the delay time between white and black races. Besides, the study of Weisse et al. [20] demonstrated that black women who came to the ED due to renal colic received lower doses of drugs while it was reversed among black men. Ng et al. [21], Iyer [22], Young et al. [23], Kosiński and Siudut [24], Eder et al. [25], and Tanabe et al. [26] reported some differences in the time and manner of analgesics prescription among patients with different ethnicities and races.
In our study, there was a significant relationship between the cause of hospitalization and "delayed time between prescription and administration". Patients who were hospitalized with a final diagnosis of surgical abdomen had the highest delay, since many physicians and nurses believe that patients should not get too much analgesic before any surgeries. Patients hospitalized with a final diagnosis of neurological disease had the lowest delay time. It should be noted that despite the fact that neurosurgeons did not prescribe analgesics, in some cases the emergency medicine physician prescribed analgesics for these patients as needed (PRN) and nurses attended these patients more vigorously. This issue might have been due to the dire situation of most neurosurgery patients.
Similar studies demonstrated that the type of patients' complaint affected delay in analgesics prescription, for example in a study by Arendts and Fry [14] this delay among the non-traumatic patients was more than traumatic ones. Weisse et al. [20] reported that the relationship between the physicians' specialty and delay time was statistically significant.We also discovered that the infectious diseases specialists had the highest delay and urologists the lowest, while some studies including the study of Yee et al. [6] showed that the physicians' specialty had no effect on pain control and delay in analgesics prescription.
We found no significant relationship between patients' hospitalization shift and the mean of "delayed time between prescription and administration", but the afternoon shifts showed maximum delay and morning shifts the lowest time. It could be due to the fact that the nursing staff were working under the surveillance of the shift's supervisor in the morning shift, so the mean delay was lower, but in the afternoon shift the ward became crowded and nurses had to wait for the physicians' next orders until the night shift when they would visit the patients after attending clinics. In the night shift some patients were discharged and some were transferred to other wards and many of their escorts left the hospital; therefore, the ED would become less crowded and calm and the nursing staff could give better services. Consequently, the mean delay in night shift was less than the afternoons.
There was a significant relationship between the week-days and "delayed time between prescription and administration". The maximum delay was reported in Thursday and the minimum time was seen during Friday. The relationship between the type of prescribed drug and mean delay time were not statistically significant, but the maximum delay was seen in morphine and pethidine came in the second place and the minimum delay time was reported with diclofenac. The reason for rapid administration of diclofenac could be the fact that sometimes nurses gave patients this medication as suppository without physicians' order, and the cause of the increase in morphine delay time might be that in our ED this medication is usually used for substance abusers. Furthermore, the mean delay was greater in these individuals. Similarly, according to the study of Marinsek et al. [27] the most administered analgesic in the EDs were narcotics among which morphine was the most commonly used.
It should be mentioned that non-pharmacological methods to relieve pain including heating or cooling, elevation of body parts, and topical analgesics were only used in just 0.4% of our patients. However, in other emergency centers these modalities are more common for example in a center in Holland 40% of patients received some these alternative methods [11].
This study showed that the mean prescribed doses for pethidine and morphine were 30.93 mg and 3 mg, respectively. In our emergency center the dose of analgesic was not based on pain intensity (according to VAS) or patients' weight (except in children) and patients mostly received fixed and routine doses. Besides, due to everlasting shortage of narcotics in our hospitals, nurses have to dilute them and many patients even did not receive the meager dose prescribed by the physician; consequently, the effect of medications was practically less than expectation which could result in increased patients' dissatisfaction. Rupp and Delaney [28] reported that only 33% of their patients received sufficient and adequate doses of analgesics and just 60% of them were discharged without pain.
In our study, there was significant relationship between the physician seniority and the mean "delayed time between prescription and administration", while the maximum delay was related to the patients who were being supervised by the interns and the lowest delay was reported in those who were being supervised by the professors.
We found that only 52% of the physicians and 32.7% of nurses asked the patients about their pain intensity and in many cases VAS was not used to assess the pain intensity. This issue confirms the deficiency in trainings to assess the patient's pain intensity and emphasizes the need for supplementary courses for physicians and nurses about assessment and management of pain. Correspondingly, Eder et al. [25] mentioned in their study that only 19% of physicians and 30% of nurses asked the patients about their pain, while 94% of patients express their pain themselves and the assessment based on VAS was performed only in 23% of cases. On the other hand, Guru and Dubinsky [29] demonstrated that VAS and Numeric Rating Scale (NRS) were used to assess the pain intensity in 72% of patients; however, the pain intensities recorded by physicians and nurses were different from the scores that patients gave to their pain intensity. Usually the patient's scores were higher than the scores of physicians and nurses. In the study of Puntillo et al. [30] similar results were also reported.
Our final model of causes of delay demonstrated that patients from rural areas experienced more delays and further studies to uproot the incriminating factors are necessary. Orders by interns also resulted in more delay which might be due to their lack of authority over the nursing staff. Patients with female attending physicians, experienced less delay which could be a result of their vigilance to prove themselves as equals to their male colleagues.
According to our results, many patients suffered from oligoanalgesia and there was delay in their treatment. We suggest further studies on the treatment with analgesics based on medical guidelines in EDs in the shortest possible time and also to train physicians and nurses on pain assessment methods and analgesic prescription.
Go to : 
ACKNOWLEDGEMENTS
We would like to thank the staff members at Valiasr Hospital's ED for their untiring efforts and the Research Committee of Arak University of Medical Sciences for their support.
Go to : 
References
1. Fry M, Bennetts S, Huckson S. An Australian audit of ED pain management patterns. J Emerg Nurs. 2011; 37:269–274. PMID: 21550463.

2. Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department. Am J Emerg Med. 1989; 7:620–623. PMID: 2803357.

3. Ducharme J. Acute pain and pain control: state of the art. Ann Emerg Med. 2000; 35:592–603. PMID: 10828773.

4. Marshall KW. Practical implications of cyclooxygenase-2--specific inhibitors in orthopedics. Am J Orthop (Belle Mead NJ). 1999; 28(3 Suppl):19–21. PMID: 10193999.
5. Kelly AM. Patient satisfaction with pain management does not correlate with initial or discharge VAS pain score, verbal pain rating at discharge, or change in VAS score in the Emergency Department. J Emerg Med. 2000; 19:113–116. PMID: 10903456.

6. Yee AM, Puntillo K, Miaskowski C, Neighbor ML. What patients with abdominal pain expect about pain relief in the emergency department. J Emerg Nurs. 2006; 32:281–287. PMID: 16863872.

7. Zarei S, Bigizadeh S, Pourahmadi M, Ghobadifar MA. Chronic pain and its determinants: a population-based study in southern Iran. Korean J Pain. 2012; 25:245–253. PMID: 23091685.

8. Johnson SH. The social, professional, and legal framework for the problem of pain management in emergency medicine. J Law Med Ethics. 2005; 33:741–760. PMID: 16686244.

9. Tcherny-Lessenot S, Karwowski-Soulié F, Lamarche-Vadel A, Ginsburg C, Brunet F, Vidal-Trecan G. Management and relief of pain in an emergency department from the adult patients' perspective. J Pain Symptom Manage. 2003; 25:539–546. PMID: 12782434.

10. Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, et al. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007; 8:460–466. PMID: 17306626.

11. Berben SA, Meijs TH, van Dongen RT, van Vugt AB, Vloet LC, Mintjes-de Groot JJ, et al. Pain prevalence and pain relief in trauma patients in the Accident & Emergency department. Injury. 2008; 39:578–585. PMID: 17640644.

12. Jones JB. Assessment of pain management skills in emergency medicine residents: the role of a pain education program. J Emerg Med. 1999; 17:349–354. PMID: 10195504.

13. Hawkins SC, Smeeks F, Hamel J. Emergency management of chronic pain and drug-seeking behavior: an alternate perspective. J Emerg Med. 2008; 34:125–129. PMID: 17997073.

14. Arendts G, Fry M. Factors associated with delay to opiate analgesia in emergency departments. J Pain. 2006; 7:682–686. PMID: 16942954.

15. Wheeler E, Hardie T, Klemm P, Akanji I, Schonewolf E, Scott J, et al. Level of pain and waiting time in the emergency department. Pain Manag Nurs. 2010; 11:108–114. PMID: 20510841.

17. Lord B, Cui J, Kelly AM. The impact of patient sex on paramedic pain management in the prehospital setting. Am J Emerg Med. 2009; 27:525–529. PMID: 19497456.

18. Chen EH, Shofer FS, Dean AJ, Hollander JE, Baxt WG, Robey JL, et al. Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad Emerg Med. 2008; 15:414–418. PMID: 18439195.

19. Marquié L, Raufaste E, Lauque D, Mariné C, Ecoiffier M, Sorum P. Pain rating by patients and physicians: evidence of systematic pain miscalibration. Pain. 2003; 102:289–296. PMID: 12670671.

20. Weisse CS, Sorum PC, Dominguez RE. The influence of gender and race on physicians' pain management decisions. J Pain. 2003; 4:505–510. PMID: 14636818.

21. Ng B, Dimsdale JE, Rollnik JD, Shapiro H. The effect of ethnicity on prescriptions for patient-controlled analgesia for post-operative pain. Pain. 1996; 66:9–12. PMID: 8857626.

22. Iyer RG. Pain documentation and predictors of analgesic prescribing for elderly patients during emergency department visits. J Pain Symptom Manage. 2011; 41:367–373. PMID: 20965692.

23. Young MF, Hern HG, Alter HJ, Barger J, Vahidnia F. Racial differences in receiving morphine among prehospital patients with blunt trauma. J Emerg Med. 2013; 45:46–52. PMID: 23478179.

24. Kosiński S, Siudut B. Pain treatment in the emergency department: what do patients think? Anestezjol Intens Ter. 2011; 43:234–238. PMID: 22343441.
25. Eder SC, Sloan EP, Todd K. Documentation of ED patient pain by nurses and physicians. Am J Emerg Med. 2003; 21:253–257. PMID: 12898478.

26. Tanabe P, Thomas R, Paice J, Spiller M, Marcantonio R. The effect of standard care, ibuprofen, and music on pain relief and patient satisfaction in adults with musculoskeletal trauma. J Emerg Nurs. 2001; 27:124–131. PMID: 11275859.

27. Marinsek M, Kovacic D, Versnik D, Parasuh M, Golez S, Podbregar M. Analgesic treatment and predictors of satisfaction with analgesia in patients with acute undifferentiated abdominal pain. Eur J Pain. 2007; 11:773–778. PMID: 17251043.

28. Rupp T, Delaney KA. Inadequate analgesia in emergency medicine. Ann Emerg Med. 2004; 43:494–503. PMID: 15039693.

29. Guru V, Dubinsky I. The patient vs. caregiver perception of acute pain in the emergency department. J Emerg Med. 2000; 18:7–12. PMID: 10645828.

30. Puntillo K, Neighbor M, O'Neil N, Nixon R. Accuracy of emergency nurses in assessment of patients' pain. Pain Manag Nurs. 2003; 4:171–175. PMID: 14663795.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download