Abstract
Background
To improve residual pain management in acute cervical radiculopathy treated with NSAIDs, the feasibility of early and repeated low-dose interscalene brachial plexus block (IS-BPB) needs to be assessed.
Methods
This was a prospective study on patients receiving NSAIDs (loxoprofen) for cervical radiculopathy of ≤ 2-week onset. Pain was assessed using the visual analogue scale (VAS). A low-dose ultrasonography (USG)-guided IS-BPB (dexamethasone [1.65 mg; 0.5 ml] and mepivacaine [1%; 3.0 ml]) was performed at baseline and weekly thereafter for 4 weeks in an outpatient setting for the intervention group. All patients were evaluated using a visual satisfaction score (VSS) at week 4. Patients with baseline VAS scores < 70 (mild to moderate pain; MM group) and ≥ 70 (severe pain; SE group) were compared to the controls receiving NSAIDs.
Results
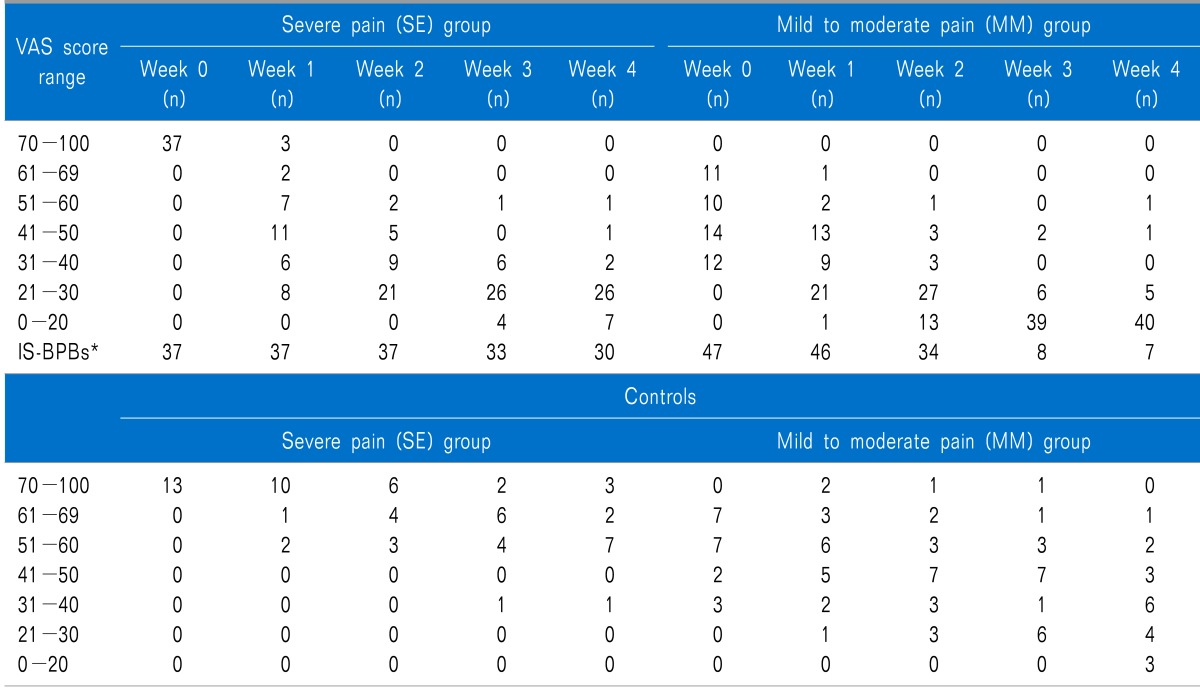
A total of 316 IS-BPBs were performed in the intervention group. There was a significant difference in the decline in the VAS from week 0 to week 3 in the MM and SE groups (P < 0.05); however, from week 3 to week 4, the therapeutic effect exhibited no significant difference. Thirteen patients at week 2 (15.5%; MM: 27.7%; SE: 0%), 43 at week 3 (51.2%; MM: 83.0%; SE: 10.8%), and 47 at week 4 (56.0%; MM: 85.1%; SE: 18.9%) achieved a VAS score of ≤ 20. Patient satisfaction was high, and the decrease in VAS scores in both groups was significant (P < 0.05) compared to the controls.
Go to : 
Cervical radiculopathy is marked by nerve compression due to disc herniation or arthritic bone spurs, and presents as neck pain and radiating arm pain or numbness accompanied by sensory deficits and motor dysfunction [1]. The pain is caused by a combination of factors that include inflammatory mediators (e.g., substance P), changes in vascular response, and intraneural oedema [2]. Cervical radiculopathy is one of the common types of peripheral neuropathic pain [3].
Interscalene brachial plexus block (IS-BPB) is used in surgery of the shoulder and is being considered as a possible option for treating cervical radiculopathy. It provides superior analgesia, uses a lower dose of anaesthetic, and is associated with fewer side effects and greater patient satisfaction. It is also easy to perform because the anatomical landmarks are readily identifiable [4]. Furthermore, in comparison with supraclavicular and axillary BPBs, the sensory block pattern of IS-BPB covers the largest area, including the upper dermatomes of the brachial plexus [5]. In addition, an ultrasonography (USG)-guided approach for IS-BPB has been shown to significantly improve the onset and completeness of sensory and motor block, reduce the incidence of paraesthesia, and confer greater safety [6]. The advantages of IS-BPB as a single low-dose nerve block during surgery can be effectively and safely translated into repeated nerve blocks for pain relief in cervical radiculopathy. Moreover, the drawbacks of IS-BPB encountered during surgery can be avoided in the outpatient setting. These include the onset time of anaesthesia; requirement of high doses, at which total motor paralysis and sensory loss may occur; and side effects associated with high doses, such as neurotoxicity, central nervous system symptoms, prolonged paralysis of sensory and motor nerves, symptoms of cardiovascular collapse, and phrenic nerve paralysis [7,8,9].
In this study, we evaluated the feasibility of early and repeated USG-guided IS-BPBs for residual pain in patients receiving nonsteroidal anti-inflammatory drugs (NSAIDS) for cervical radiculopathy in an outpatient setting. Low doses of dexamethasone (1.65 mg; 0.5 ml) and mepivacaine (1%; 3.0 ml) were used to selectively block the identified radicular pain pathway component (C5, or C6, or C7). We tried to highlight the relevance of targeting pain as a symptom and effectively treating it with repeated low-dose nerve blocks, while waiting for the cervical radiculopathy to resolve with other nonoperative measures or as a natural disease process.
Go to : 
This prospective study was carried out on consecutive commuting outpatients who had cervical radiculopathy of ≤ 2-week onset and were referred to our hospital between June 2010 and May 2012. All patients were initially treated with NSAIDs; after the first visit, they were converted to 1 tablet of loxoprofen (after each meal, 3 tablets/day), so that all patients received loxoprofen for a minimum of 3 days. They were then offered a choice of intervention (the USG-guided IS-BPB procedure) or continued treatment with NSAIDs. Based on their choice, the patients were grouped as either the intervention or control group. For both these groups, pain was assessed using the visual analogue scale (VAS, 100 mm) at baseline (week 0) and every week thereafter for 4 weeks. All patients were evaluated with a visual satisfaction score (VSS) at week 4. In the intervention group, time for recovery from motor paralysis of the treated arm was recorded for patients experiencing motor paralysis after IS-BPB. IS-BPB and NSAIDs were discontinued when the VAS score reached ≤ 20, and restarted if it increased to ≥ 20 within the 4-week treatment period. For patients in the intervention group with a VAS score of ≥ 20 at week 4, a final IS-BPB procedure was performed, and they were continued on loxoprofen. Patients were followed up for 6 months in the outpatient department or telephonically. Patients with persistent pain after 4 weeks of IS-BPB were treated with one of the following procedures: a nerve root block, intradiscal steroid injection, selective transforaminal epidural block, cervical epidural block, or tramadol/acetaminophen combination tablets.
Patients in the intervention group were further evaluated by dividing them into 2 groups based on the baseline VAS score: (1) VAS score < 70 (mild to moderate pain; MM group) and (2) VAS score ≥ 70 (severe pain; SE group). They were later compared to the controls treated with NSAIDS only (patients who refused interventional treatment). The study was approved by the ethics committee of the Nara Perfectural Mimuro Hospital, and written informed consent was obtained from all patients enrolled in the study. The study was conducted in accordance with the Good Clinical Practices (GCP) guidelines and the Declaration of Helsinki.
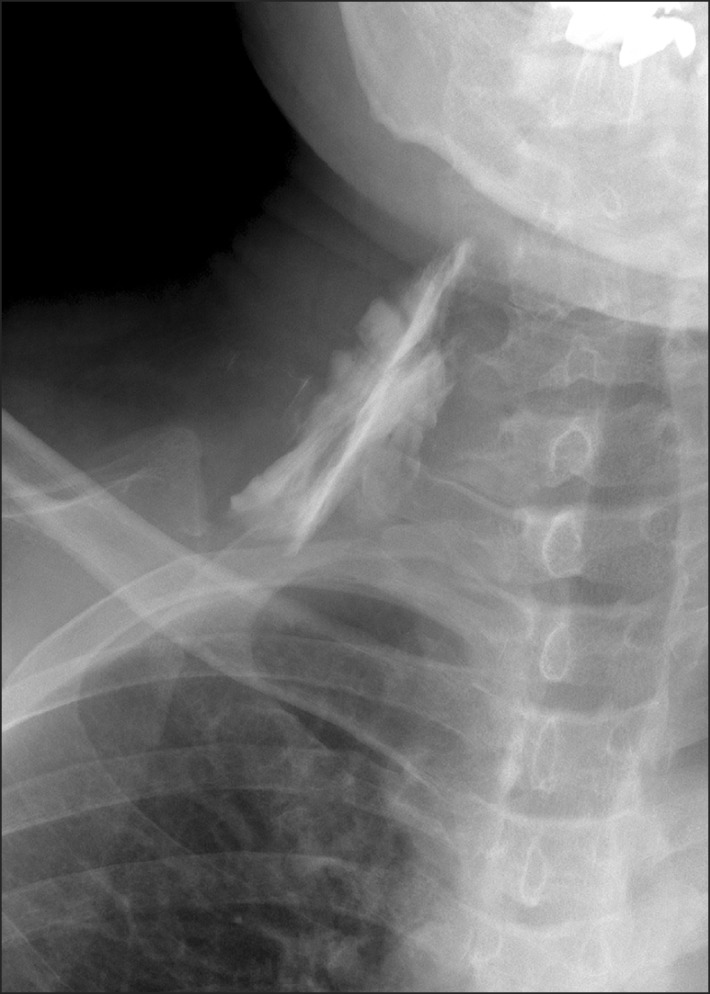
Patients with cervical radiculopathy originating from a single root within 2 weeks of onset, who did not develop cervical myelopathy or upper limb muscular weakness or spine instability, were enrolled. The patients were diagnosed with the presence of osteophytes in the intervertebral foramen (confirmed by cervical radiograph plain X-P or computed tomography [CT]) or disc herniation (confirmed by cervical magnetic resonance imaging [MRI]). Subjective symptoms, loss of sensation, and neurological findings were assessed with the Jackson's test and Spurling's test and by sensory and motor evaluation of the involved nerve root. Subjects with confirmed injection of the total dose in the interscalene groove were considered for evaluation. Patients with coagulation abnormalities, ongoing antithrombotic therapy, diabetes, digestive ulcers, kidney disease, or lung disease were excluded from the study. Patients who showed no interscalene spread of the drug with USG at any time point within the 4 weeks were excluded from the study. Nonoperative measures such as the use of cervical collar and traction were allowed if necessary.
IS-BPB was performed under ultrasound guidance for all individuals in the intervention group as a part of the protocol. Low-dose dexamethasone (1.65 mg; 0.5 ml) and mepivacaine (1%; 3.0 ml), for a total volume of 3.5 ml, was injected using a 22 G × 50 mm (B/BRAUN, Tokyo, Japan) needle; the needle puncture was parallel to the ultrasound probe. Care was taken that the needle did not go beyond the middle scalene muscle fascia, as observed from the drug injection image. This was confirmed by USG while the first 1 ml was being injected. Thereafter, the remaining amount (2.5 ml) was injected. The drug was administered primarily between the upper and middle neural stems. The USG-guided IS-BPB procedure with contrast imaging showing the area and pattern of contrast distribution performed in a volunteer (not included in this study) is shown in Fig. 1. After drug injection, the patients were placed on bed rest, and their blood pressure and oxygen saturation (SPO2) levels were monitored for at least 1 hour. Patients experiencing partial motor nerve paralysis were allowed to return home after complete recovery of the treated arm.
The primary endpoint was to evaluate the feasibility and efficacy of early and repeated USG-guided IS-BPB in an outpatient setting, for residual pain in patients with acute cervical radiculopathy. The secondary endpoints included assessing whether low-dose IS-BPB could be a suitable choice for an intervention treatment, could reduce adverse events and increase safety, and also reduce the need for conventional doses of anaesthetic agents.
After every IS-BPB procedure, the patient's blood pressure and SPO2 were monitored for 1 hour. Adverse events were also monitored, and the patient was allowed to return home after complete recovery from motor nerve paralysis of the treated arm. Patients were advised to report any adverse events that occurred during the entire study duration.
Changes in VAS scores at each of the observation points were compared with one-way repeated measures analysis of variance (ANOVA), in terms of the afflicted nerve and severity. Patient baseline characteristics in terms of severity and treatment outcome during the study duration were analysed using an unpaired t-test and the chi-squared test, with the level of significance set at P < 0.05. Average values are expressed as the mean ± SD.
Go to : 
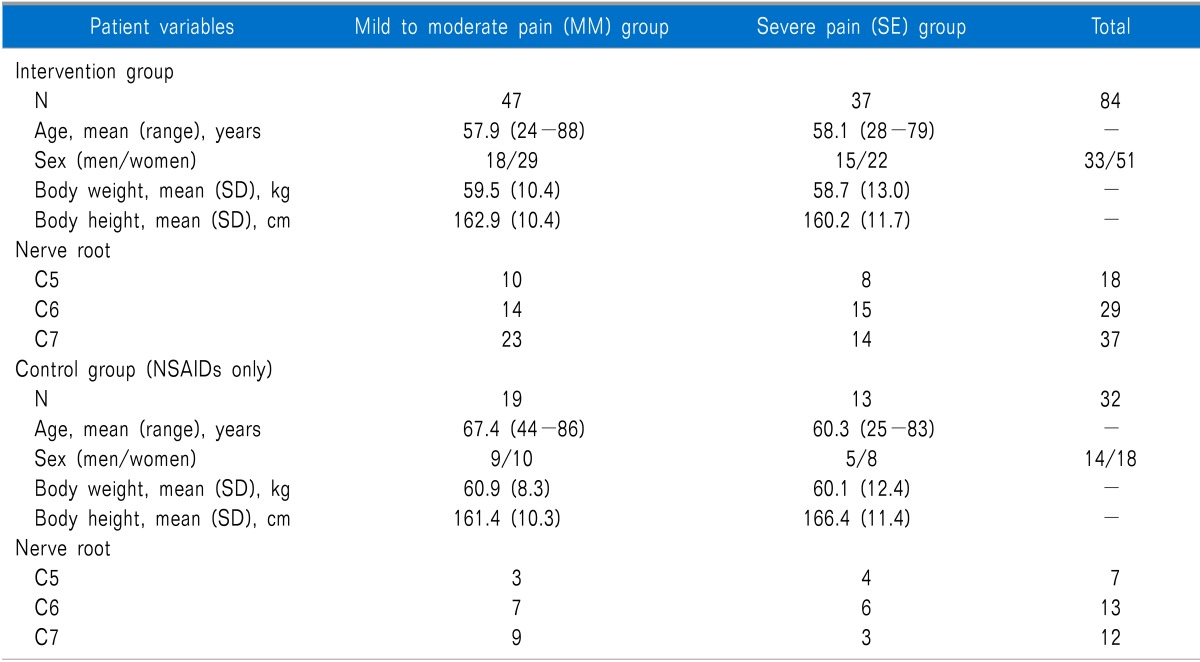
A total of 88 patients were enrolled in the intervention group and 32 in the control group. Four patients were excluded from the intervention group because they did not show a USG-detected interscalene spread of the drug. Thus, 84 (95.5%; 33 men, 51 women) patients from the intervention group were evaluated. Table 1 shows the baseline characteristics of the intervention and control group patients divided into the MM and SE categories (Table 1).
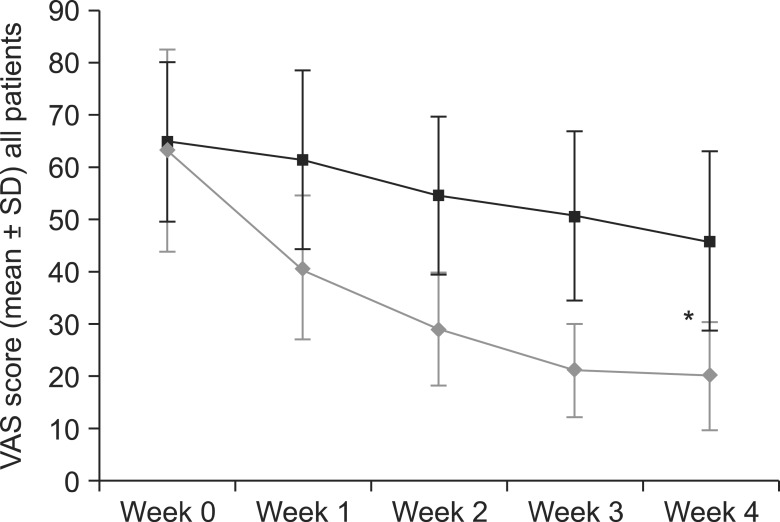
The VAS score (mean ± SD) showed a significant decline from week 0 (63.3 ± 19.4) to week 4 (20.0 ± 10.3). All patients experienced pain relief as early as week 1 (VAS score, 40.9 ± 13.9), and further improvement was seen at week 2 (29.0 ± 10.8) (Fig. 2). There was no significant difference in the therapeutic effect based on the VAS score, among patients with C5, C6, and C7 nerve root involvement.
Among patients reporting pain at the end of week 4, 10 were treated with a nerve root block, 10 with a cervical epidural block, 3 with both a nerve root block and intradiscal steroid injection under fluoroscopy, and 2 with both a nerve root block and tramadol/acetaminophen combination tablets. The longest treatment course lasted 19 weeks for 1 patient who underwent 2 nerve root block procedures along with tramadol/acetaminophen combination tablets. Only 1 patient underwent a laminectomy at week 9.
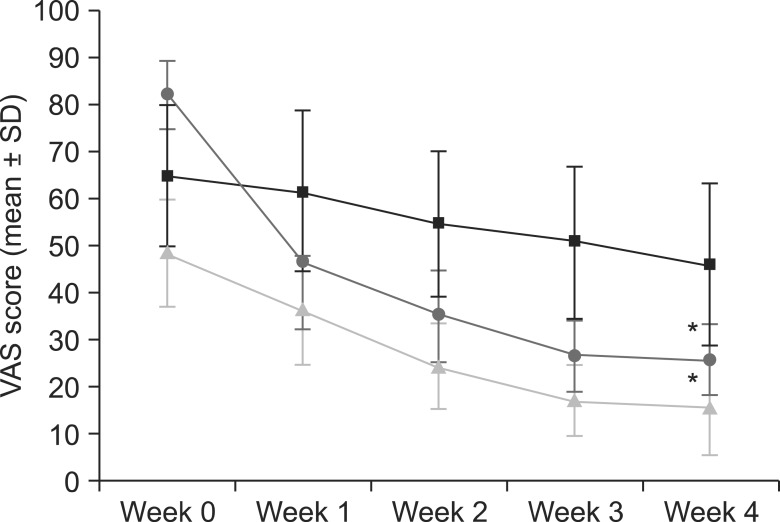
There was a significant difference in the decline in VAS score from week 0 to week 3 in the MM and SE groups (P < 0.05); however, from week 3 to week 4, the therapeutic effect exhibited no significant difference. The VAS values between the MM and SE groups at weeks 1, 2, 3, and 4 were significantly different (P < 0.05), with patients in the SE group less likely to experience alleviation of symptoms until week 4 (Fig. 3). Patients in the MM group showed an early treatment response in comparison to the SE group (Fig. 3). The treatment was concluded as early as week 2 (requiring 2 IS-BPBs) for 13 patients because they achieved a VAS score of ≤ 20 (15.5%; MM group: 27.7%; SE group: 0%). A total of 43 patients (51.2%; MM group: 83.0%; SE group: 10.8%) at week 3 (requiring 3 IS-BPBs) and 47 patients (56%; MM group: 85.1%; SE group: 18.9%) at week 4 (requiring 4 IS-BPBs) achieved a VAS score of ≤ 20. The rate of study treatment completion was significantly higher in the MM group than in the SE group at weeks 2, 3, and 4 (P < 0.05) (Table 2). At week 2, 86.9% of all patients (MM group: 91.5%; SE group: 81.1%) had achieved a VAS score of ≤ 40, while 89.3% (MM group: 95.7%; SE group: 81.1%) had a VAS score of ≤ 30 at week 3.
When compared to the controls treated with NSAIDS alone, there was a significant reduction in the VAS scores in the MM and SE groups over the 4 weeks (P < 0.05; Mann-Whitney U test).
There was no significant difference in the VSS of patients in the MM and SE groups (Mann-Whitney U test) in the intervention group. At week 4, a majority of patients reported a VSS of ≥ 80, and 2 patients (1 each in the MM and SE groups) with a VAS score of 55 reported a VSS of 53 and 35, respectively. Additionally, 1 patient in the SE group with a VAS score of 44 reported a VSS of 78 at week 4.
In the control group, only 5 patients (26.3%) in the MM group and no patients (0%) in the SE group reported a VSS of ≥ 80.
A total of 84 episodes of partial motor nerve blocks lasting 84.7 ± 40.9 minutes (range, 25-190 minutes) were noted, from a total of 316 IS-BPBs performed. No reports of Horner's symptoms, recurrent laryngeal nerve paralysis, haemodynamic changes, respiratory discomfort, and symptoms of IS-BPB-induced neuropathy were noted in this study.
Go to : 
This study evaluated the feasibility of using repeated, low-dose, USG-guided IS-BPB in an outpatient setting for residual pain in patients with acute cervical radiculopathy treated with NSAIDS. Our study showed that patients on NSAIDS experienced significant pain that could be easily targeted with weekly USG-guided IS-BPB, a safe and feasible procedure. This adds to recent research on effective and target-specific measures to treat pain [10,11], helping clinicians to manage pain more effectively.
Although cervical radiculopathy is treated conservatively [3,12,13] and symptoms resolve in 3 to 6 months [14,15], one third of patients continue to have persistent symptoms [1,16]. Theoretically, NSAIDs provide an analgesic effect and reduce inflammation around the nerve route, thereby decreasing its sensitivity to compression; however, there is no evidence that NSAIDs are more effective than pure analgesics such as acetaminophen [3]. Patients managed conservatively, who do not find relief from pain and suffer from the side effects of long-term NSAID administration, are often referred to the outpatient pain control unit at our hospital. We believe that these patients with residual pain are ideal candidates for this repeated USG-guided IS-BPB procedure, which can be performed in an outpatient setting.
Treatment with pain medications and nerve block therapy are often practiced in parallel, and several blocks such as BPB, nerve root block, cervical epidural block, and stellate ganglion block are considered [17,18,19,20]. A nerve root block, which is the closest to the dorsal root ganglia (DRG) that receives compression, is considered to be most effective [19]. However, it requires a fluoroscopic device and often cannot be performed immediately after diagnosis, making it a difficult choice for implementation in an outpatient setting. A nerve root block can also be performed under USG guidance, but when the needle is advanced up to the nerve root level (unlike when performed with a contrast agent under fluoroscopy), anatomically, there may be more complications than with BPB, such as blood vessel puncture and subarachnoid injection. Various reviews and studies have discussed the advantages and disadvantages of the different types of BPBs in relation to the equipment required, dose administered, and the technique used [5,17,19,20,21,22]. Therefore, a small-dose BPB under USG guidance that can mimic the efficacy of a nerve root block could potentially resolve the problems of equipment needs and complications.
The efficacy of any interscalene approach for cervical radiculopathy can be enhanced by USG in terms of the accuracy, lack of side effects [5,23], and lower dose required. Although it can help avoid direct contact with the nerves and larger blood vessels [24], it is often difficult to avoid small blood vessels that cannot be visualized by USG. This unintentional inclusion of small vessels further increases the desirability for a smaller dosage and volume. In the present study, USG was able to cover the C5-C7 nerve roots by administering the drug between the stems of 2 nerve roots, thereby affecting the main nerve trunk.
Conventionally, higher quantities of anaesthetics and steroids are used for IS-BPB and other BPBs in an outpatient setting [18], which may cause motor nerve paralysis leading to enhanced patient anxiety and safety concerns for travel. In addition, injecting large volumes of these drugs may lead to accidental intravascular injection. The lower absolute quantities of anaesthetics and steroids used in this study reduced the possibility of local anaesthetic intoxication, phrenic nerve paralysis, and neurotoxicity [7,22,23]. Phrenic nerve paralysis has been reported to occur 45% of the time with a 5 ml injection volume [22]; therefore, careful attention is required even when a 3.5 ml volume is injected. However, in the present study, no such side effects were observed.
In terms of severity, the SE group exhibited a tendency for delayed pain relief. This suggests that for patients with severe pain, a block under fluoroscopy, such as a nerve root block, or the use of weak opioids should be considered at an early stage. Opioids are indicated in selected patients with moderate to severe pain that is refractory to nonopioid agents and nonpharmacological therapies [3]. Early treatment is important because prolonged symptoms lead to a complex intertwining of not only the elements of nociceptive and neuropathic pain, but also of sympathetically maintained pain [25] and psychogenic and societal [26] factors, which support the transition to chronic pain. The patients in this study presented with acute pain, which may have contributed to the high efficacy of IS-BPB in the MM group.
It could be inferred from the contrast distribution that the drug could reach close to the nerve root. However, it is unknown whether the drug actually reached all the nerve roots (C5, C6, or C7) in all the patients. It is also possible that if the needle gets to the peripheral site of the nerve root, the drug may not spread centrally; thus, the drug acts like a peripheral nerve block. The patients in this study experienced immediate pain relief with IS-BPB. Temporary blocking of peripheral nociceptive input using IS-BPB can normalize the central processing of pain, thereby eliminating allodynia and other associated abnormalities such as spontaneous pain [27].
The limitations of this study include a comparison with historical controls treated with NSAIDS. Furthermore, because this study involved patients with acute cervical radiculopathy, alleviation of pain due to the natural passage of time could not be assessed. However, when targeting pain as a symptom, the IS-BPB procedure performed after evaluating the VAS (≥ 20) was able to provide immediate pain relief in an outpatient setting. Further studies will be required to evaluate the efficacy of IS-BPB in chronic cervical radiculopathy.
Go to : 
This study highlights the possibility of using weekly USG-guided IS-BPB for early pain relief in acute cervical radiculopathy, instead of keeping it as a last resort rescue procedure for chronic pain. This approach, using a small dose, could safely provide clinically satisfactory pain relief in an outpatient setting, especially in patients with mild or moderate pain, with high patient satisfaction. Because these patients were treated with NSAIDS, the high level of residual pain identified by VAS justified the implementation of IS-BPB. Available literature suggests that a multimodal approach may benefit patients with cervical radiculopathy [1]. This low-dose, USG-guided IS-BPB procedure performed in an outpatient setting could become part of a multimodal approach.
Go to : 
References
1. Eubanks JD. Cervical radiculopathy: nonoperative management of neck pain and radicular symptoms. Am Fam Physician. 2010; 81:33–40. PMID: 20052961.
2. Levine MJ, Albert TJ, Smith MD. Cervical radiculopathy: diagnosis and nonoperative management. J Am Acad Orthop Surg. 1996; 4:305–316. PMID: 10797198.

3. Dworkin RH, Backonja M, Rowbotham MC, Allen RR, Argoff CR, Bennett GJ, et al. Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol. 2003; 60:1524–1534. PMID: 14623723.
4. Long TR, Wass CT, Burkle CM. Perioperative interscalene blockade: an overview of its history and current clinical use. J Clin Anesth. 2002; 14:546–556. PMID: 12477594.

5. Neal JM, Hebl JR, Gerancher JC, Hogan QH. Brachial plexus anesthesia: essentials of our current understanding. Reg Anesth Pain Med. 2002; 27:402–428. PMID: 12132064.

6. Soeding PE, Sha S, Royse CE, Marks P, Hoy G, Royse AG. A randomized trial of ultrasound-guided brachial plexus anaesthesia in upper limb surgery. Anaesth Intensive Care. 2005; 33:719–725. PMID: 16398375.

7. Dhir S, Ganapathy S, Lindsay P, Athwal GS. Case report: ropivacaine neurotoxicity at clinical doses in interscalene brachial plexus block. Can J Anaesth. 2007; 54:912–916. PMID: 17975237.

8. Krone SC, Chan VW, Regan J, Peng P, Poate EM, McCartney C, et al. Analgesic effects of low-dose ropivacaine for interscalene brachial plexus block for outpatient shoulder surgery-a dose-finding study. Reg Anesth Pain Med. 2001; 26:439–443. PMID: 11561264.

9. Fujimura N, Namba H, Tsunoda K, Kawamata T, Taki K, Igarasi M, et al. Effect of hemidiaphragmatic paresis caused by interscalene brachial plexus block on breathing pattern, chest wall mechanics, and arterial blood gases. Anesth Analg. 1995; 81:962–966. PMID: 7486085.

10. Kang SS, Jung JW, Song CK, Yoon YJ, Shin KM. A new anterior approach for fluoroscopy-guided suprascapular nerve block - a preliminary report -. Korean J Pain. 2012; 25:168–172. PMID: 22787547.

11. Choi IG, Choi YS, Kim YH, Min JH, Chae YK, Lee YK, et al. The effects of postoperative brachial plexus block using MgSO(4) on the postoperative pain after upper extremity surgery. Korean J Pain. 2011; 24:158–163. PMID: 21935495.

12. Boyce RH, Wang JC. Evaluation of neck pain, radiculopathy, and myelopathy: imaging, conservative treatment, and surgical indications. Instr Course Lect. 2003; 52:489–495. PMID: 12690875.
13. Swezey RL, Swezey AM, Warner K. Efficacy of home cervical traction therapy. Am J Phys Med Rehabil. 1999; 78:30–32. PMID: 9923426.
14. Persson LC, Moritz U, Brandt L, Carlsson CA. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar. A prospective, controlled study. Eur Spine J. 1997; 6:256–266. PMID: 9294750.

15. Heckmann JG, Lang CJ, Zöbelein I, Laumer R, Druschky A, Neundörfer B. Herniated cervical intervertebral discs with radiculopathy: an outcome study of conservatively or surgically treated patients. J Spinal Disord. 1999; 12:396–401. PMID: 10549703.
16. Lees F, Turner JW. Natural history and prognosis of cervical spondylosis. Br Med J. 1963; 2:1607–1610. PMID: 14066179.

17. Candido KD, Knezevic N. Cervical epidural steroid injections for the treatment of cervical spinal (neck) pain. Curr Pain Headache Rep. 2013; 17:314. PMID: 23315021.

18. Murata Y, Kanaya K, Wada H, Wada K, Shiba M, Hatta S, et al. Interscalene brachial plexus block for scapular and upper chest pain due to cervical radiculopathy: a randomized controlled clinical trial. J Orthop Sci. 2012; 17:515–520. PMID: 22828914.

19. Chung JY, Yim JH, Seo HY, Kim SK, Cho KJ. The efficacy and persistence of selective nerve root block under fluoroscopic guidance for cervical radiculopathy. Asian Spine J. 2012; 6:227–232. PMID: 23275805.

20. Bruce BG, Green A, Blaine TA, Wesner LV. Brachial plexus blocks for upper extremity orthopaedic surgery. J Am Acad Orthop Surg. 2012; 20:38–47. PMID: 22207517.

21. Yuan JM, Yang XH, Fu SK, Yuan CQ, Chen K, Li JY, et al. Ultrasound guidance for brachial plexus block decreases the incidence of complete hemi-diaphragmatic paresis or vascular punctures and improves success rate of brachial plexus nerve block compared with peripheral nerve stimulator in adults. Chin Med J (Engl). 2012; 125:1811–1816. PMID: 22800905.
22. Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008; 101:549–556. PMID: 18682410.

23. Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2009; 34:498–502. PMID: 19920426.

24. Loubert C, Williams SR, Hélie F, Arcand G. Complication during ultrasound-guided regional block: accidental intravascular injection of local anesthetic. Anesthesiology. 2008; 108:759–760. PMID: 18362609.

25. Chabal C, Jacobson L, Russell LC, Burchiel KJ. Pain response to perineuromal injection of normal saline, epinephrine, and lidocaine in humans. Pain. 1992; 49:9–12. PMID: 1594285.

26. Murphy DR, Hurwitz EL, Gregory A, Clary R. A nonsurgical approach to the management of patients with cervical radiculopathy: a prospective observational cohort study. J Manipulative Physiol Ther. 2006; 29:279–287. PMID: 16690382.

27. Gracely RH, Lynch SA, Bennett GJ. Painful neuropathy: altered central processing maintained dynamically by peripheral input. Pain. 1992; 51:175–194. PMID: 1484715.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download