1. Gregori-Puigjané E, Setola V, Hert J, Crews BA, Irwin JJ, Lounkine E, et al. Identifying mechanism-of-action targets for drugs and probes. Proc Natl Acad Sci U S A. 2012; 109:11178–11183. PMID:
22711801.

2. Moore RA, Derry S, McQuay HJ, Wiffen PJ. Single dose oral analgesics for acute postoperative pain in adults. Cochrane Database Syst Rev. 2011; (9):CD008659. PMID:
21901726.

3. Alfonsi P, Adam F, Passard A, Guignard B, Sessler DI, Chauvin M. Nefopam, a nonsedative benzoxazocine analgesic, selectively reduces the shivering threshold in unanesthetized subjects. Anesthesiology. 2004; 100:37–43. PMID:
14695722.

4. Heel RC, Brogden RN, Pakes GE, Speight TM, Avery GS. Nefopam: a review of its pharmacological properties and therapeutic efficacy. Drugs. 1980; 19:249–267. PMID:
6991238.
5. Podranski T, Bouillon TW, Riva T, Kurz AM, Oehmke MJ. Compartmental pharmacokinetics of nefopam during mild hypothermia. Br J Anaesth. 2012; 108:784–791. PMID:
22331396.

6. Bassett JR, Cairncross KD, Hacket NB, Story M. Studies on the peripheral pharmacology of fenazoxine, a potential antidepressant drug. Br J Pharmacol. 1969; 37:69–78. PMID:
5343358.

7. Tobin WE, Gold RH. Nefopam hydrochloride: a novel muscle relaxant. J Clin Pharmacol New Drugs. 1972; 12:230–238. PMID:
4555883.

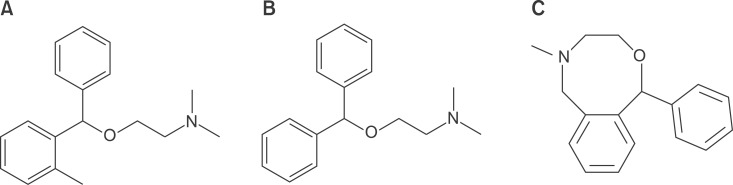
8. Bolt AG, Graham G, Wilson P. Stereoselective demethylation of the enantiomers of nefopam, an experimental antidepressant and skeletal muscle relaxant. Xenobiotica. 1974; 4:355–363. PMID:
4842015.

9. Koe BK. Molecular geometry of inhibitors of the uptake of catecholamines and serotonin in synaptosomal preparations of rat brain. J Pharmacol Exp Ther. 1976; 199:649–661. PMID:
994022.
10. Cohen A. Nefopam hydrochloride for pain relief. Curr Ther Res Clin Exp. 1974; 16:184–193. PMID:
4206725.
11. Klotz AL. Long-term safety of Nefopam hydrochloride (Acupan), a new analgesic formulation. Curr Ther Res Clin Exp. 1974; 16:602–608. PMID:
4211140.
12. Workmon FC, Winter L Jr. A clinical evaluation of nefopam hydrochloride (Acupan): a new analgesic. Curr Ther Res Clin Exp. 1974; 16:609–616. PMID:
4211141.
13. Kolodny AL, Winter L Jr. Further clinical evaluations of nefopam hydrochloride, a new analgesic. Curr Ther Res Clin Exp. 1975; 17:519–524. PMID:
808373.
14. Kakkar M, Derry S, Moore RA, McQuay HJ. Single dose oral nefopam for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009; (3):CD007442. PMID:
19588431.

15. Izzo V, Mariconti P, Tiengo M. Action and effectiveness of nefopam chloride in the control of postoperative shivering. Minerva Anestesiol. 1991; 57:760–762. PMID:
1798568.
16. Kim YA, Kweon TD, Kim M, Lee HI, Lee YJ, Lee KY. Comparison of meperidine and nefopam for prevention of shivering during spinal anesthesia. Korean J Anesthesiol. 2013; 64:229–233. PMID:
23560188.

17. Park SM, Mangat HS, Berger K, Rosengart AJ. Efficacy spectrum of antishivering medications: meta-analysis of randomized controlled trials. Crit Care Med. 2012; 40:3070–3082. PMID:
22890247.
18. Bilotta F, Rosa G. Nefopam for severe hiccups. N Engl J Med. 2000; 343:1973–1974. PMID:
11186682.

19. Bilotta F, Pietropaoli P, Rosa G. Nefopam for refractory postoperative hiccups. Anesth Analg. 2001; 93:1358–1360. PMID:
11682430.

20. Pajot S, Geeraerts T, Leblanc PE, Duranteau J, Benhamou D. Hiccup during weaning from mechanical ventilation: the use of nefopam. Br J Anaesth. 2007; 99:748–749. PMID:
17933805.

21. Barrot M. Tests and models of nociception and pain in rodents. Neuroscience. 2012; 211:39–50. PMID:
22244975.

22. Jaggi AS, Jain V, Singh N. Animal models of neuropathic pain. Fundam Clin Pharmacol. 2011; 25:1–28. PMID:
20030738.

23. Hunskaar S, Hole K. The formalin test in mice: dissociation between inflammatory and non-inflammatory pain. Pain. 1987; 30:103–114. PMID:
3614974.

24. Cho SY, Park AR, Yoon MH, Lee HG, Kim WM, Choi JI. Antinociceptive effect of intrathecal nefopam and interaction with morphine in formalin-induced pain of rats. Korean J Pain. 2013; 26:14–20. PMID:
23342202.

25. Girard P, Pansart Y, Coppe MC, Gillardin JM. Nefopam reduces thermal hypersensitivity in acute and postoperative pain models in the rat. Pharmacol Res. 2001; 44:541–545. PMID:
11735363.

26. Buritova J, Besson JM. Effects of nefopam on the spinal nociceptive processes: a c-Fos protein study in the rat. Eur J Pharmacol. 2002; 441:67–74. PMID:
12007921.

27. Laboureyras E, Chateauraynaud J, Richebé P, Simonnet G. Long-term pain vulnerability after surgery in rats: prevention by nefopam, an analgesic with antihyperalgesic properties. Anesth Analg. 2009; 109:623–631. PMID:
19608840.

28. Evans MS, Lysakowski C, Tramèr MR. Nefopam for the prevention of postoperative pain: quantitative systematic review. Br J Anaesth. 2008; 101:610–617. PMID:
18796441.

29. Tigerstedt I, Tammisto T, Leander P. Comparison of the analgesic dose-effect relationships of nefopam and oxycodone in postoperative pain. Acta Anaesthesiol Scand. 1979; 23:555–560. PMID:
397711.

30. Dordoni PL, Della Ventura M, Stefanelli A, Iannace E, Paparella P, Rocca B, et al. Effect of ketorolac, ketoprofen and nefopam on platelet function. Anaesthesia. 1994; 49:1046–1049. PMID:
7864317.

31. Gasser JC, Bellville JW. Respiratory effects of nefopam. Clin Pharmacol Ther. 1975; 18:175–179. PMID:
1097153.

32. Guindon J, Walczak JS, Beaulieu P. Recent advances in the pharmacological management of pain. Drugs. 2007; 67:2121–2133. PMID:
17927280.

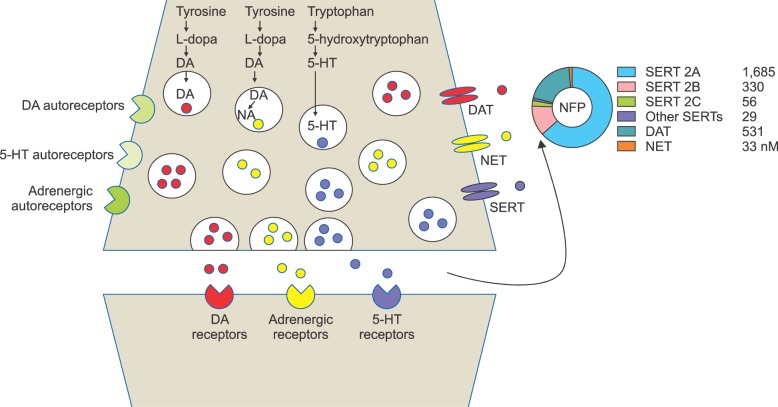
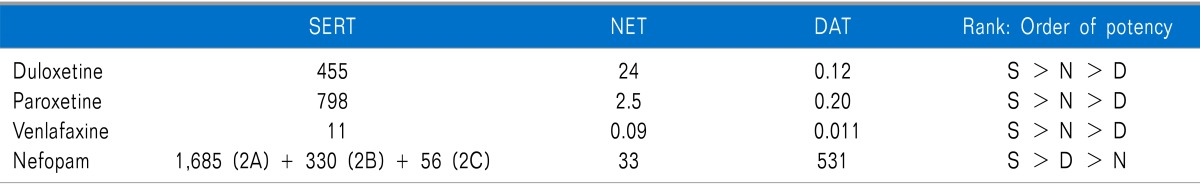
33. Torres GE, Gainetdinov RR, Caron MG. Plasma membrane monoamine transporters: structure, regulation and function. Nat Rev Neurosci. 2003; 4:13–25. PMID:
12511858.

34. Max MB, Gilron IH. Antidepressants, muscle relaxants, and N-methyl-D-aspartate receptor antagonists. In : Loeser JD, Bonica JJ, editors. Bonica's management of pain. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins;2001. p. 1710–1726.
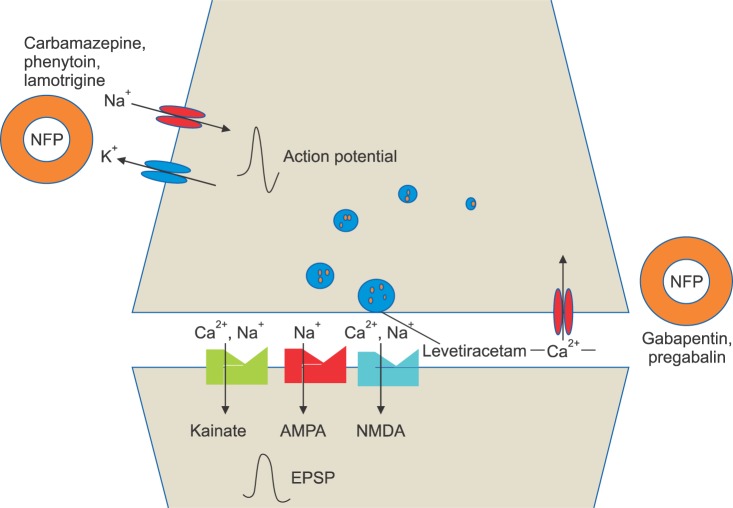
35. Novelli A, Díaz-Trelles R, Groppetti A, Fernández-Sánchez MT. Nefopam inhibits calcium influx, cGMP formation, and NMDA receptor-dependent neurotoxicity following activation of voltage sensitive calcium channels. Amino Acids. 2005; 28:183–191. PMID:
15714253.

36. Verleye M, André N, Heulard I, Gillardin JM. Nefopam blocks voltage-sensitive sodium channels and modulates glutamatergic transmission in rodents. Brain Res. 2004; 1013:249–255. PMID:
15193535.

37. Biella GE, Groppetti A, Novelli A, Fernández-Sánchez MT, Manfredi B, Sotgiu ML. Neuronal sensitization and its behavioral correlates in a rat model of neuropathy are prevented by a cyclic analog of orphenadrine. J Neurotrauma. 2003; 20:593–601. PMID:
12906743.

38. Novelli A, Groppetti A, Rossoni G, Manfredi B, Ferrero-Gutiérrez A, Pérez-Gómez A, et al. Nefopam is more potent than carbamazepine for neuroprotection against veratridine in vitro and has anticonvulsant properties against both electrical and chemical stimulation. Amino Acids. 2007; 32:323–332. PMID:
17021653.

39. Czuczwar M, Czuczwar K, Cięszczyk J, Kiś J, Saran T, Łuszczki JJ, et al. Nefopam enhances the protective activity of antiepileptics against maximal electroshock-induced convulsions in mice. Pharmacol Rep. 2011; 63:690–696. PMID:
21857079.

40. Löscher W, Schmidt D. New Horizons in the development of antiepileptic drugs: innovative strategies. Epilepsy Res. 2006; 69:183–272. PMID:
16835945.

41. Hoebel BG, Hernandez L, Schwartz DH, Mark GP, Hunter GA. Microdialysis studies of brain norepinephrine, serotonin, and dopamine release during ingestive behavior. Theoretical and clinical implications. Ann N Y Acad Sci. 1989; 575:171–191. PMID:
2699187.

42. Hoyer D, Clarke DE, Fozard JR, Hartig PR, Martin GR, Mylecharane EJ, et al. International Union of Pharmacology classification of receptors for 5-hydroxytryptamine (Serotonin). Pharmacol Rev. 1994; 46:157–203. PMID:
7938165.
43. Fink KB, Göthert M. 5-HT receptor regulation of neurotransmitter release. Pharmacol Rev. 2007; 59:360–417. PMID:
18160701.

44. Barnes NM, Sharp T. A review of central 5-HT receptors and their function. Neuropharmacology. 1999; 38:1083–1152. PMID:
10462127.

45. Bannister K, Bee LA, Dickenson AH. Preclinical and early clinical investigations related to monoaminergic pain modulation. Neurotherapeutics. 2009; 6:703–712. PMID:
19789074.

46. Cotecchia S, Stanasila L, Diviani D. Protein-protein interactions at the adrenergic receptors. Curr Drug Targets. 2012; 13:15–27. PMID:
21777184.

47. Girault JA, Greengard P. The neurobiology of dopamine signaling. Arch Neurol. 2004; 61:641–644. PMID:
15148138.

48. Benzon HT. The neuropathic pain scales. Reg Anesth Pain Med. 2005; 30:417–421. PMID:
16135344.

49. Mather GG, Labroo R, Le Guern ME, Lepage F, Gillardin JM, Levy RH. Nefopam enantiomers: preclinical pharmacology/toxicology and pharmacokinetic characteristics in healthy subjects after intravenous administration. Chirality. 2000; 12:153–159. PMID:
10689295.

50. Durrieu G, Olivier P, Bagheri H, Montastruc JL. French Network of Pharmacovigilance Centers. Overview of adverse reactions to nefopam: an analysis of the French Pharmacovigilance database. Fundam Clin Pharmacol. 2007; 21:555–558. PMID:
17868209.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download