Abstract
Compensatory hyperhidrosis or reflex hyperhidrosis is the increase in sweating in the postoperative stage of thoracic sympathectomy or lumbar sympathectomy. It shares several features with anxiety disorders and has a negative impact on a patient's quality of life. Oralglycopyrrolate is one of the treatment options available. This study reviewed case notes in a series of 19 patients with compensatory hyperhidrosis. We made a comparison between the Milanez de Campos score of a pre-glycopyrrolate medication group and the Milanez de Campos score of a post-glycopyrrolate medication group. The Beck Depression Inventory (BDI) score, Beck Anxiety Inventory (BAI) score, and autonomic nervous system (ANS) scale score were also compared between the pre-medication and post-medication groups. In the post-glycopyrrolate medication group, there was decrease in the Milanez de Campos score, BAI score, and BDI score (P < 0.05). But no meaningful change was seen in the ANS score in the post-glycopyrrolate medication group (P > 0.05). Glycopyrrolate is an effective medication in the treatment of compensatory hyperhidrosis that, can alleviate anxiety and improve patients' quality of life.
Go to : 
Compensatory hyperhidrosis is the phenomenon of increased compensatory sweating in parts of the body unrelated to surgery or anatomy after sympathectomy [1]. Among the various methods for treating compensatory hyperhidrosis, the preferred treatment should be less invasive, have minimal side effects, and be less of an economic burden. In this respect,drug treatment will be the primarily utilized treatment method. Glycopyrrolate is different fromother anticholinergic agents in that it does not pass through the blood-brain barrier; it is thus the most widely used drug, as it has relatively few side effects compared with other medications. This study administered glycopyrrolate, which can be applied without particular restrictions, to patients with compensatory hyperhidrosis. Patients' case notes were examined before and after administration of the drug to determine the degree of improvement in compensatory hyperhidrosis and psychological state.
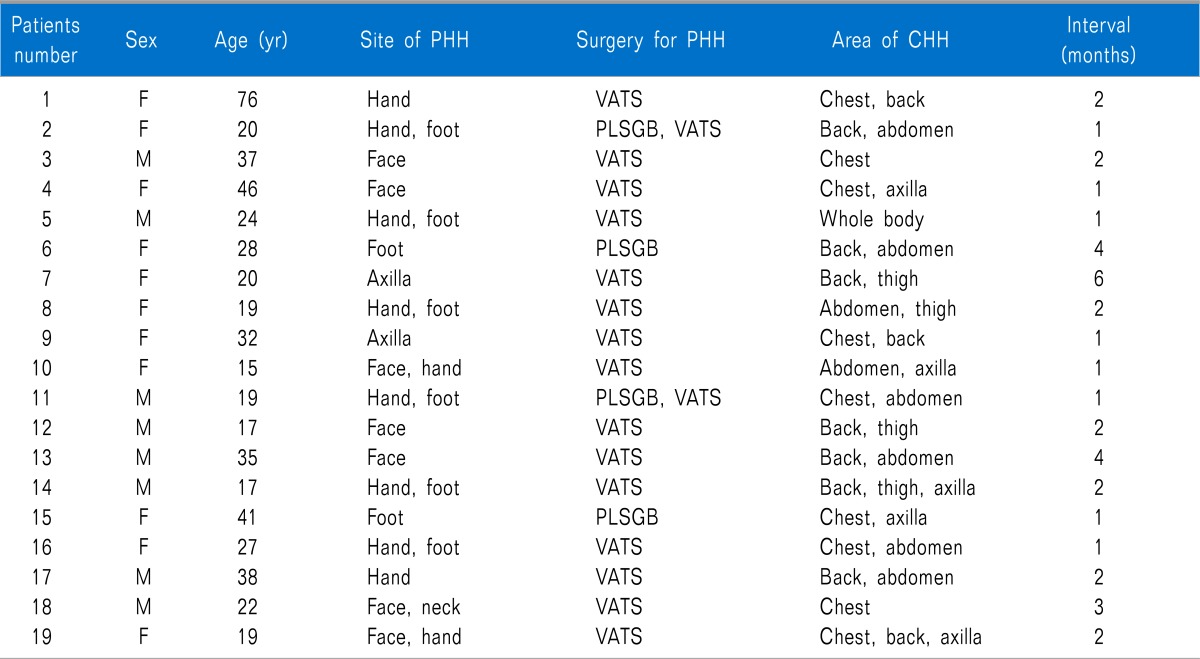
The study was conducted on patients who visited our pain clinic from April 1, 2007 to February 28, 2012 and were diagnosed with compensatory hyperhidrosis. Various treatment methods were explained to each patient. Among the patients who decided to take glycopyrrolate (Glycopyrrolate®, Myungmoon Pharmaceuticals, Seoul, Korea), 19 were chosen for the study; these patients had diligent physical examination records, completed interviews and questionnaires before and after administration, and satisfied the following conditions: the research subjects were a) at least 10 years old and less than 80 years old; b) diagnosed with compensatory hyperhidrosis on the first visit or diagnosed with compensatory hyperhidrosis due to hyperhidrosis that developed after receiving thoracic sympathectomy or lumbar sympathetic ganglion block using 99% alcohol for primary hyperhidrosis; c) diagnosed with compensatory hyperhidrosis but ascertained as having no underlying diseases through the thyroid function test, electrocardiography, simple chest PA, and blood test; d) excluded from asthma, voiding difficulty, glaucoma, and heart disease through interviews; and e) able and willing to diligently respond to the questionnaire (Table 1).
The questionnaire was given twice, during the first clinic visit and during the clinic visit 1 month after administration of the drug. Glycopyrrolate 1mg was administered twice as the first administration dosage. Depending on the presence of side effects, the dosage was increased 2 mg every day up to a maximum of 8 mg. When side effects occurred and discomfort was felt in everyday life, the dosage was reduced to the dosage before the occurrence of side effects. Side effects from glycopyrrolate were checked every week through a questionnaire, interview, observation, and physical examination. The questionnaire recorded age, sex, period when hyperhidrosis developed after surgery or nerve block, physical state, medical history, allergies, medication history, underlying disease, family history, and area of perspiration. The Milanez de Campos scale questionnaire was used to evaluate the degree of improvement in symptoms, and the scores before and after administration were compared. The function of the autonomic nervous system (ANS), comprising 90 questions, was also compared. Other than the direct measurement of hyperhidrosis symptoms, changes in patient psychology were compared by using the Modified Beck Depression Inventory (BDI) [2] and the Beck Anxiety Inventory (BAI) [3].
The characteristics of each patient were analyzed through the mean value for each category and paired t-test, and these were used to compare the changes before and after administration of the medication. The Wilcoxon signed-rank test was used for analysis of several categories that did not follow a normal distribution, and each category before and after administration was compared through nonparametric statistical analysis. SPSS 12.0.1 (SPSS Inc., Chicago, IL, USA) was used for all analysis. Statistical significance was defined as P < 0.05.
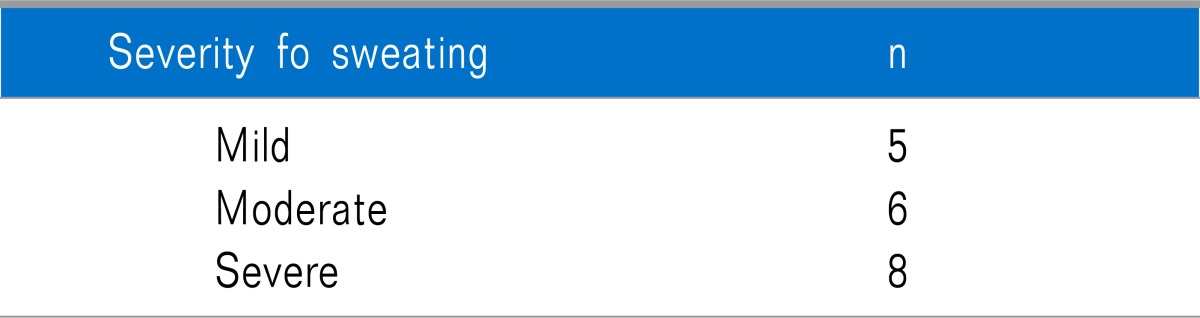
The objective degree of hyperhidrosis was based on the scale suggested by Lai et al., and it was divided into mild (underwear does not become wet), moderate (underwear become swet but not enough to warrant changing), and severe (underwear has to be changed) (Table 2) [3].
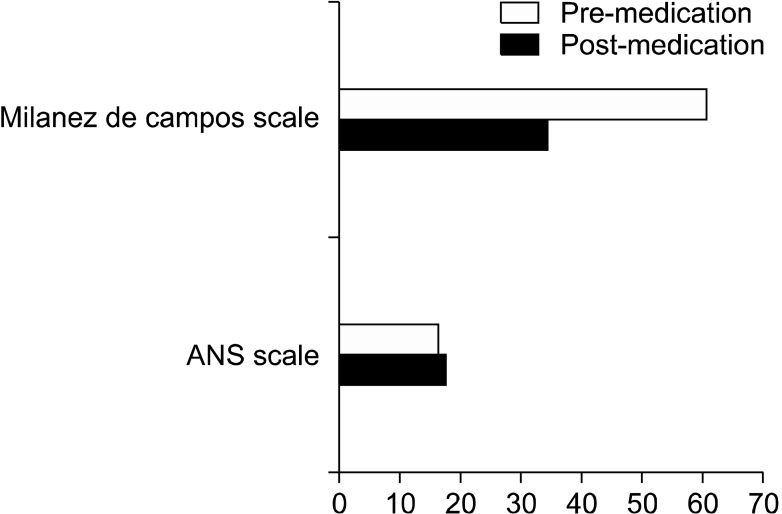
According to the Milanez de Campos scale, which measures the everyday discomfort experienced by patients due to hyperhidrosis, there was an 89% reduction in the score from before administration to after 1 month. The mean score before administration was 60.4, whereas the mean score on the Milanez de Campos scale after taking glycopyrrolate decreased to 34.2. This was statistically significant (P < 0.05) (Fig. 1).
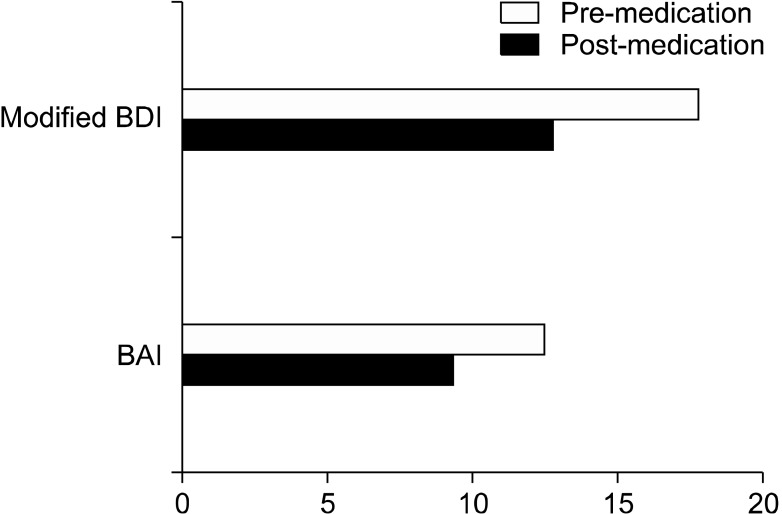
The Modified Beck Depression Inventory, which shows the degree of depression, also decreased in 89% of patients. The mean score decreased from 17.8 before administering glycopyrrolate to 12.8 a month after administration. This was also statistically significant (P < 0.05) (Fig. 2).
In the Beck Anxiety Inventory, which measures anxiety in everyday life felt by patients due to hyperhidrosis, the score was reduced in 79% of patients. Before administration of glycopyrrolate, the mean score was 12.5; one month after administration, the mean score fell to 9.3. This was also statistically significant (P < 0.05) (Fig. 2).
The ANS score, which examines the symptom of the Autonomic Nervous System before and after medication, increased slightly from 16.1 to 17.3 after medication, but there was no statistical significance (P > 0.05) (Fig. 1).
Side effects appeared in 8 patients (42%) during administration of glycopyrrolate; 3 had dry mouth (17.5%), 3 had palpitation (17.5%), and there was 1 patient each with constipation and headache (5%), but there were no instances of discontinuing medication because of side effects.
Go to : 
Compensatory hyperhidrosis is defined as the occurrence of post-operative perspiration exceeding the level of perspiration necessary for temperature control in areas where there had been no hyperhidrosis before surgery; it can be divided into mild, moderate, and severe hyperhidrosis [4,5]. The symptoms of compensatory hyperhidrosis can appear immediately after surgery or permanent sympathectomy and maybe triggered by changes in climate or temperature, emotional changes, or anxiety. When the symptoms are severe, underwear or socks have to be changed several times a day. This can have a serious effect on the everyday life of individuals and lead to psychological stress and depression.
The incidence of compensatory hyperhidrosis after sympathectomy is reported to be around 59.8-90% [6-8]. The precise mechanism of compensatory hyperhidrosis has not yet been revealed, but it is thought to result from aberrant functioning of the sympathetic nervous system after surgery. Lin and Telaranta [9] argued that the destruction of the nerve flex arch between the sympathetic nervous system and the hypothalamus was the main mechanism of compensatory hyperhidrosis after sympathectomy. Therefore, they suggested that maintaining negative afferent stimulation by returning to the hypothalamus during surgery was the key point in preventing the occurrence of post-operative compensatory hyperhidrosis.
The main goals of treating patients with compensatory hyperhidrosis are to maximize their quality of life and to maintain their social functioning, including occupation, by reducing or controlling excessive sweating [10]. Initially, simple non-pharmacologic treatments that can be performed at home include weight control, non-thermogenic diet, and physical exercise. Generally, it is known that increased body mass index (BMI) is related to increased perspiration. Therefore, patients with compensatory hyperhidrosis should work towards reducing perspiration by maintaining their BMI in the normal range [11].
From treatment using medications, topical application of aluminium salts showed a reduction in sweating of 60-80% in patients with compensatory hyperhidrosis, and the effect appears approximately 48 hours after application [12]. Skin irritation is reported as a side effect, however, and this sometimes leads to discontinuing treatment.
Subcutaneous injection of botulinum toxin is a new treatment method that has an anticholinergic effect in the sympathetic cholinergic nerve endings distributed in the neuromuscular junction and sweat glands. The duration of perspiration suppression is reported to vary widely [13,14]. The subcutaneous botulinum toxin injection is administered after performing the Minor's test, and the effect continues for 4 months or more. In some cases, it has even resulted in permanent reduction of perspiration.
Orally administered anticholinergic medications have been used for at least the past 30 years; propantheline, glycopyrrolate, oxybutynin, and benztropine are known to be effective. With regard to mechanism, anticholinergic medications are known to suppress the secretion of acetylcholine in the nerve endings distributed in the sweat glands. However, side effects such as dry mouth, constipation, voiding difficulty, tachycardia, digestive system dysfunction, and dizziness can occur due to their suppression of the sympathetic nervous system, and another drawback is that anticholinergic medications cannot be used in patients with glaucoma or urologic disease [2].
The limitations of this study include, first and foremost, the insufficient study population due to subject selection restrictions and subjects' lack of diligence in taking medication, visiting the clinic, and answering the questionnaire. Secondly, there was a limitation in securing objectivity of a certain level because all data before and after oral administration of glycopyrrolate were measured through patient questionnaires. Thirdly, due to the insufficient number of subjects, analysis could not be performed according to the degree of symptoms of hyperhidrosis. A fourth limitation is that proper analysis was not performed regarding the location of excision in the laparoscopic thoracic sympathectomy or location of the lumbar sympathetic ganglion block.
Various methods have been suggested for the treatment of compensatory hyperhidrosis. Anticholinergic agents, especially glycopyrrolate, can be taken easily without serious complications and pose no particular economic or social difficulties. Another merit of this medication is that effective suppression of perspiration appears even when it is not used consistently, but only as needed. Hence, the authors suggest that oral administration of glycopyrrolate can be helpful as the primary treatment for compensatory hyperhidrosis.
Go to : 
References
1. Sato K, Kang WH, Saga K, Sato KT. Biology of sweat glands and their disorders. II. Disorders of sweat gland function. J Am Acad Dermatol. 1989; 20:713–726. PMID: 2654213.

2. Kim WO, Yoon DM, Kil HK, Kim JI, Choi BI. Effect of oral glycopyrrolate in essential hyperhidrosis. Korean J Anesthesiol. 2004; 46:298–301.

3. Lai YT, Yang LH, Chio CC, Chen HH. Complications in patients with palmar hyperhidrosis treated with transthoracic endoscopic sympathectomy. Neurosurgery. 1997; 41:110–113. PMID: 9218302.

4. Adar R, Kurchin A, Zweig A, Mozes M. Palmar hyperhidrosis and its surgical treatment: a report of 100 cases. Ann Surg. 1977; 186:34–41. PMID: 879872.
5. Chou SH, Kao EL, Li HP, Lin CC, Huang MF. T4 sympathectomy for palmar hyperhidrosis: an effective approach that simultaneously minimzes compensatory hyperhidrosis. Kaohsiung J Med Sci. 2005; 21:310–313. PMID: 16089308.

6. Fredman B, Zohar E, Shachor D, Bendahan J, Jedeikin R. Video-assisted transthoracic sympathectomy in the treatment of primary hyperhidrosis: friend or foe? Surg Laparosc Endosc Percutan Tech. 2000; 10:226–229. PMID: 10961751.

7. Lin TS, Wang NP, Huang LC. Pitfalls and complication avoidance associated with transthoracic endoscopic sympathectomy for primary hyperhidrosis (analysis of 2200 cases). Int J Surg Investig. 2001; 2:377–385.
8. Gossot D, Galetta D, Pascal A, Debrosse D, Caliandro R, Girard P, et al. Long-term results of endoscopic thoracic sympathectomy for upper limb hyperhidrosis. Ann Thorac Surg. 2003; 75:1075–1079. PMID: 12683540.

9. Lin CC, Telaranta T. Lin-Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol. 2001; 90:161–166. PMID: 11695784.
10. Lyra Rde M, Campos JR, Kang DW, Loureiro Mde P, Furian MB, Costa MG, et al. Guidelines for the prevention, diagnosis and treatment of compensatory hyperhidrosis. J Bras Pneumol. 2008; 34:967–977. PMID: 19099105.
11. de Campos JR, Wolosker N, Takeda FR, Kauffman P, Kuzniec S, Jatene FB, et al. The body mass index and level of resection: predictive factors for compensatory sweating after sympathectomy. Clin Auton Res. 2005; 15:116–120. PMID: 15834768.
12. Nascimento LP, Raffin RP, Guterres SS. Aspectos atuais sobre a segurança no uso de produtos antiperspirantes contendo derivados de aluminio. Infarma. 2004; 16:66–72.
13. Guntinas-Lichius O. Increased botulinum toxin type A dosage is more effective in patients with Frey's syndrome. Laryngoscope. 2002; 112:746–749. PMID: 12150533.

14. Naumann M. Evidence-based medicine: botulinum toxin in focal hyperhidrosis. J Neurol. 2001; 248(Suppl 1):31–33. PMID: 11357238.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download