Abstract
Hemifacial spasm is defined as unilateral, involuntary, irregular twitching of all or parts of the muscles innervated by facial nerves. Here, we present a case of recurrent hemifacial spasm after microvascular decompression (MVD) treated with pulsed radiofrequency (PRF) treatment with good results. A 35-year-old woman suffered from recurrent hemifacial spasm after MVD that was refractory to medical treatment and botulinum toxin injections. We attempted a left facial nerve block twice. Then, we applied PRF at a maximum temperature of 42℃ for 120 sec. Some response was observed, so we applied PRF two additional times. The frequency of twitch decreased from 3-4 Hz to < 0.5 Hz, and subjective severity on a visual analogue scale also decreased from 10/10 to 2-3/10. PRF treatment might be an effective medical treatment for refractory hemifacial spasm and has fewer complications and is less invasive compared with those of surgery.
Hemifacial spasm (HFS) is defined as involuntary and irregular tonic, clonic movement of muscles innervated by the ipsilateral facial nerve [1]. Spasms usually begin with twitching of the lower eyelid, followed by involvement of other periorbital, facial, perioral, and platysma muscles [1]. This disorder may be caused by a lesion, such as a tumor, a cyst, an aneurysm, an arteriovenous (AV) malformation, or vascular compression of facial nerve. But, the precise pathophysiology remains unclear [2]. Several treatment options are available such as medical therapy, local botulinum toxin injections, facial nerve block, and surgical treatment. Pulsed radiofrequency (PRF) has been used since the mid-1970s and offers the advantage of pain control without tissue destruction and painful sequelae [3]. PRF is commonly used to treat facial pain. Here, we present a case of recurrent HFS after microvascular decompression (MVD) that was treated with PRF with good results.
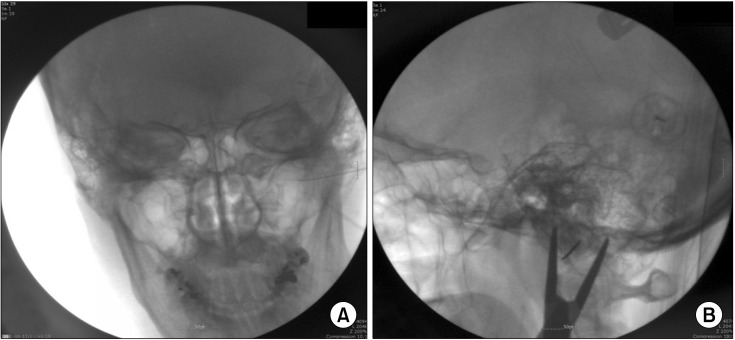
A 35-year-old woman developed MVD due to a left HFS 6 years ago, which was refractory to medical treatment. Results of preoperative brain magnetic resonance image and electromyography were normal. Surgery was successfully performed, and the postoperative findings revealed that the branch of the left anterior inferior cerebellar artery had been compressing the VII-VIII cranial nerve complex. The pateint did not show any specific symptoms for about 3 and a half years after MVD. But, the symptoms began to recur 1 year ago and she was medicated with 0.5 mg clonazepam for 3 months, and received two local botulinum toxin injections. No treatment effect occurred, so she visited our pain clinic. The patient was experiencing a twitch on the infraorbital area and chin when the HFS was severe, and spasm frequency was 3-4 Hz. Discomfort on the visual analogue scale (VAS) was 10/10. We initially attempted a left stellate ganglion block twice, but no effect was observed, Then, we performed a fluoroscope-guided left facial nerve block twice using 4 ml of 2% lidocaine, and 20 mg triamcinolone. No complications occurred, and the HFS symptoms were relieved for 4 days. Thus, we decided to perform PRF on the facial nerve. In the right lateral decubitus position, the patient's chin was slightly lifted, which exposed the mastoid process. Both sides of the mastoid process and mandible were superimposed on a lateral fluoroscope imaging view (Fig. 1). The skin was prepared with betadine and aseptic draping. We used a 10 cm, 22-G Sluijter-Mehta cannula needle with a 0.5 mm active tip and verified accurate needle position by fluoroscopy. A 5 mm skinwheal appeared from the mastoid process to the nose beginning at the needle entry point of the local anesthetic. We explored facial nerves with 50 Hz, 0.5 V sensory stimulation to the tongue and 2 Hz, 1.0 V motor stimulation to the left hemi face when the tip of the needle was positioned around the stylomastoid for amen. We administered three PRF pulses at 42℃ for 120 seconds after confirming that the needle tip was near the facial nerve. After the procedure, we injected 3 ml of 4% lidocaine mixed with 20 mg triamcinolone. The patient was symptom free for only 4 days, so we applied additional PRF treatments twice using the same method to obtain a longer effect. When the patient returned as an outpatient 1 week after the second PRF treatment, HFS frequency was improved to < 0.25 Hz, and subjective complaints improved on the VAS (2-3/10). The modified MacNab criteria at 1 week after the procedure were good. The patient was followed up at 3, 6, 9, and 12 months via telephone, and symptom relief was maintained continuously.
Idiopathic HFS is a rare disorder with a 1 year prevalence of 1 in 10,000 people [4]. The cause of HFS is unclear, but it may be caused by a lesion such as a tumor, a cyst, an aneurysm, an AV malformation, an intrinsic brain stem lesion, or a bony lesion of the cranium in the cerebellopontine angle [2]. Several medical and surgical treatments can cure HFS but may only temporarily relieve HFS [5]. Hence, sole use of medical and nonsurgical treatment is rarely effective and can cause adverse effects. A local botulinum toxin injection in the branch of the facial nerve is effective in 75-100% of cases but the duration of relief varies from 4-24 weeks [6]. Therefore, this treatment can be repeated but the expense is high. MVD success rate is relatively high compared with other treatments. Cure rates with the use of MVD vary from 38.2-87.9% [7]. At the last follow-up report, 1-3 years after surgery, the successful spasm relief rate increased to 79-94.6% [7]. But, MVD is invasive and unacceptable to elderly patients or those with severe systemic disease, as there is a chance for temporary or permanent hearing loss, facial weakness, lower cranial nerve dysfunction, and complications such as an intracranial infection. The recurrence rate of HFS after MVD is up to 20% [6]. Similar to preoperative HFS, the cause of recurrent HFS after successful MVD remains unclear. The causes of recurrence may be incomplete vascular decompression or relapse of vascular compression [8]. Repeated MVD for HFS can be an effective procedure, but complication rates are probably higher than those for the first procedure. Engh et al. suggested an HFS treatment algorithm [9] in which patients who are refractory to MVD have three options such as to live with their disease, undergo botulinum therapy, or undergo repeat MVD [9].
PRF is a unique technology that provides pain relief without causing any significant damage to nervous tissue. The mechanism by which PRF controls pain is unclear, but it may involve a temperature-independent pathway mediated by the rapidly changing electrical field [3]. Higachi et al. reported that PRF treatment is associated with a significant number of c-fos immunoreactive neurons in the dorsal horn [10]. PRF can be used to treat neuropathic pain with fewer complications because it does not destroy nerves or block their transmission, whereas conventional heat RF is not used frequently for neuropathic pain because it destroys nerves [3]. PRF is safe and less risky and takes a relatively shorter time compared with that of surgery; thus, it can be applied to risky areas. Our patient did not want additional facial nerve surgical exploration, so we applied PRF. HFS was controlled very effectively after the procedure without complications such as facial muscle weakness or dysethesia of the tongue.
PRF treatment of facial nerves might be effective for patients with intractable and recurrent HFS who are refractory to medical treatment and reject a surgical option.
References
1. Yaltho TC, Jankovic J. The many faces of hemifacial spasm: differential diagnosis of unilateral facial spasms. Mov Disord. 2011; 26:1582–1592. PMID: 21469208.

2. Payner TD, Tew JM Jr. Recurrence of hemifacial spasm after microvascular decompression. Neurosurgery. 1996; 38:686–690. PMID: 8692385.

3. Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008; 12:37–41. PMID: 18417022.

4. Fraioli MF, Moschettoni L, Fraioli C, Strigari L. Treatment of idiopathic hemifacial spasm with radiosurgery or hypofractionated stereotactic radiotherapy: preliminary results. Minim Invasive Neurosurg. 2010; 53:34–36. PMID: 20376743.

6. Tan NC, Chan LL, Tan EK. Hemifacial spasm and involuntary facial movements. QJM. 2002; 95:493–500. PMID: 12145388.

7. Li S, Hong W, Tang Y, Ying T, Zhang W, Li X, et al. Re-operation for persistent hemifacial spasm after microvascular decompression with the aid of intraoperative monitoring of abnormal muscle response. Acta Neurochir (Wien). 2010; 152:2113–2118. PMID: 20936485.

8. Yamaki T, Hashi K, Niwa J, Tanabe S, Nakagawa T, Nakamura T, et al. Results of reoperation for failed microvascular decompression. Acta Neurochir (Wien). 1992; 115:1–7. PMID: 1595390.

9. Engh JA, Horowitz M, Burkhart L, Chang YF, Kassam A. Repeat microvascular decompression for hemifacial spasm. J Neurol Neurosurg Psychiatry. 2005; 76:1574–1580. PMID: 16227555.

10. Higuchi Y, Nashold BS Jr, Sluijter M, Cosman E, Pearlstein RD. Exposure of the dorsal root ganglion in rats to pulsed radiofrequency currents activates dorsal horn lamina I and II neurons. Neurosurgery. 2002; 50:850–855. PMID: 11904038.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download