INTRODUCTION
Nowadays, the C-arm fluoroscope is an invaluable tool for the intervention of pain. However, the danger of radiation exposure is well acknowledged. Ionizing radiation can cause both somatic and genetic damage. Examples are seen in squamous cell carcinomas of the hands, leukemia, thyroid cancers, stomach cancers, and birth defects [
1]. It is common practice to wear lead aprons during fluoroscopy-guided procedures, and many pain physicians use thyroid shields routinely. Lead gloves, however, are not routinely used by pain physicians [
2]. During fluoroscopy-guided procedures, pain physicians may be at risk from ionizing radiation both directly from the primary beam and indirectly via scattered radiation. The occupational dose limits, recommended by the International Commission on Radiology Protection, have been adopted by most countries in the world, including the European Union and the United States [
3]. The limit for radiation dose is 20 mSv per year, averaged over a defined period of 5 years [
4].
The aim of this study was to assess the radiation exposure doses in the hand and chest of pain physicians during C-arm fluoroscopy-guided procedures.
Go to :

MATERIALS AND METHODS
This study was conducted from May to August of 2012. This is a prospective study about radiation exposure experienced by pain physicians during transforaminal epidural steroid injection (TFESI) and medial branch block (MBB). The pain physicians consisted of four doctors (one professor, and three fellows). The physician represented as the professor has more than 40 months of experience and the three fellows have 3 to 6 months of experience.
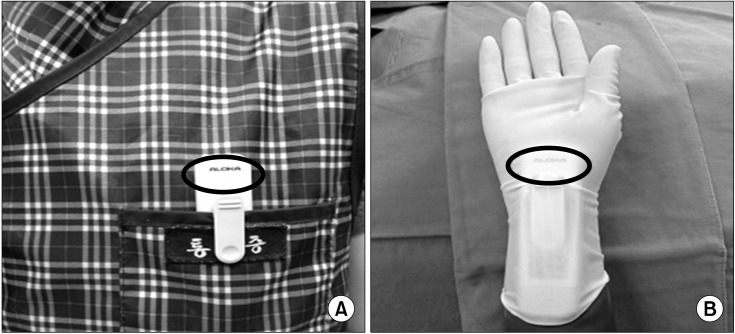
Two dosimeters were used to record the radiation exposure. One (PDM-127, Aloka, Tokyo, Japan) was worn on the palmar aspect of the right hand (
Fig. 1A). The other (PDM-227, Aloka, Tokyo, Japan) was worn on the left side of the chest over the lead apron (
Fig. 1B). The effective doses (ED) at each physician's hand and chest were measured from direct reading dosimeters. Exposure times and the radiation absorbed doses (RAD) were collected from the C-arm fluoroscope (OEC 9800 Plus, GE healthcare, Salt Lake City, Utah). Immediately after X-ray scanning by C-arm fluoroscopy, the distance from the center of the X-ray field to the physician during X-ray scanning was also investigated. When we checked real-time fluoroscopy, we administrated contrast media through a 75-cm-long extension tube. We reviewed patients' medical records to collect their age, height, and weight.
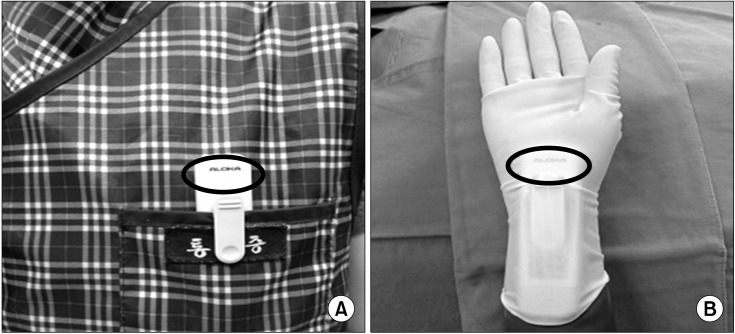 | Fig. 1Two dosimeters were used to record the radiation exposure. (A) One was worn on the left chest over the lead apron. (B) The other was worn on the palmar aspect of the right hand. Circle: detector of dosimeter. 
|
All statistical analyses were performed on SPSS version 17. Interphysician comparisons of the demographic data, such as age, weight, height, and sex of the patients, along with distance from the X-ray field, time, ED, and RAD were analyzed by ANOVA and Turkey's multiple comparisons test. The ratio of male/female for each group was compared using a chi-square test. Statistical significance was defined as P < 0.05.
Go to :

RESULTS
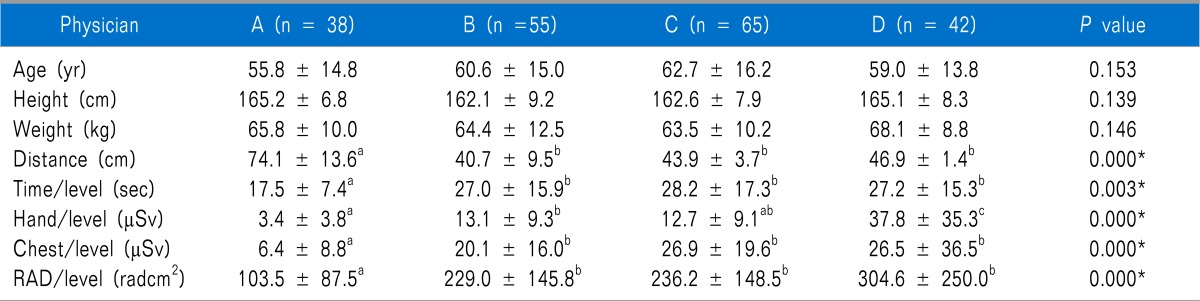
Three hundred and fifteen cases were included for this study. The number of cases in the TFESI and MBB analysis were 200 and 115, respectively. The ratios between males and females for the two groups were 88:112 and 64:37. There were no significant differences in the patient's sex, age, height, and weight among each of the physicians (
Table 1,
2). In the TFESI group, there were statistically significant differences in the distance from the X-ray, exposure time, and ED at the hand and chest, as well as RAD between the physicians (
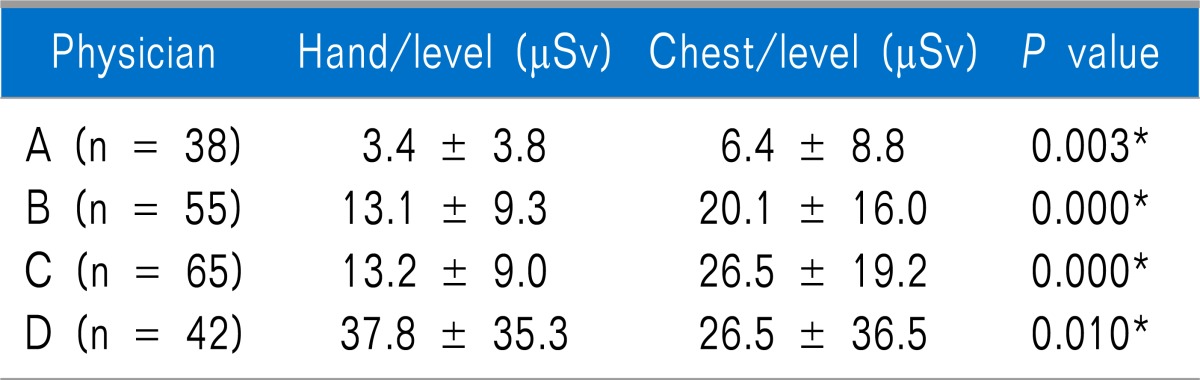
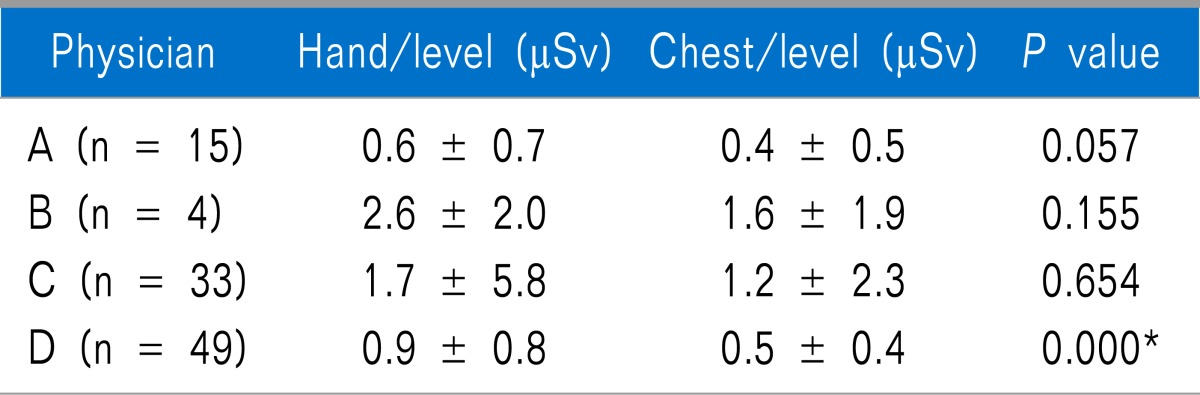
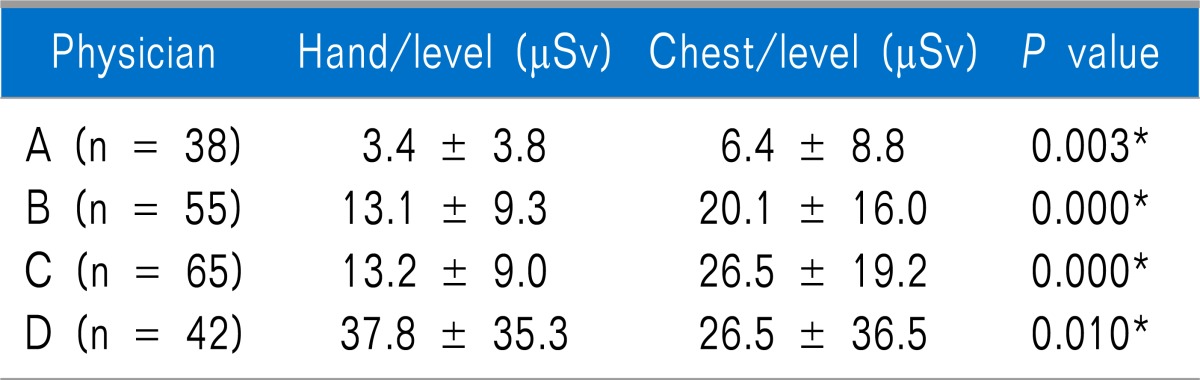
Table 1). The distance from the center of the X-ray field to physician A was more than that of the other physicians, and the exposure time, ED, and RAD in physician A were less than that of the other physicians. ED at the hand of physician D was more than that of the other physicians. There were significant differences between ED of the hand and ED of chest in all the physicians (
Table 3). In physician A, B and C, the ED at the chest was more than the ED at the hand. In physician A, the lowest dose was received at the hand and chest, while the distance from the X-ray field was the furthest among the physicians (
Table 1).
Table 1
Demographic and Radiation Related Data in Transforaminal Epidural Steroid Injection
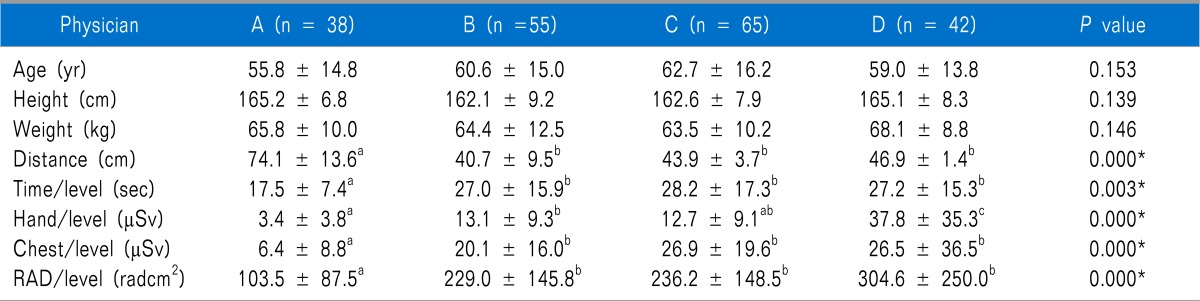

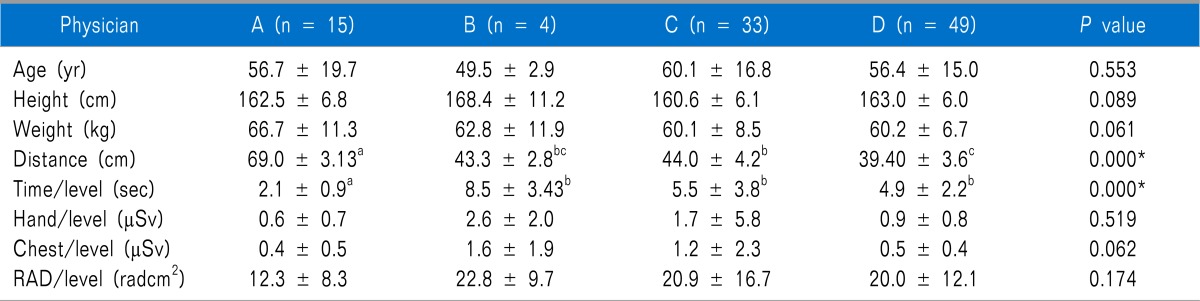
Table 2
Demographic and Radiation Related Data in Medial Branch Block
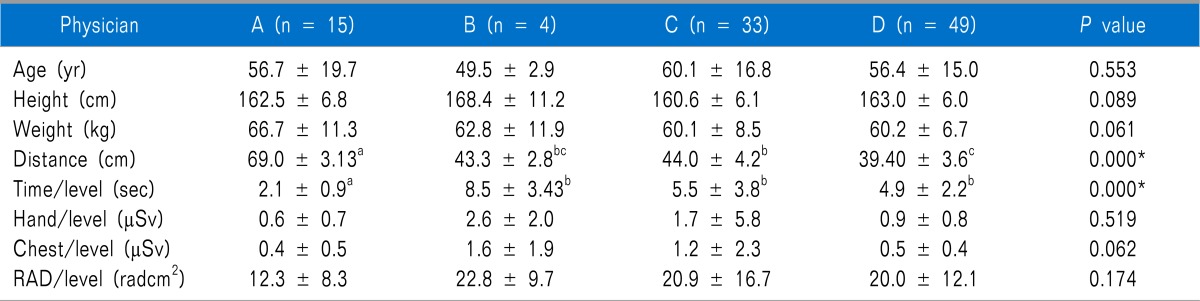

Table 3
Radiation Dose at the Hand and Chest in TFESI

In the MBB group, there were no differences between the ED at the hand and chest, except for physician D (
Table 4). There were statistically significant differences in the distance from the X-ray field and exposure time between the physicians (
Table 2). However, there were no differences in the ED and RAD between the physicians. The distance from the center of the X-ray field to physician A was more than that of the other physicians, and the exposure time for physician A was less than that of the other physicians (
Table 2,
4).
Table 4
Radiation Dose at the Hand and Chest in MBB

Go to :

DISCUSSION
Radiation has the potential to cause harm, as well as provide benefits during medical use. Thus, limiting the potential risks from radiation exposure in these procedures is essential, while physicians must remember that there is no dose below which there is zero risk [
5]. The adverse effects of ionizing radiation on the human body include skin diseases, thyroid cancers, brain tumors, and cataracts [
6]. The degree of the risks to health from radiation is primarily dependent on intraoperative exposure time, cumulative career exposure, and the effectiveness of the utilized protective measures [
7,
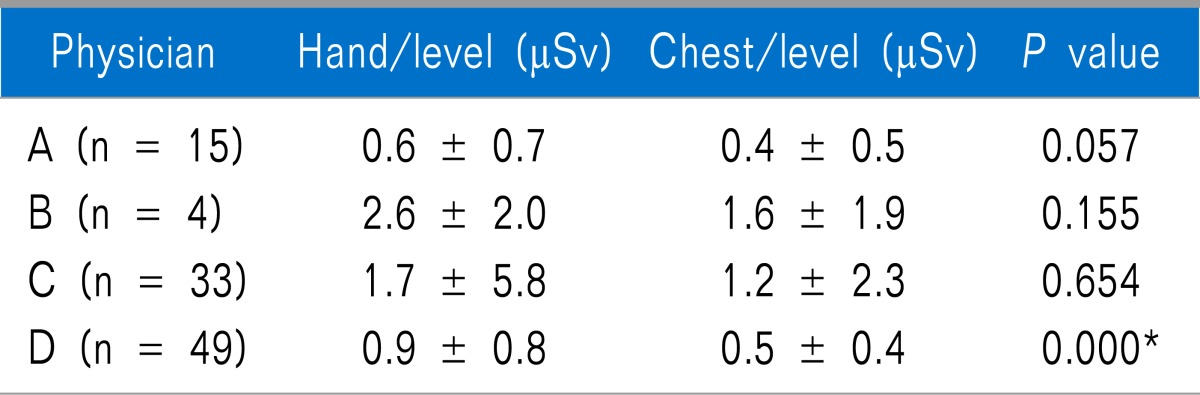
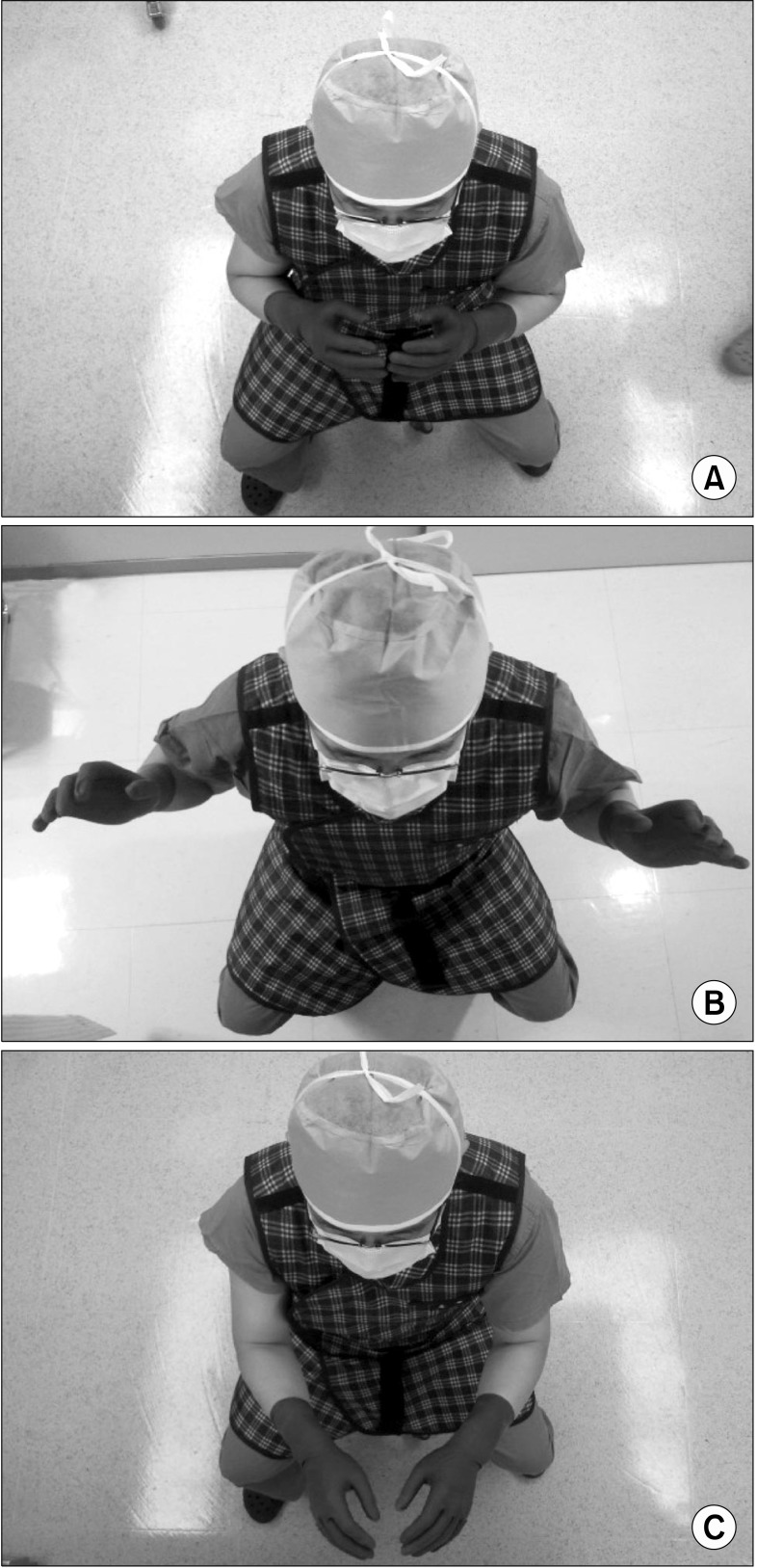
8]. The ED of the hand depends on the position of the physician's hands.
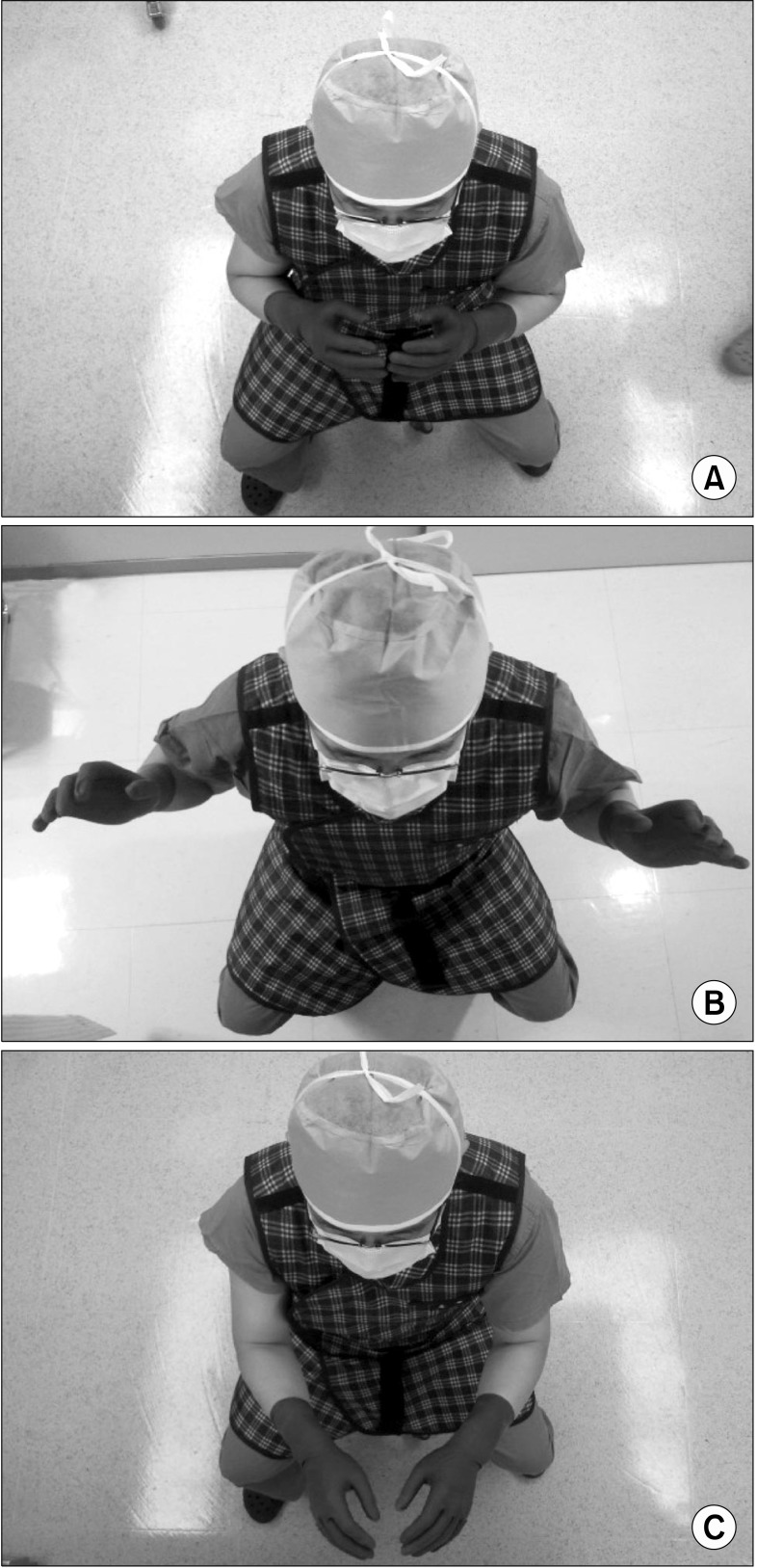
Fig. 2 and
3 show various positions of the hands and the distance from the field during X-ray scanning. The hand dosimeter was worn only on the palmar aspect of the right hand. Therefore, the ED was not measured at the dorsum of the hand, but at the palm of the hand. If the physician's palm faced the opposite side of the radiation source, ED at the hand for this study would be decreased. Although the hand was closer than the chest in physician A during TFESI, the radiation detector faced the opposite side from the radiation source during X-ray scanning, which could be related to a less effective dose than that of the chest. The mean ED at the hand of physician D was the highest during TFESI. The physician's palm faced the radiation source for a longer duration than the others during the procedures (
Fig. 2). However, the dorsum of the hand faced the radiation field during fluoroscopy by physician A, while it was still further from the radiation source than the chest of physician B and C. Therefore, the mean ED at the hand could be less than the mean ED at the chest in physician A, B, and C during TFESI. Although the distance and time were different, there were no significant differences in the ED at the hand and at the chest, along with the RAD among the physicians during MBB. The causes were thought to be due to MBB being a simple procedure, with the differences of ED and RAD being very small among the physicians. Moreover, the physicians did not check for real-time fluoroscopy during the MBBs, and the physicians could easily master this skill even though some had relatively low experience. Unlike the other physicians, the ED of the hand of physician D was higher than the ED of the chest. Physician D's hand was located closer than his chest during the entire procedure, and the palm of his hand faced the radiation source for a longer duration than the other physicians. The time, RAD, and ED at the hand and chest of physician A were the lowest of all the physicians during TFESI. The causes of these results are thought to be due to physician A (professor) being the most experienced pain physician compared to the others, and kept a longer distance from the radiation source than the others. From these results, it can be inferred that experience and long-distance can be related to a lower radiation dose when performing complicated procedures like TFESI.
 | Fig. 2Various position of hands during X-ray scanning. (A) Physician A's position, (B) Physician B and C's position, (C) Physician D's position. 
|
 | Fig. 3The positions of each physician's hand which was looked down. (A) Physician A's position, (B) Physician B and C's position, (C) Physician D's position. 
|
In the MBB group, the hand and chest positions of the physicians, along with their experience, did not influence radiation exposure. However, in the TFESI groups, it was shown that the hand and chest positions, distance from the radiation source, and the physician's experience influenced radiation exposure.
We believe that MBB is a simple and easy procedure. Therefore, the technique and physician's position had little impact on radiation exposure. Previous studies, investigating the relationship between experience level and radiation exposure, showed that less experienced surgeons received higher radiation doses [
9,
10]. These results are also reflected in our study, where the 3 fellows (physician B, C and D) have an increased duration in time and radiation exposure during C-arm fluoroscopy-guided procedures. Arnstein et al. [
11] performed a cadaveric study, which showed that radiation exposure is 100 times greater at 15 cm from the radiation source compared to 30 cm. There are three protective measures which can limit the exposure from the primary and scatter radiation source. First, maintaining a safe distance from the primary beam can greatly reduce the radiation dose. Physicians should be familiar with the Inverse Square Law related to radiation safety, which states that the exposure rate from a point source of radiation is inversely proportional to the square of the distance from the source [
12]. At a distance of 2 meters, exposure is 0.025% of the direct beam intensity [
13]. Second, protective garments can effectively reduce radiation exposure of the physicians. Lead aprons, of 0.5 mm thickness, have been shown to shield approximately 99% of the potential radiation dose [
13,
14]. Radioprotective glasses, gloves, thyroid shields, and drapes can provide additional shielding and protection for sensitive tissues. A third protective measure is to operate the C-arm fluoroscopy in such a way as to minimize exposure. Using the pulsed and low-dose modes rather than conventional fluoroscopy, whenever possible, can reduce radiation doses [
15-
17].
This study contains the limitation of not measuring the radiation dose of the dorsum of the hand, but only measuring the palm of the hand. If we also measured the radiation dose of the dorsum of the hand, the amount of radiation to the hand would be more than that of the chest.
In conclusion, the physician's distance from the radiation source, position of the hand, experience and technique can correlate with the radiation dose in complicated procedures such as TFESI. Therefore, for radiation safety, we have to make efforts to keep our hands and body at a distance from the radiation field, while attempting to master the skills for interventional pain procedures.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download