INTRODUCTION
The key strategy in promoting postoperative recovery is early ambulation after surgery [1]. However, early ambulation is difficult when there is orthostatic intolerance, which is characterized by having difficulty maintaining a sitting and/or upright position due to symptoms from cerebral hypoperfusion, such as dizziness, nausea, feeling of heat, blurred vision, and syncope [2]. In the sitting and/or upright position, gravity pulls blood towards the abdomen or legs, and it is easy for postoperative patients to have a reduced central blood volume when maintaining a sitting and/or upright position due to an insufficient amount of fluids or blood during surgery. Especially, use of premedication, anesthesia, postoperative analgesia, and drugs can reduce arterial pressure, cerebral blood flow, and oxygenation; therefore, it can further affect orthostatic intolerance [3].
In ambulatory surgery, temporary instability during first ambulation after surgery is the largest cause for extending a hospital stay [4]; however, there is only a small amount of research regarding the occurrence and duration of orthostatic intolerance developing in patients after major surgery. There is minimal research in Korea regarding orthostatic intolerance in surgical patients using patient controlled analgesia, while most of the research has been on the prevention and treatment of nausea and vomiting caused by the administration of drugs when using patient controlled analgesia [5]. In research done in other countries, there has only been research on orthostatic intolerance for early ambulation and cardiovascular response [1] and on orthostatic intolerance occurring 1 hour after anesthesia related to sex and age [6], and after an exhaustive search, no studies were found on the relationship of orthostatic intolerance with opioid analgesics used in patient controlled analgesia. Especially, there is nearly no research on the orthostatic intolerance of postoperative patients using patient controlled analgesia.
Hence, the aims of this study were to investigate the factors related to the manifestation and frequency of orthostatic intolerance in surgical patients using patient controlled analgesia, to examine how orthostatic intolerance can be prevented and to determine whether appropriate nursing management is necessary.
Go to : 
MATERIALS AND METHODS
This research was approved by the Institutional Review Board and carried out on 175 adult patients that underwent an open or laparoscopic gastrectomy as elective surgery who were managing postoperative pain with patient controlled analgesia.
Patients who had headache, dizziness, nausea, vomiting, double vision, and postural hypotension before surgery were excluded from the study as well as patients who stopped the use of patient controlled analgesia during the investigation period, patients who were unable to stand up, patients who used beta-blockers, patients who were ASA III or above, patients who were alcoholics, and patients who developed cardiac arrest.
All patients were IV injected midazolam 2 mg and lidocaine 40 mg as premedication before inducing anesthesia. Target controlled infusion pump (Orchestra, France) was used to inject propofol (induction 2 mg/kg/hr, plasma concentration 1-1.7 ug/ml) and remifentanil (plasma concentration 5 ng/ml). Vecuronium 0.1 mg/kg was IV injected to enable endotracheal intubation, and 0.01-0.015 mg/kg was administered in 30 minute intervals as a maintenance dosage. Thirty minutes before the end of the surgery, fentanyl 100 ug was IV injected to prevent pain, while ondancetron 4 mg was IV injected to prevent nausea and vomiting. At the end of surgery, glycopyrrolate 0.4 mg and neostigmine 15 mg were IV injected to recover from muscle relaxants. To manage pain in the recovery room, fentanyl 50 mcg was administered from 0 to 3 times depending on the degree of pain. The mixture of drugs in the patient controlled analgesia used by the subjects after surgery was as follows. Fentanyl 1,500 ug, ketorolac 180 mg, and ondansetron 8 mg were mixed with normal saline made up to a total volume of 100 ml for normal adults. Subjects who were 65 years or older or subjects with a weight of 50 kg or lower were provided with a mixture of fentanyl 1,300 ug, ketorolac 180 mg, and ondansetron 8 mg made up to a total volume of 100 ml with normal saline. When there were problems in liver or kidney function, fentanyl 1,600 ug and ondansetron 8 mg were mixed with normal saline made up to a total volume of 100 ml. Finally, subjects who were 65 years or older or weighed 50 kg or lower together with liver or kidney function problems, were provided with a mixture of fentanyl 1,400 ug and ondansetron 8 mg made up to a total volume of 100 ml with normal saline. The patient controlled analgesia (Automed, Korea) was set at basal rate of 1 ml/hr, bolus rate 1 ml/dose, and a lockout-time of 15 minutes. The pain until first ambulation at the ward was measured by the NRS (Numerical Rating Scale), and when the patient complained of pain at 4 points or more, tramadol 50 mg was IV injected.
To compare the degree of orthostatic intolerance, the minimal sample size for logistic regression analysis was a minimum of 100 or a larger sample size 10 times the value of the independent variable plus 1 [7]. Since there are 11 independent variables, it was set as 120, and including a 50% possibility of failure, the sample size was calculated as 180 subjects. The research subjects were 175 patients from a total of 194, excluding 19 cases where patient controlled analgesia was removed or stopped (8 patients) and subjects refusing to participate in the investigation (11 patients) due to dizziness, nausea, vomiting, headache and hypotention before postoperative first ambulation.
The degree of dizziness, nausea, vomiting, blurred vision, headache, drowsiness, and syncope at first ambulation after surgery was measured by yes or no, and if any of the above 7 symptoms occurred, it was defined as orthostatic intolerance. The total amount of opioid analgesia used included the amount of fentanyl administered in the recovery room and the amount of opioid analgesia administered through the patient controlled analgesia.
Data analysis was performed with the SPSS 12.0 program. General characteristics were analyzed with frequency, percentage, mean, and standard deviation. The difference in general and clinical characteristics between groups with and without symptoms of orthostatic intolerance was compared with the χ2 test and t-test. A logistic regression analysis using the forward selection method was performed to identify the factors affecting the occurrence of orthostatic intolerance. Here, the input level for the independent variables was 0.05 and the removal level 0.10, and the cross ratio for each factor and 95% confidence interval and accuracy of the classification were obtained.
Go to : 
RESULTS
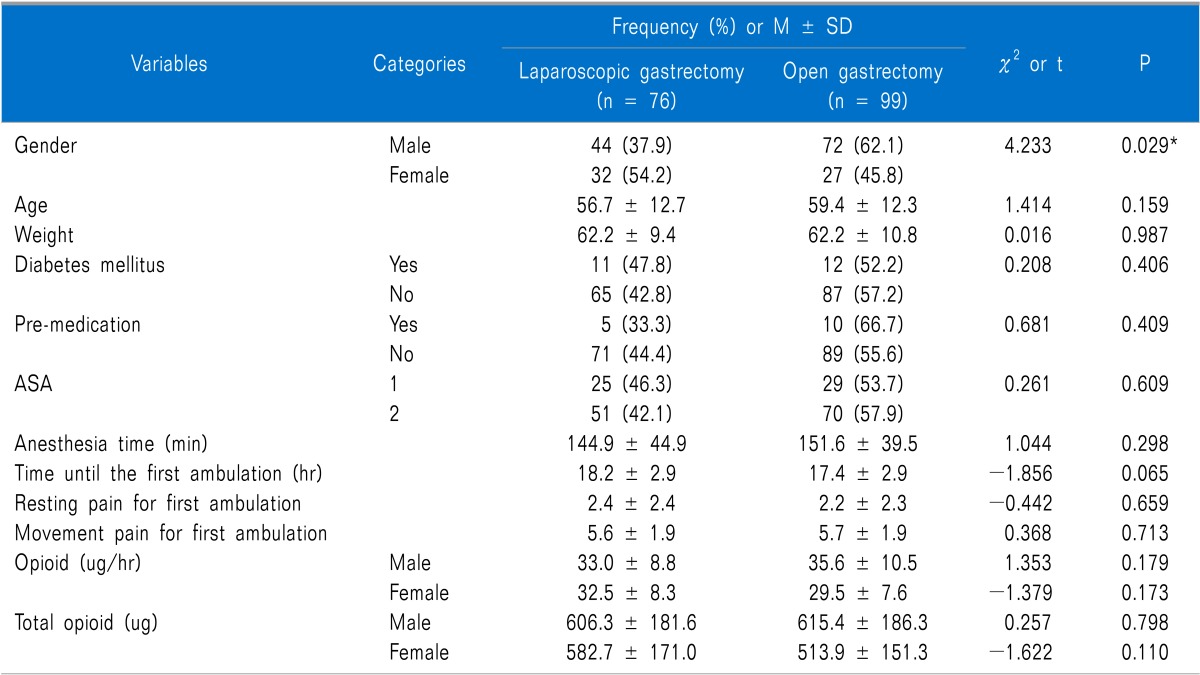
The general characteristics of all the subjects who received a gastrectomy were as follows. One hundred sixteen subjects were male (66.3%) and 59 subjects were female (33.7%). The mean age and weight were 58.2 ± 12.6 and 62.2 ± 10.2 kg, respectively. The anesthesia time was 148.7 ± 42.0 minutes, and 76 patients had laparoscopic surgery (43.4%) while 99 patients had open surgery (56.6%). The time until first ambulation after surgery was 17.8 ± 2.9 hours; resting pain immediately before first ambulation was 2.4 ± 2.4 points, and movement pain at first early ambulation was 5.7 ± 1.9 points. From the recovery room to first ambulation, the total administered drug dose was 591.5 ± 179.4 ug; a mean dose of 33.4 ± 9.5 ug was administered per hour (Table 1).
The comparison results of the differences in the general and clinical characteristics of the group who developed symptoms of orthostatic intolerance and the group who did not are as follows. The orthostatic intolerance symptoms group was 52.6% (61 patients) in male patients, and 74.6% (44 patients) in female patients. For the amount of drug used by patient controlled analgesia per hour in male patients, the group with orthostatic intolerance symptoms (OISs) significantly used more drug (36.5 ± 10.8 ug/hr) than the group without OISs (32.4 ± 8.4 ug/hr) (t = -2.234, P = 0.027). There were no significant differences in age, history of diabetes, premedication, ASA, anesthesia time, use of laparoscope, time from end of surgery to first early ambulation, resting pain at first early ambulation, movement pain, amount of drug used by patient controlled analgesia per hour in female patients, and total amount of drug used in both male and female (Table 1).
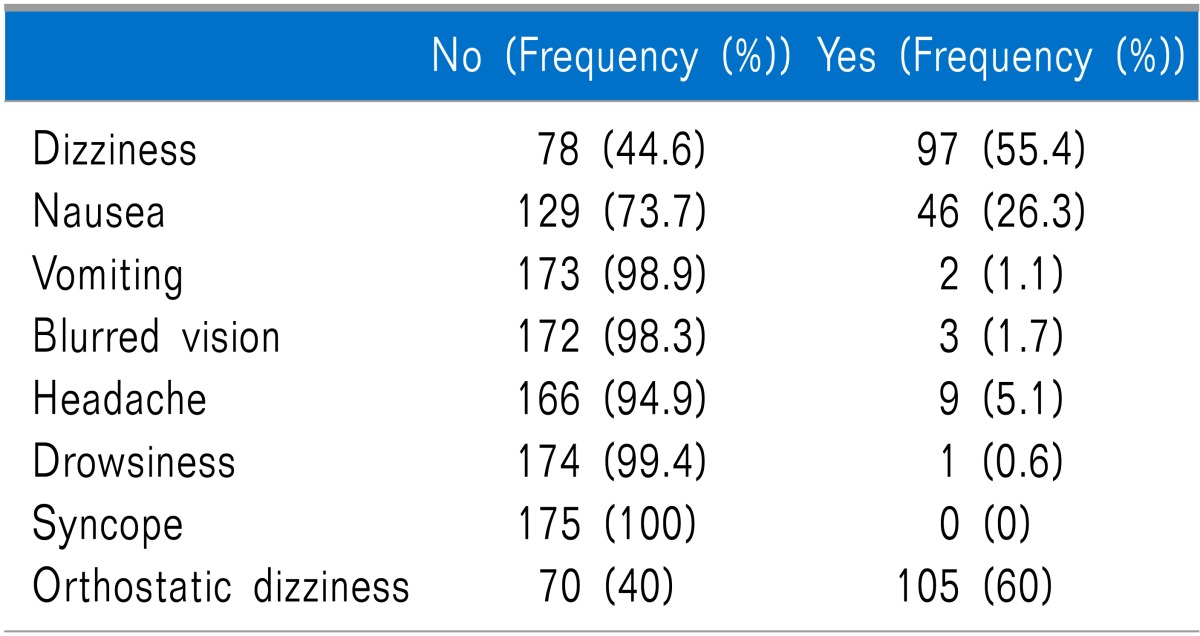
The orthostatic intolerance symptoms (OISs) presented by the patients were as follows. Dizziness and nausea occurred in 97 (55.4%), and 46 patients (26.3%), respectively. Vomiting and blurred vision presented in 2 (1.1%) and 3 patients (1.7%), respectively. Nine patients (5.1%) complained of headache; drowsiness appeared in 1 patient (0.6%), and no atients showed syncope. For the seven symptoms, some of them appeared exclusively and some together, and the group with OISshad105 patients (60%) and group without had 70 patients (40%) (Table 2).
The comparison results of the differences in the general and clinical characteristics between the group who underwent laparoscopic surgery and the group who underwent open surgery are as follows (Table 3). Females received laparoscopy (32 patients, 54.2%) more than open surgery (27 patients, 45.8%), while males received open surgery (72 patients, 62.1%) more than laparoscopy (44 patients, 37.9%) (X2 = 4.233, P = 0.029). There were no significant differences in age, history of diabetes, premedication, ASA, anesthesia time, time from end of surgery to first early ambulation, resting pain at first early ambulation, movement pain, amount of drug used by patient controlled analgesia per hour, and total amount of drug used between the laparoscopy group and open surgery group (Table 3).
Within subjects who underwent laparoscopic gastrectomy, the comparison results of the differences in the general and clinical characteristics between the group with OISs and group without were as follows. The orthostatic intolerance symptoms group was 56.8% (25 patients) in male patients, and 75.0% (24 patients) in female patients. There were no significant differences in age, history of diabetes, premedication, ASA, anesthesia time, time from end of surgery to first early ambulation, resting pain at first early ambulation, movement pain, amount of drug used by patient controlled analgesia per hour, and total amount of drug used (Table 4).
Within subjects who underwent open gastrectomy, the comparison results of the differences in the general and clinical characteristics between the group with OISs and group without were as follows. The orthostatic intolerance symptoms group was 74.1% (20 patients) in female patients. The frequency of male patients with OISs (36 patients, 50.0%) was the same without OISs (36 patients, 50.0%). For the amount of drug used by patient controlled analgesia per hour in male patients, the group with OISs significantly used more drug (38.6 ± 11.5 ug/hr) than the group without OISs (32.5 ± 8.5 ug/hr) (t = -2.558, P = 0.013). Total amount of drug used in female patients, the group with OISs significantly used more drug (549.3 ± 153.7 ug) than the group without OISs (412.7 ± 91.0 ug) (t = -2.203, P = 0.037). There were no significant differences in age, history of diabetes, premedication, ASA, anesthesia time, use of laparoscope, time from end of surgery to first early ambulation, resting pain at first early ambulation, movement pain, amount of drug used by patient controlled analgesia per hour in female patients, and total amount of drug used in male patients (Table 5).
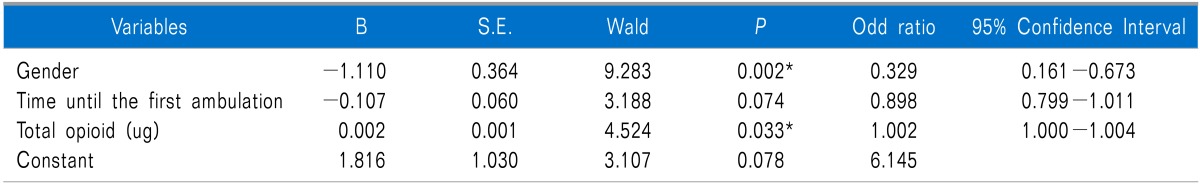
A logistic regression analysis was performed to identify the factors which affect the occurrence of OISs in all subjects who underwent gastrectomy, and it appears that sex (P = 0.002) and total amount of drug used (P = 0.033) were significant. When the occurrence of OISs in patients who used patient controlled analgesia was analyzed through odd's ratio, male patients appear to have a lower possibility of presenting symptoms compared to female patients (95% CI = 0.161-0.673), and the occurrence of symptoms was 1.002 times higher for a 1 ug increase in the total amount of drug used (95% CI = 1.000-1.004). The classification accuracy regarding the occurrence of OISs for the model was 63.4% (Table 6).
A logistic regression analysis was performed to identify the factors which affect the occurrence of OISs in subjects who underwent laparoscopic gastrectomy, and it appears that all variables were not significant (Table 7).
A logistic regression analysis was performed to identify the factors which affect the occurrence of OISs in subjects who underwent open gastrectomy, and sex (P = 0.008) and total amount of drug used (P = 0.015) appear to be significant. When the occurrence of OISs in patients who use patient controlled analgesia was analyzed through the odd's ratio, male patients appear to have a lower possibility of presenting with symptoms compared to female patients (95% CI = 0.084-0.690), and the occurrence of symptoms was 1.003 times higher for a 1 ug increase in the total amount of drug used (95% CI = 1.000-1.006). The classification accuracy regarding the occurrence of OISs for the model was 65.7% (Table 8).
Go to : 
DISCUSSION
This study was an investigative study identifying factors for orthostatic intolerance in general gastrectomy patients using patient controlled analgesia and discussed the results.
In this study, from the orthostatic intolerance symptoms of surgery patients who used patient controlled analgesia, 97 patients showed dizziness (55.4%), which was more than the 46 patients with nausea (26.3%) and the 9 patients with headache (5.1%). Other studies were mainly done on the changes in blood pressure because orthostatic intolerance is symptoms appearing from orthostatic hypotension [1,6], or related to nausea and vomiting in surgery patients using patient controlled analgesia [8]. However, the symptom that most patients actually complained of and suffered from was dizziness; thus, it is evident that the development and provision of nursing intervention to reduce dizziness is a priority.
From the general characteristics, more female patients (74.6%) complained of orthostatic intolerance than male patients (52.6%). This partially agrees with research results which reported that the occurrence of nausea and vomiting was more than two times higher in females [9]. Therefore, before using the patient controlled analgesia, education regarding orthostatic intolerance should be included or intervention to reduce the intolerance should be used for female patients.
In this study, there was no difference in age between the group with OISs (57.4 ± 12.9) and group without (59.6 ± 11.8). This contrast the results in another study [10] which reported that dizziness significantly increased as age increased in patients aged (odd ratio 2.83 (1.46-5.58); P = 0.002). In our study, most of the subjects who underwent a gastrectomy were in their 60's or younger so it was difficult to compare with subjects older than 75 years of age. Hence, in the future, it is necessary to conduct further research with subjects grouped in different age distributions.
In most studies, diabetes in patients was expected to have an effect on orthostatic intolerance due to its cardiovascular influence; therefore, diabetic patients were excluded from the studies [1,6,11]. However, when planning our study, it was anticipated that many of the gastrectomy patients would be elderly and have secondary diseases such as diabetes or hypertension. Hence, it was included in the variables, and there were no differences between the group with OISs and group without; thus, it was confirmed that diabetes did not apply as a reciprocal variable.
Regarding ASA classification, patients of grade 3 and 4 were excluded from our study, and when patients of grade 1 and 2 were compared for OISs, there were no statistically significant differences. This result partially agrees with research regarding orthostatic hypotension during continual injection of chest epidural bupivacaine-morphine in abdominal surgery patients [12], which reported that grade 1, 2, and 3 from the ASA classification had no correlation with orthostatic hypotension.
There were no differences in the group who developed orthostatic intolerance after laparoscopic surgery (64.5%) and the group who developed orthostatic intolerance after open surgery (56.6%). This result contrasts research which reported that the occurrence of postoperative nausea or vomiting increased 40-77% after laparoscopic surgery [13] and research which reported that in surgery patients using patient controlled analgesia, nausea and vomiting increased in laparoscopic surgery (43.5%) compared to open surgery (25.1%) [8]. Nausea and vomiting caused by laparoscopic surgery can occur immediately after surgery, but these results show that laparoscopy is not related to nausea and vomiting as symptoms of orthostatic intolerance during first ambulation.
From the factors which affected the occurrence of OISs in all subjects who underwent a gastrectomy, sex (P = 0.002) and total amount of drug used (P = 0.033) appear to be significant. For the total amount of drug used, the occurrence of OISs was 1.002 times higher for each 1 ug increase per hour (95% CI = 1.000-1.004). This result contrasts research conducted on hip arthroplasty patients [11], which reported that there were no differences in the total amount of drug used between the group who developed orthostatic intolerance and group who did not. In our study, opioid analgesic was continually administered as well as by the decision of the patient whenever there was pain through the patient controlled analgesia; thus, it showed a significant difference in the amount of drug used compared to the opioid analgesic prescribed according to pain in the precedent study. In addition, even without the patient having a sufficient understanding of pain expression, patients use it whenever they feel discomfort, so it is believed that the manifestation of OISs increased when the amount of opioid analgesic increased. Therefore, if patients have to continually use analgesics due to severe pain, performing a nursing intervention that has the patient gradually move to 30 degrees, 60 degrees, 90 degrees (sitting position) and a standing position rather than sudden movement should reduce the symptoms of orthostatic intolerance.
In conclusion, from the predictors of orthostatic intolerance symptoms at first ambulation of surgery patients who used patient controlled analgesia, total amount of drug used is a variable which can reduce the occurrence of orthostatic intolerance symptoms. Because decreasing the total amount of opioid drug, using other analgesics, and applying a nursing intervention may be helpful in reducing the occurrence of orthostatic intolerance symptoms, further research regarding this area is necessary.
Go to : 




 PDF
PDF Citation
Citation Print
Print







 XML Download
XML Download