This article has been
cited by other articles in ScienceCentral.
Abstract
There are various origins for chronic abdominal pain. About 10-30% of patients with chronic abdominal pain have abdominal wall pain. Unfortunately, abdominal wall pain is not thought to be the first origin of chronic abdominal pain; therefore, patients usually undergo extensive examinations, including diagnostic laparoscopic surgery. Entrapment of abdominal cutaneous nerves at the muscular foramen of the rectus abdominis is a rare cause of abdominal wall pain. If abdominal wall pain is considered in earlier stage of chronic abdominal pain, unnecessary invasive procedures are not required and patients will reach symptom free condition as soon as the diagnosis is made. Here, we report a case of successful treatment of a patient with abdominal cutaneous nerve entrapment syndrome by ultrasound guided injection therapy.
Go to :

Keywords: abdominal pain, abdominal wall, nerve compression syndromes, ultrasonography
Chronic abdominal pain has various origins. When patients are presented with chronic abdominal pain, physicians usually focus on the internal organs using extensive imaging techniques, laboratory exams, and sometimes even invasive procedures, including surgeries. Even when the examinations have no specific abnormal findings in the internal organs, physicians try to treat their patients with gastrointestinal tract medications empirically. However, in chronic abdominal pain, about 10-30% of patients have chronic abdominal wall pain [
1,
2]. Abdominal wall pains are known to be caused by myofascial pain, thoracic radiculopathy, nerve entrapments, referred pain of abdominal or thoracic viscera and so on [
3]. Among those, abdominal cutaneous nerve entrapment syndrome is a pain syndrome, which is thought to be the result of entrapment of cutaneous branches of an intercostal nerve at the level of the rectus abdominal muscle [
4].
The etiology of the syndrome is still obscure. Although there has been a few literature of abdominal cutaneous nerve entrapment syndrome, most of the previous reports described of blind injection techniques [
5]. Moreover, Recently, ultrasound guided injection for pain management is carried out more frequently due to its accuracy and efficacy. Here, we report a case of successful treatment of a patient with abdominal cutaneous nerve entrapment syndrome by an ultrasound guided injection.
CASE REPORT
A 31-year-old man visited our clinic with chronic abdominal pain that persisted for approximately one year. He was 170 centimeters tall, and his body weight was 53 kilograms. He was a car mechanic, and had no specific medical history or trauma history. At first, the pain started after taking a late-night snack. It was described as being severe squeezing in nature, which located on the right side of the periumbilical area that had persisted all day long. He did not have history of any sports activities. The pain intensity in visual analogue scale (VAS) was about 60-70 of 100. He had been on medication for gastrointestinal tract with nonsteroidal anti inflammatory drugs (NSAIDs) at the other hospital for over two months. The medication had no effect at all. For further evaluation, abdominal ultrasonography, abdominal computed tomography (CT), contrast media study of small and large intestine, endoscopy, and colonoscopy were done. Laboratory tests and simple x-rays of chest, abdomen, and lumbar spine were also performed. The examinations showed no specific abnormal findings. The patient was examined in supine position, and the site of maximum tenderness was identified; then he was asked to fold his arms across the upper chest, and to sit half way up. He complained greater tenderness with continuous local palpation, which is called Carnett test positive. It implies that the pain originated from the abdominal wall [
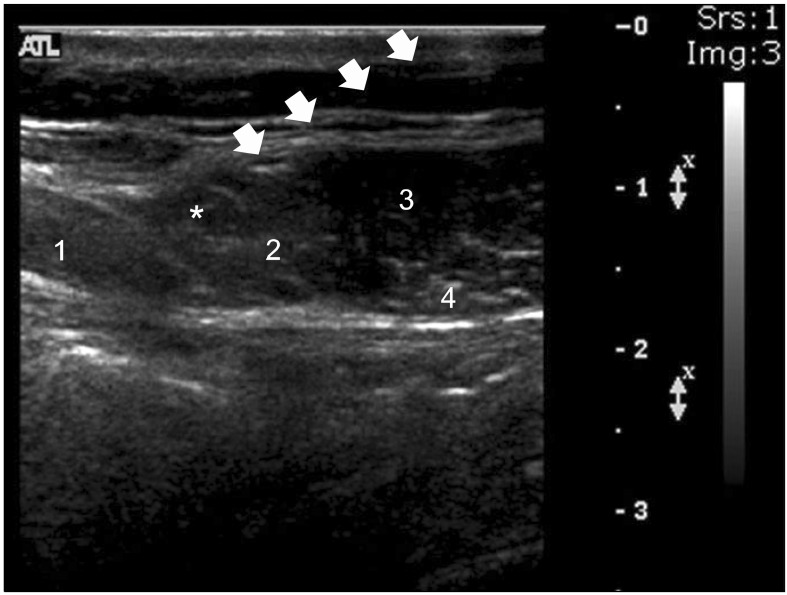
6]. For both diagnostic and therapeutic purpose, we decided to make an injection of local anesthetics at the area of rectus muscle where the entrapment of cutaneous nerve could occur. The patient was placed in supine position. We conducted Carnett test again to find the maximal tender point. The transducer (Linear probe 12-5 Hz, HDI 5000, Philips, USA) was positioned in the midline first, to get a short axis view (anatomic transverse view) so that the medial border of the rectus muscle and the linea alba are visulized. Then the transducer moved laterally to get a view of the lateral end of the rectus muscle and the linea semilunaris (
Fig. 1). The abdominal cutaneous nerve generally exists between the rectus abdominis and linea semilunaris, approximately 0.5-1.0 cm medial to linea semilunaris. Using the transverse scan, 25G 38 mm needle (BD Precision Glide™ Needle, Becton Dickinson Medical, Singapore) was advanced with the short axis in plane technique to reach the target area (
Fig. 2). We injected 10 ml of 1% of mepivacaine with 10 mg of triamcinolone. The pain intensity in VAS decreased to 30 of 100 with a single injection. With one week of interval, booster injection was done. After the second injection, the pain intensity in VAS decreased to 0-10 of 100. He remained symptom free for 10 months.
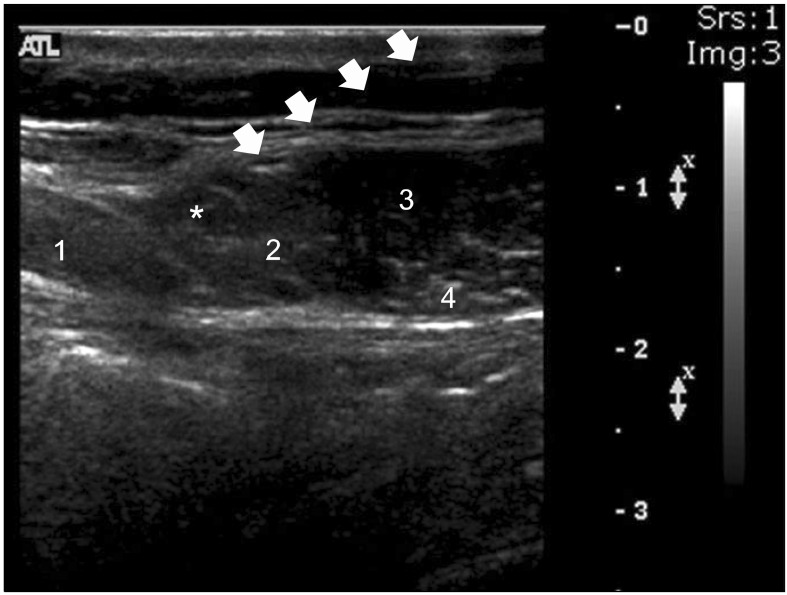
 | Fig. 1Placement of ultrasound transducer and needle over the lateral end of the rectus abdominis muscle. 
|
 | Fig. 2Ultrasound guided block of the abdominal cuateneous nerve, using the transverse scan of rectus abdominis muscle. Under the ultrasound guidance (12-5 Hz linear probe), the needle was advanced with the short axis in plane technique to reach the target area. 1: Rectus abdominis, 2: Linea semilunaris, 3: Internal oblique, 4: Transversus abdominis, *: Abdominal cutaneous nerve, White arrows are marked tracing needle trajectory. 
|
Go to :

DISCUSSION
Abdominal cutaneous nerve entrapment syndrome is a rare condition in chronic abdominal pain. The most common cause of the syndrome is nerve entrapment at the lateral border of the rectus abdominis muscle. When a patient is seen for abdominal pain without other clinically significant symptoms, the syndrome should be high on the list of likely diagnoses. In this case, we made both diagnosis and treatment together using ultrasound in a young male-patient, who had chronic abdominal pain for one year without any reliable triggering factor.
Abdominal cutaneous nerve entrapment syndrome is first described by Applegate in 1972 [
7]. In patients with chronic abdominal pain, abdominal wall is not usually considered as a cause of pain. However, Hall and Lee [
8] have previously reported that about 15% of persistent chronic non-specific abdominal pain can be originated from the abdominal wall. Abdominal cutaneous nerve entrapment syndrome is considered as a neuropathy of cutaneous branches of the 7-12
th intercostal nerves [
4]. When the cutaneous branches go through the rectus abdominis, entrapment in the muscular foramen can occur, which will lead to ischemia of the nerve branches causing ischemic neuropathy. In previous reports, abdominal trauma, surgery, and pregnancy are thought to develop abdominal cutaneous nerve entrapment syndrome [
9-
11]. However, in this case, the patient had no such conditions and the syndrome occurred spontaneously.
Diagnostic criteria of abdominal cutaneous entrapment syndrome are as follows; 1) the pain can be developed by physical examination or position change, 2) no specific abnormal results in other examinations, 3) reproducible pain with pinching on the affected area, which called positive pinch test, and 4) dramatic improvement of the pain with local anesthetics [
12]. Above these, Carnett test can be done to see if the pain is originated from the abdominal wall [
13]. In this case, the patient satisfied the above described criteria and showed a positive Carnett test.
Here, we carried out an ultrasound guided injection and it has several benefits compared to blind procedures. First, blind injections need experienced techniques to infiltrate the exact site. Second, even with experts, when the injection is performed blindly, the positional variations of fascia and nerve between people cannot be properly considered, which will result in ineffectiveness of treatment. Third, ultrasound guidance can make an actual confirmation of the drug go into the accurate site for injection, where the operator intended to. Fourth, ultrasound guidance can identify the depth and direction of the inserted needle tip; therefore, complications such as peritoneal penetrations and vascular injuries can be avoided [
4,
13,
14].
In conclusion, abdominal wall pain, such as abdominal cutaneous entrapment syndrome, should be considered when there is no other diagnostic finding. If abdominal wall pain is considered in earlier stage of chronic abdominal pain, unnecessary examinations and invasive procedures, such as diagnostic laparoscopy, can be avoided, and the patient will not suffer from pain for a long time. Furthermore, ultrasound guided procedures are reliable, safe, and effective for both diagnosis and treatment.
Go to :






 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download