This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The pes anserine bursa lies beneath the pes anserine tendon, which is the insertional tendon of the sartorius, gracilis, and semitendinosus muscles on the medial side of the tibia, but it can lie in different sites in the medial knee. Accurate diagnosis of the position of the bursa is critical for diagnostic and therapeutic goals. The aim of this study was to evaluate sonoanatomic variations of the pes anserine bursa in the medial knee.
Methods
One hundred seventy asymptomatic volunteers were enrolled in this study. Using ultrasound imaging (transverse approach, 7-13 MHz linear array probe) the sonoanatomic position of the pes anserine bursa and its relation to the pes anserine tendon were evaluated. Additionally, we evaluated the sonoanatomic variation of the saphenous nerve.
Results
The position of the pes anserine bursa was between the medial collateral ligament and the pes anserine tendons in 21.2%/18.8% (males/females) of subjects; between the pes anserine tendons and the tibia in 67.1%/64.7% (m/f); and among the pes anserine tendons in 8.2%/12.9% (m/f). No significant differences in the position of the bursa existed between males and females. The saphenous nerve was found within the pes anserine tendons in 77.6%/74.1% (m/f) of subjects, but outside the pes anserine tendons in 18.8%/15.3% (m/f). Visibility of sonoanatomic structures was not related to either gender or BMI.
Conclusions
Ultrasound provides very accurate information about variations in the pes anserine bursa and the saphenous nerve. This suggests that our proposed ultrasound method can be a reliable guide to facilitate approaches to the medial knee for diagnostic and therapeutic objectives.
Go to :

Keywords: bursa, pes anserine, saphenous nerve, ultrasonography
INTRODUCTION
Knee problems are the cause for which a large number of patients are referred to pain clinics. Due to its nature of complex movements, the knee is extremely sensitive to anatomic and functional derangements which can result from even small changes such as arthritis or injury to cartilage or ligaments [
1]. Given that the knee has a complex structure, inflammation of one bursa can cause significant dysfunction, pain, and sometimes infection of the entire knee [
2].
Although in most cases, the pes anserine bursa lies beneath the pes anserine tendon, which is the insertional tendon of the sartorius, gracilis, and semitendinosus muscles on the medial side of the tibia, it can have other anatomic positions as well. Due to the unique anatomic connections in the medial part of the knee, it is often hard to detect the anatomic structure which is the cause of a patient's pain by clinical examination [
3]. Patients suffering from pes anserine bursitis experience pain in the medial part of the knee. Generally, it is difficult to diagnose pes anserine bursitis by physical examination. Use of common diagnostic modalities such as plain X-ray, MRI, and electromyography for the diagnosis of pes anserine bursitis is time-consuming, and injection into the bursa without image guidance is associated with considerable complications [
4,
5]. In recent years, the ultrasound technique has played a crucial role in increasing the accuracy and efficacy of neuraxial and peripheral nerve blockade as well as joint injection by both decreasing the rate of complications and improving our anatomic knowledge [
6-
8].
Therefore, this study was performed to evaluate sonographically the visibility and positions of the pes anserine bursa and its adjacent anatomic structures. In addition, the location of the saphenous nerve was also examined because it is in close vicinity to the pes anserine tendons of the medial part of the knee.
Go to :

MATERIALS AND METHODS
After approval of the study protocol by the Institutional Review Board, 170 asymptomatic volunteers between 15 and 80 years of age and of ASA class I or II were enrolled in this study after providing informed consent. Exclusion criteria were: volunteer's withdrawal at any time after the submission of informed consent, congenital or acquired structural malformation, localized infection, knee pain, history of knee surgery, and any type of knee injury.
Following preparation, the volunteers were placed in the supine position with the knee bent at a 5 to 10 degree angle and ultrasound imaging was performed on the medial part of the knee. The sonography device was MicroMaxx (SonoSite, Inc., USA), and we used a linear array probe with 6-13 MHz frequency, with penetration depths of 2.5, 3.1, or 4 cm according to the volunteer's body mass index (BMI). The sonographic study was performed by an expert physician on both knees of the volunteers. For ultrasound visibility, we set criteria as follows: invisible (cannot detect), poor (detection of tendons and saphenous nerve), moderate (detection of tendons, pes anserine bursa, and saphenous nerve), and well (detection of tendons, pes anserine bursa, saphenous nerve, and medial collateral ligament). To prevent bias, all ultrasound examinations were performed by one pain physician while image evaluation was performed by another pain physician.
The gathered data were recorded by the first physician on previously composed sheets including demographic data such as age, weight, height, BMI, and gender, while anatomic indicators regarding the pes anserine bursa and the saphenous nerve were recorded by the second physician. The data were statistically analyzed using SPSS software version 18. The chi-square test was used for comparison of the frequency of the bursa position.
Go to :

RESULTS
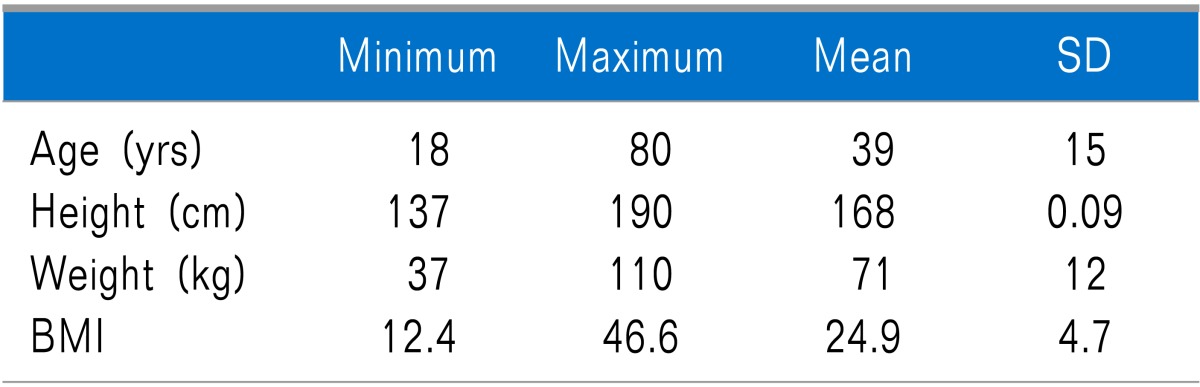
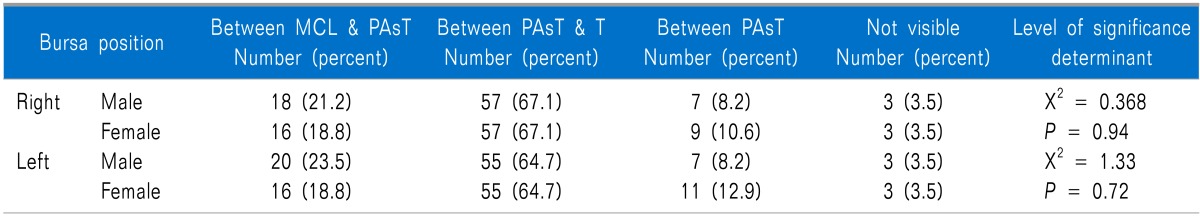
The demographic data is shown in
Table 1. No relationship was detected between BMI and sonographic visibility of the anatomic structures.
Table 1
Demographic Data of the Patients Studied for Sonoanatomic Variables of Pesanserine Bursa

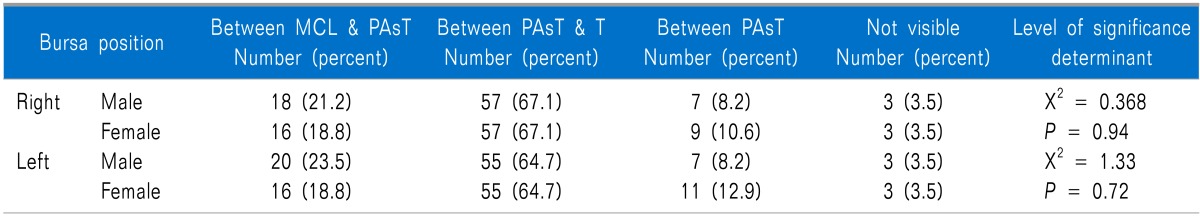
The position of the bursa in males was between the pes anserine tendons and the tibia in 67.1% of cases, between the medial collateral ligament and the pes anserine tendons in 21.2%, and between the pes anserine tendons in the right knee in 8.2%, and in some cases it was not visible. There were no significant differences between males and females in the position of the pes anserine bursa (
Table 2).
Table 2
Comparison of the Frequency of Pes Anserine Bursa According to Gender

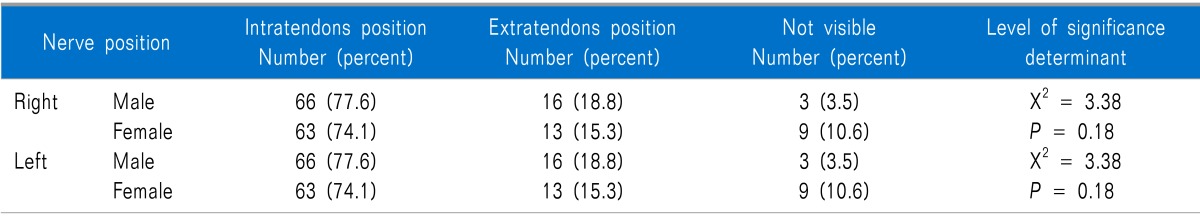
Comparison of the location of the saphenous nerve between males and females showed that the nerve lies between the pes anserine tendons (intratendinous position) in 77.6% of male and female volunteers and outside the pes anserine tendons (extratendinous position) in 18.8% of males and 15.3% of females (
P = 0.18), and in some cases it was not visible (
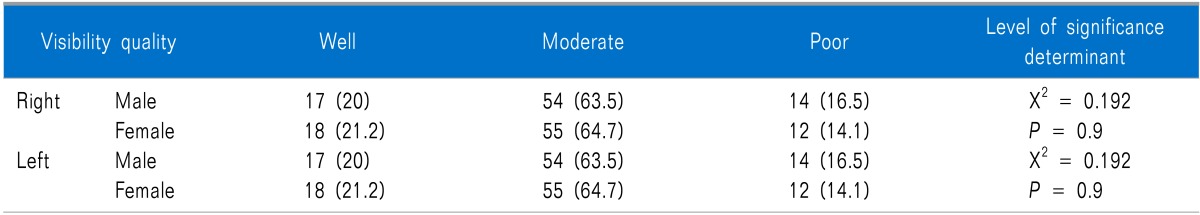
Table 3). No differences between males and females were observed in the frequency of visibility of sonoanatomic structures including the pes anserine tendons, the pes anserine bursa, and the saphenous nerve (
Table 4).
Table 3
Comparison of the Frequency of Saphenous Nerve According to Gender
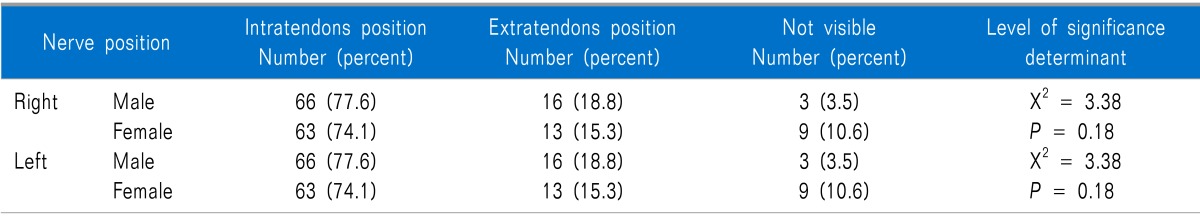

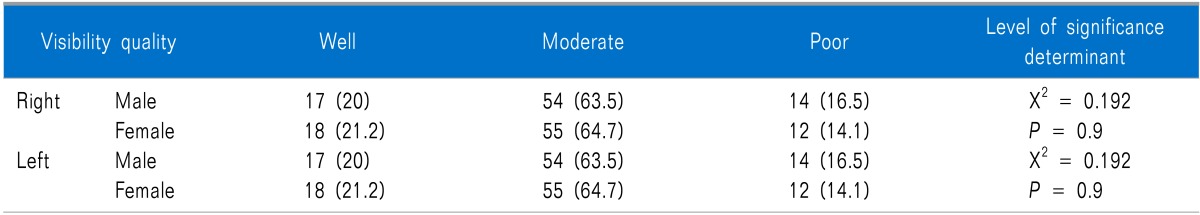
Table 4
Comparison of the Frequency of Visibility of Sonoanatomic Structures According to Gender

Out of 170 volunteers, one 40-year-old woman had pes anserine bursitis and felt moderate pain when the sonography probe was placed on the medial part of her left knee (
Fig. 1). On examination of the knee of one 38-year-old man, thickening of the pes anserine tendon was observed. The subject gave a history of mild pain upon walking down slopes (
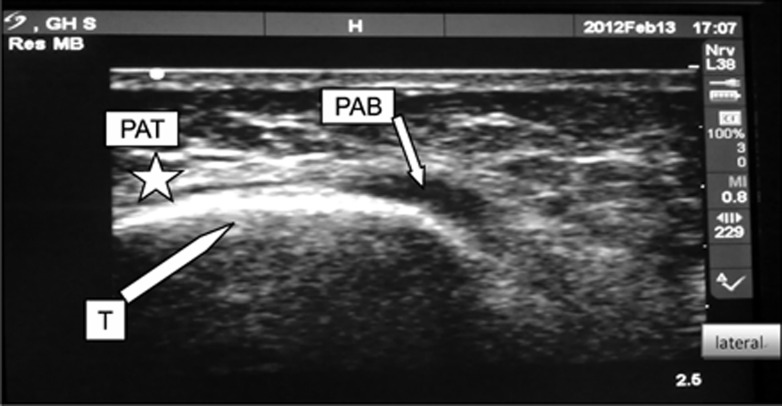
Fig. 2). Other sonoanatomic variations are shown in
Fig. 3-
6.
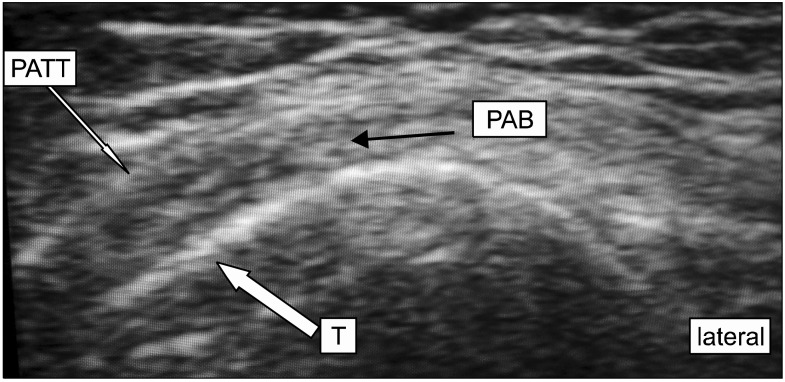
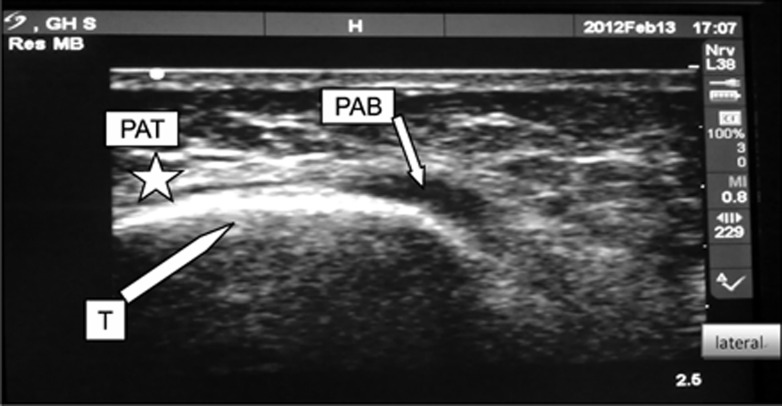 | Fig. 1Fluid filled pes anserine bursa (PAB) indicates the presence of bursitis. T: border of tibia, PAT: pes anserine tendons (asterisk). 
|
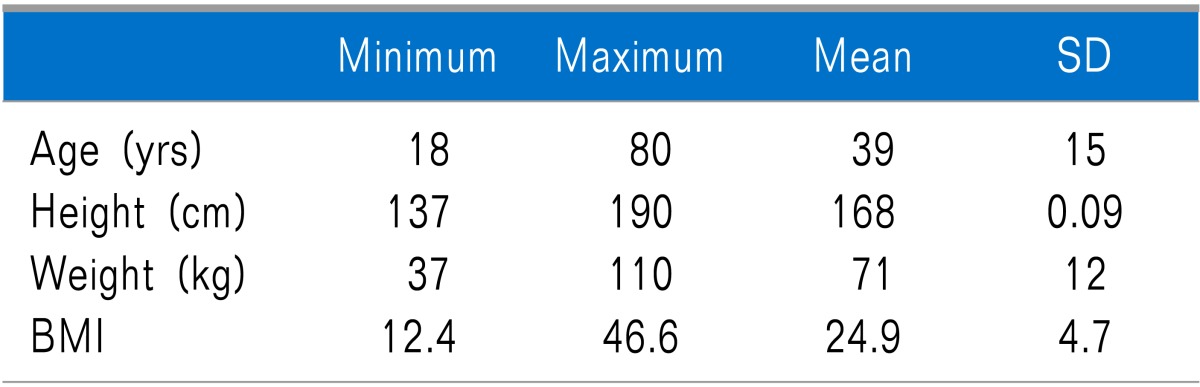
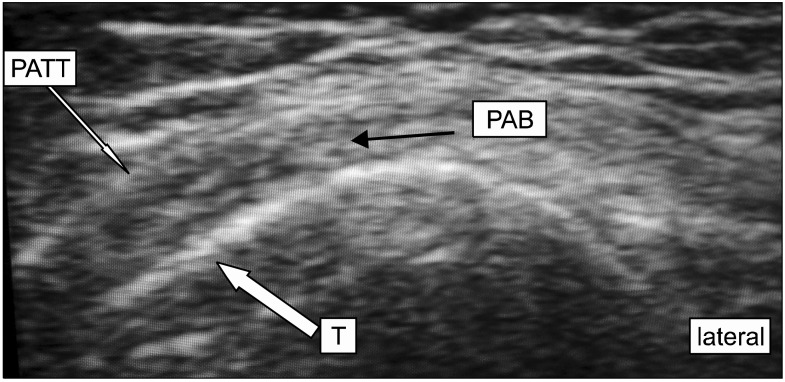 | Fig. 2Thickening of pes anserine tendons is shown. PATT: pes anserine tendon thickening, T: border of tibia, PAB: pes anserine bursa. 
|
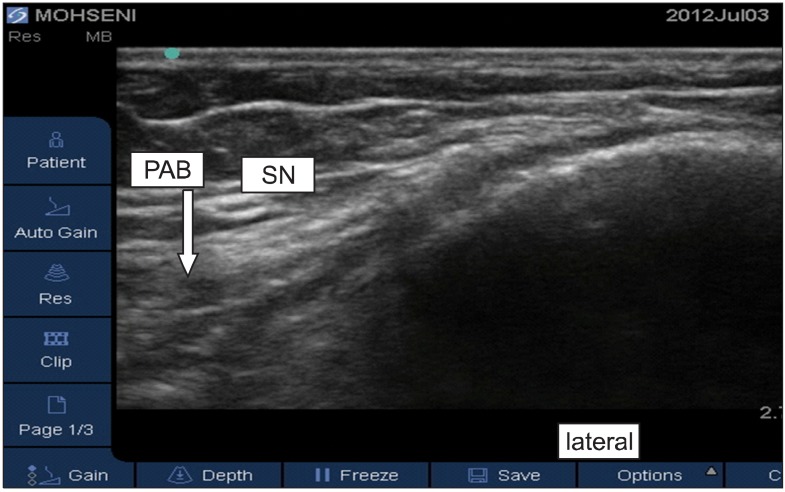
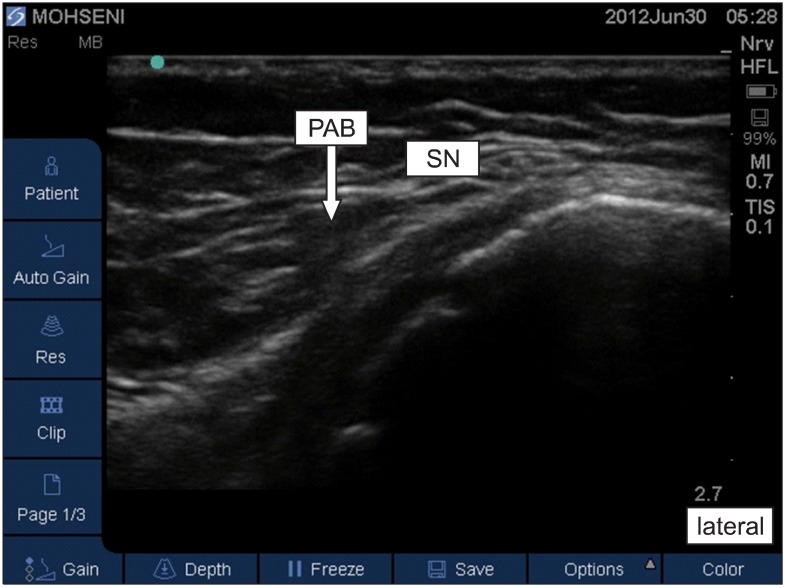
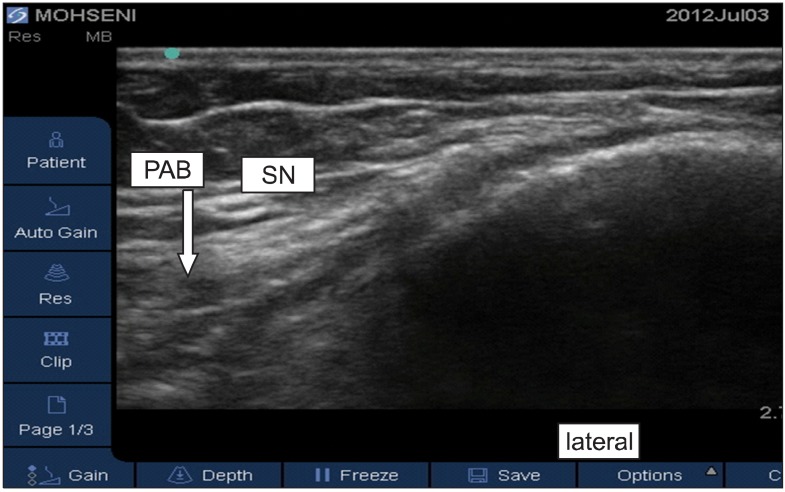 | Fig. 3Pes anserine bursa (PAB) is located between the pes anserine tendons and tibia. SN: saphenous nerve. 
|
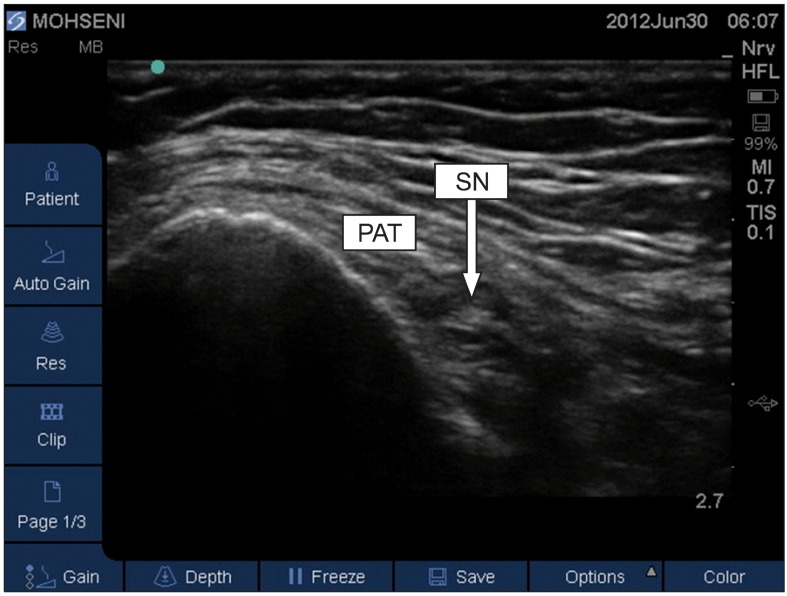
 | Fig. 6Saphenous nerve is located outside of pes anserine tendons. PAT: pes anserine tendons, SN: saphenous nerve. 
|
Go to :

DISCUSSION
In clinical practice, bursitis is one of the most common causes of knee pain [
9]. Knee bursae including the pes anserine bursa are prone to injuries from both acute traumas and continuous micro traumas [
10,
11]. The pes anserine bursa has been described by most sources to lie beneath the pes anserine tendon, which is the insertional tendon of the sartorius, gracilis, and semitendinosus muscles on the medial side of the tibia, but it can lie between the pes anserine tendons and the medial collateral ligament of the knee [
12].
Pain from inflammation of the pes anserine bursa worsens with passive internal rotation and active external rotation of the knee. Activity, especially external rotation and flexion of the knee, aggravates the pain [
13]. Therefore, it can be mistaken for delicate pressure fractures, degenerative joint disease, meniscus injury, medial collateral ligament injury, non-specific medial meniscus cysts, paratibial cysts, semimembranosus bursitis, pes anserine tendonitis, and entrapment of the saphenous nerve [
14]. Although magnetic resonance imaging is helpful in ruling out problems such as tumors and other injuries, it is not a cost-effective modality for diagnostic injection into the pes anserine bursa [
15].
According to the study of Finnoff et al. [
16], blind injection into the pes anserine bursa has a high failure rate. In that study, the accuracy of ultrasound for correct injection into the pes anserine bursa was 92% (correct injections 11 out of 12), while only 17% of injections performed without ultrasound guidance correctly entered the bursa (correct injections 2 out of 12). In addition, a case of pes anserine tendonitis diagnosed by sonography in a 45-year-old woman who presented to the emergency room with acute severe pain in the medial part of her knee was also reported [
17].
In recent years, the ultrasound technique has played a crucial role in increasing the accuracy of peripheral nerve blockades, knee joint injections, and diagnosis of rheumatologic diseases [
18-
20]. Considering the prevalence of knee pain and the importance of diagnostic injections for pes anserine bursitis, as well as the results of this study, which demonstrated that demographic characteristics such as age, gender, and BMI do not influence the visibility of sonoanatomic structures, ultrasound can be considered an effective modality in diagnostic and therapeutic injection in the pes anserine bursa.
In the present study, although the pes anserine bursa lies in its usual position, which is between the tibia and the pes anserine tendons, in 67.1% of subjects, it is also found between the pes anserine tendons and the medial collateral ligament in 21.2%, and between the tendons of the sartorius, gracilis, and semitendinosus in 8.2%. This anatomic variation may lead to incorrect injections inside the tendon while attempting blind injection into the bursa. Information on the variation in location of the bursa and tendons is mandatory in performing injection therapy because correct injection into an inflamed bursa can help to reduce inflammation, but an inaccurate injection into a tendon may lead to tendon weakness and atrophy and higher risk of tendon rupture. On the other hand, entrapment of the saphenous nerve in the medial part of the knee is an important consideration in the differential diagnosis of pes anserine bursitis [
21,
22]. According to the results of this study, which reported the position of the saphenous nerve as intratendinous in 77.6% of cases and extratendinous in 18.8% of cases, we would assume that sonography can be used to find and block the saphenous nerve either for local surgical procedures or for treating nerve entrapment.
Finally, based on the results of this study, as a domestic survey on the target patients, and considering the evidence provided by previous studies reporting the accuracy of sonography in finding the position of the pes anserine bursa, ultrasonography can be used as a valuable and rapid method to assist in diagnostic and therapeutic procedures on the medial part of the knee. However, utilization of ultrasound for chronic pain interventions is still in its relatively early stages, and additional studies are required to further evaluate the efficacy and limitations of employing this modality [
23].
Go to :

ACKNOWLEDGEMENTS
The researchers wish to offer their sincere thanks to those colleagues who provided invaluable advice on statistical analysis.
The authors did not receive any external funding or grants in support of their research for or preparation of this work.
Go to :

References
1. Shrive NG, O'Connor JJ, Goodfellow JW. Load-bearing in the knee joint. Clin Orthop Relat Res. 1978; (131):279–287. PMID:
657636.

2. Jensen LK, Eenberg W. Occupation as a risk factor for knee disorders. Scand J Work Environ Health. 1996; 22:165–175. PMID:
8837261.

3. Mochizuki T, Akita K, Muneta T, Sato T. Pes anserinus: layered supportive structure on the medial side of the knee. Clin Anat. 2004; 17:50–54. PMID:
14695588.

4. Alvarez-Nemegyei J. Risk factors for pes anserinus tendinitis/bursitis syndrome: a case control study. J Clin Rheumatol. 2007; 13:63–65. PMID:
17414530.
5. Chatra PS. Bursae around the knee joints. Indian J Radiol Imaging. 2012; 22:27–30. PMID:
22623812.

6. Kil HK, Cho JE, Kim WO, Koo BN, Han SW, Kim JY. Prepuncture ultrasound-measured distance: an accurate reflection of epidural depth in infants and small children. Reg Anesth Pain Med. 2007; 32:102–106. PMID:
17350519.

7. Wisniewski SJ, Smith J, Patterson DG, Carmichael SW, Pawlina W. Ultrasound-guided versus nonguided tibiotalar joint and sinus tarsi injections: a cadaveric study. PM R. 2010; 2:277–281. PMID:
20430329.

8. Reach JS, Easley ME, Chuckpaiwong B, Nunley JA 2nd. Accuracy of ultrasound guided injections in the foot and ankle. Foot Ankle Int. 2009; 30:239–242. PMID:
19321101.

9. Aaron DL, Patel A, Kayiaros S, Calfee R. Four common types of bursitis: diagnosis and management. J Am Acad Orthop Surg. 2011; 19:359–367. PMID:
21628647.

10. Calmbach WL, Hutchens M. Evaluation of patients presenting with knee pain: part II. Differential diagnosis. Am Fam Physician. 2003; 68:917–922. PMID:
13678140.
11. Forbes JR, Helms CA, Janzen DL. Acute pes anserine bursitis: MR imaging. Radiology. 1995; 194:525–527. PMID:
7824735.

12. De Maeseneer M, Vanderdood K, Marcelis S, Shabana W, Osteaux M. Sonography of the medial and lateral tendons and ligaments of the knee: the use of bony landmarks as an easy method for identification. AJR Am J Roentgenol. 2002; 178:1437–1444. PMID:
12034613.

13. Butcher JD, Salzman KL, Lillegard WA. Lower extremity bursitis. Am Fam Physician. 1996; 53:2317–2324. PMID:
8638508.
14. Rennie WJ, Saifuddin A. Pes anserine bursitis: incidence in symptomatic knees and clinical presentation. Skeletal Radiol. 2005; 34:395–398. PMID:
15940489.

15. Grover RP, Rakhra KS. Pes anserine bursitis - an extra-articular manifestation of gout. Bull NYU Hosp Jt Dis. 2010; 68:46–50. PMID:
20345364.
16. Finnoff JT, Nutz DJ, Henning PT, Hollman JH, Smith J. Accuracy of ultrasound-guided versus unguided pes anserinus bursa injections. PM R. 2010; 2:732–739. PMID:
20598959.

17. Valley VT, Shermer CD. Use of musculoskeletal ultrasonography in the diagnosis of pes anserine tendinitis: a case report. J Emerg Med. 2001; 20:43–45. PMID:
11165837.

18. Curtiss HM, Finnoff JT, Peck E, Hollman J, Muir J, Smith J. Accuracy of ultrasound-guided and palpation-guided knee injections by an experienced and less-experienced injector using a superolateral approach: a cadaveric study. PM R. 2011; 3:507–515. PMID:
21665162.

19. Gilliland CA, Salazar LD, Borchers JR. Ultrasound versus anatomic guidance for intra-articular and periarticular injection: a systematic review. Phys Sportsmed. 2011; 39:121–131. PMID:
22030948.

20. Epis O, Iagnocco A, Meenagh G, Riente L, Delle Sedie A, Filippucci E, et al. Ultrasound imaging for the rheumatologist. XVI. Ultrasound-guided procedures. Clin Exp Rheumatol. 2008; 26:515–518. PMID:
18799078.
21. Hemler DE, Ward WK, Karstetter KW, Bryant PM. Saphenous nerve entrapment caused by pes anserine bursitis mimicking stress fracture of the tibia. Arch Phys Med Rehabil. 1991; 72:336–337. PMID:
2009053.
22. Morganti CM, McFarland EG, Cosgarea AJ. Saphenous neuritis: a poorly understood cause of medial knee pain. J Am Acad Orthop Surg. 2002; 10:130–137. PMID:
11929207.

23. Soneji N, Peng PW. Ultrasound-guided pain interventions - a review of techniques for peripheral nerves. Korean J Pain. 2013; 26:111–124. PMID:
23614071.

Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download