INTRODUCTION
Since BC 400 when Hippocrates used temperature in a diagnosis by applying mud to a patient's body and speculating that dry areas had disease, temperature has been an important area of interest in medicine. The skin is a very important organ in temperature regulation, and body temperature is controlled by the combined control of the central and autonomic nerve system. Infrared thermography (IRT) detects infrared light emitted by the body to visualize changes in body heat due to abnormalities in the surface blood flow of diseased areas. IRT is not a tool that shows anatomical abnormalities, but is a method that shows physiological changes. It objectively visualizes subjective symptoms, therefore, it is useful in making diagnoses and doing evaluations in the field of pain medicine where a diagnosis is based on subjective complaints of symptoms. The advantages of IRT is that ① it is non-invasive and painless, ② it is not harmful to the patient, ③ it is possible to conduct tests in a physiologically natural state, and ④ its testing time is short. The aim of this paper is to introduce the basic mechanism of IRT, significance in interpretation, and clinical utilization.
Go to : 
BASIC MECHANISM
The most important theoretical background of IRT is that the distribution of body heat in a normal body is symmetrical [1]. Therefore, the symmetry of body heat is considered to be the most important element when interpreting IRT images. An infrared camera is used to measure infrared light emitted from the body and displays this on the screen, and pseudocolor mapping is done on the obtained infrared image to facilitate visual interpretation [2]. Therefore, when comparing the distribution of body heat on both sides of the body, the region of interest (ROI) is set to an equal size on each side of the obtained pseudocolor image, and the mean temperature within each ROI is calculated to compare the difference. There are two methods to compare the temperature difference within an ROI of the affected and unaffected sides. The first method is to define a significant difference such as when the asymmetry of temperature deviates from 1-standard deviation of the unaffected side ROI [3], and second is to define the significance such as when the difference in mean temperature of both ROIs is more than the 'reference temperature difference'. The latter method is mainly used in the clinical field.
Go to : 
UTILIZATION OF IRT IN PAIN MEDICINE
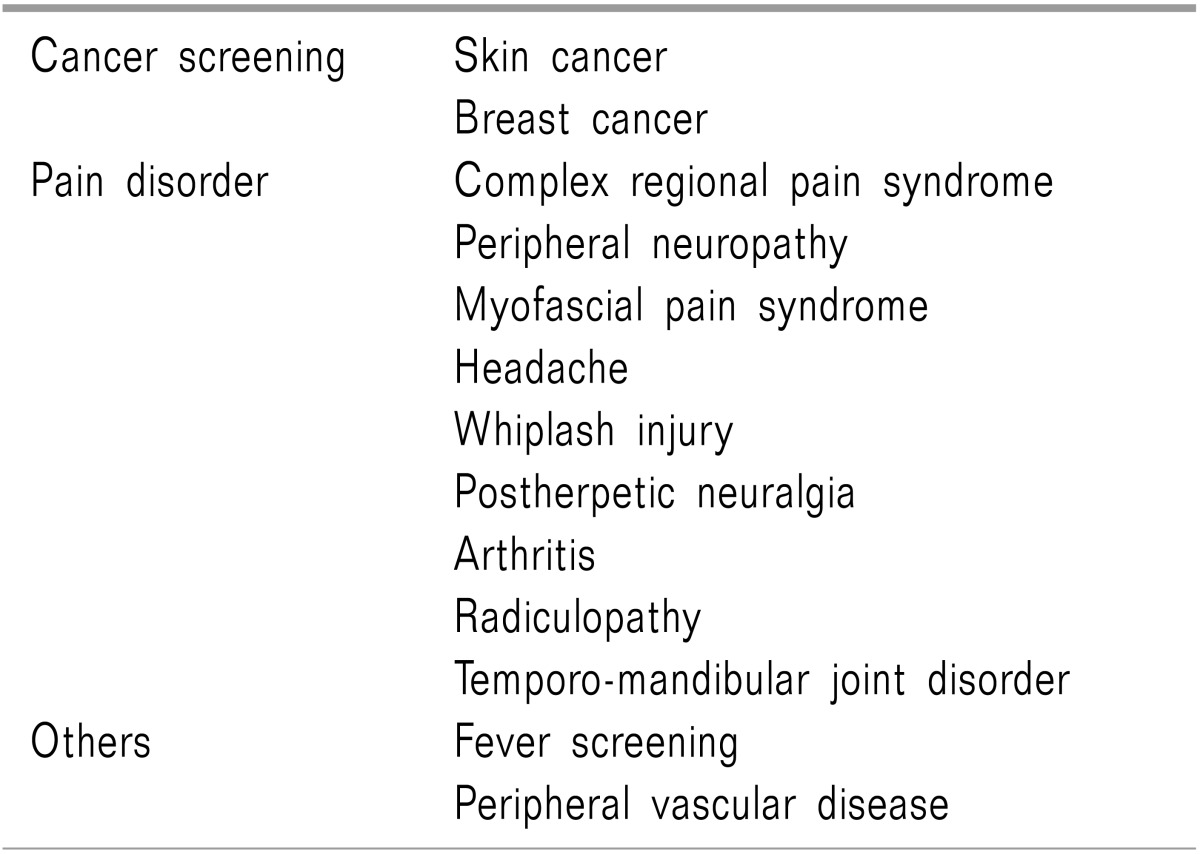
After Galileo designed the first thermometer in 1592, infrared light was discovered by William Herschel in 1800, and the first diagnostic IRT was used in diagnosis of breast cancer by Lawson in 1956 [4]. Then, in 1982, the US Food and Drug Administration approved IRT as an adjunctive screening tool of breast cancer, and up to now, there have been many studies regarding the usefulness of IRT in various areas such as complex regional pain syndrome (CRPS) [5-7], postherpetic neuralgia [8], whiplash injury [9,10], inflammatory arthritis [11,12], temporo-mandibular joint disorder [13,14], headache [15,16], and myofascial pain syndrome [17,18]. The diseases where IRT can be used are presented in Table 1. Considering that IRT visualizes physiological and functional abnormalities rather than anatomical abnormalities, there is no doubt that compared to other imaging diagnostic methods, IRT is an effective diagnostic method for diseases difficult to diagnose with CT or MRI, such as CRPS, neuropathic pain, headache, and myofascial pain. In fact, for CRPS, it is known to have higher sensitivity compared to MRI or three phase bone scan [5,19], and it is reported that thermography has higher sensitivity in diagnosis of neuropathic pain compared to the sympathetic skin response test [20]. When deciding an abnormality in specific diseases, there are different views on what the 'reference temperature difference' should be according to researcher, and for CRPS, standards such as 0.6℃ [21] and 1.0℃ [22] are used. Meanwhile, regarding the reliability of IRT, research has been conducted for CRPS [7] and myofascial pain syndrome [17,23], and it was reported that there is high reliability for these diseases. In terms of correlation between pain and temperature difference measured with IRT, it was reported that there was a significant correlation between the severity of pain caused by lumbar disc herniation with the difference in skin temperature [24]. It was also reported that there was a significant correlation between the pressure pain threshold and the temperature difference in myofascial pain syndrome [18]. Recently, the technique, which obtains a dynamic image using a stress loading test as well as static IRT, is widely used. The theoretical basis for this is that normally the temperature change on both sides of the body after stress loading is symmetrical, and the degree of temperature restoration after removing the stress is symmetrical on both sides. Therefore, when restoration of temperature is asymmetrical after removal of stress, it is considered that physiological abnormalities exist. For the stress loading test, cold/warm stress, exercise, pharmacological stress, vibration, and visual stimulation are used as stress, and from these, the cold stress test is used the most. When using cold stress thermography, it is known that sensitivity and specificity is enhanced for diagnosis of CRPS [25-27], but it causes pain for the patient during the cold stress thermography, and a standardized guideline for the stress loading test has not been established.
Go to : 
POSSIBILITY OF ERROR IN COMPARING THE TEMPERATURE DIFFERENCE OF BOTH SIDES ACCORDING TO THE ROI SETTING
Currently there are no established standards for setting an appropriate ROI. The ROI is set as symmetrical on the pseudocolor image based on the discretion of the examiner taking into consideration the medical history and symptom area of the patient. Therefore, according to the size and shape of the ROI, the temperature difference on both sides can be calculated differently. In addition, the IRT equipment currently used only shows the mean temperature and standard deviation within the fixed ROI, and the actual interpretation of the IRT image only compares the mean temperature of the ROI without considering the size of the ROI. In principle, when comparing two means, statistical difference is determined by considering the mean, standard deviation, and sample size. Thus, when only the mean values are simply compared without considering all these items, there is the possibility of error based on statistical interpretation. Therefore, considering the number of pixels in the fixed ROI (reflecting sample size), and the mean and standard deviation of the temperature in interpreting results can reduce false positives and false negatives, and enable objective interpretation of the results. For this, an ROI of equal size symmetrical for both sides of the body is set, and the t-test can be used taking into consideration the mean temperature, standard deviation, and number of pixels in the ROI, or the pixels on each side can be matched 1:1 to conduct a paired t-test for the temperature difference in each matched pixel [28]. Based on personal opinion, it is difficult to satisfy the assumption that the left and right side of the body are independent; thus, using the paired t-test with matched pixels is thought to be a more valid method statistically. However, there is no testing equipment which provides this kind of function presently. Hence, it is anticipated that an IRT system will be developed to enable such statistical analysis in the future.
Go to : 
DEVELOPMENT OF IRT TECHNOLOGY
Recently, there has been much effort to improve the hardware and software of medical IRT. Developments have been achieved such as enhanced performance of the infrared sensor, improved image quality, real-time image processing, and a multi-channel system. As a result, it is possible to obtain precise images with a thermal resolution of 0.08℃ or lower and a special resolution of 1×1 mm or lower. A 3-dimensional image technique was also developed to show the body heat in a more detailed image compared to the existing 2-dimensional image [29]. In addition, recently a remote diagnosis system was established to decipher images from a long distance away.
Go to : 
CONCLUSION
IRT is a non-invasive and safe diagnostic method which visualizes functional abnormalities and is used effectively in the diagnosis of numerous diseases and in the evaluation of treatment effect. Compared to other imaging diagnostic methods, it shows high diagnostic performance in pain diseases, and even higher sensitivity and specificity is obtained when using the stress loading test. Together with the development in medical technology, it is anticipated that the use of IRT will gradually increase in the field of pain medicine.
Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download