Abstract
Background
Postherpetic neuralgia (PHN) is a serious complication resulting from herpes zoster infections, and it can impair the quality of life. In order to relieve pain from PHN, various treatments, including pharmacological and interventional methods have been used. However, little information on the recommendations for the interventional treatment of PHN, along with a lack of nation-wide surveys on the current status of PHN treatment exists. This multicenter study is the first survey on the treatment status of PHN in Korea.
Methods
Retrospective chart reviews were conducted on the entire patients who visited the pain clinics of 11 teaching hospitals from January to December of 2011. Co-morbid disease, affected site of PHN, routes to pain clinic visits, parenteral/topical medications for treatment, drugs used for nerve block, types and frequency of nerve blocks were investigated.
Results
A total of 1,414 patients' medical records were reviewed. The most commonly affected site was the thoracic area. The anticonvulsants and interlaminar epidural blocks were the most frequently used pharmacological and interventional methods for PHN treatment. For the interval of epidural block, intervals of 5 or more-weeks were the most popular. The proportion of PHN patients who get information from the mass media or the internet was only 0.8%.The incidence of suspected zoster sine herpete was only 0.1%.
Go to : 
Postherpetic neuralgia (PHN) is the most debilitating and common complications of herpes zoster (HZ). Pain from PHN causes adverse impacts on the quality of life of patients, especially in the elderly [1]. Although there is no consensus on the precise definition of PHN, in general, pain which may persist for months or years after the healing of skin lesions at the HZ site is generally considered PHN. According to an epidemiologic study, the incidence of persistent pain is 19.5% and 13.7% 1 and 3 months after HZ, respectively [2]. It is also reported that the incidence of PHN increases with age, about 10-20% of patients aged over 50, experience PHN after HZ infection, and about 30% of patients aged over 80, experience PHN [2,3]. Also, PHN causes social issues because of its high prevalence in the elderly and economic burden on the national health care system [4]. For the treatment of PHN, both pharmacologic and non-pharmacologic methods have been used [5]. There have been many efforts to optimize the medical treatment of PHN [6,7], thus as a result, the medical treatment of PHN is performed according to the available pharmacologic treatment guidelines or recommendations. Nevertheless, the management of PHN is often suboptimal [8]. In the field of pain medicine, many pain practitioners perform various interventional treatments for PHN, and new methods are being applied [9,10]. However, there is little information on the recommendations or practice guidelines for the interventional treatment of PHN, which forces pain clinicians to apply different interventional methods in the treatment of PHN. Therefore, considerable variations throughout Korea are being applied in the interventional treatment methods for PHN. To overcome this problem, the 'Research and Development Committee' of the Korean Pain Society decided to conduct a multicenter survey on the treatment of PHN in Korea. This is the first multicenter study on the current status of PHN treatment in Korea. We think that this study will be baseline data in establishing the recommendations for PHN treatment.
Go to : 
A total of 11 teaching hospitals, a part of the Korean Pain Society, participated in this study. This study was approved by the institutional review board of each hospital. In these hospitals, interventional pain management is conducted by a certified pain specialist. We conducted retrospective chart reviews on patients who met the following criteria; ① new-visit or first visit patients to the pain clinic of the 11 hospitals during the periods from January to December 2011, and ② patients who complained of herpes zoster related pain, regardless of the duration of the symptoms. For the retrospective chart reviews, the information for the following items were collected from each patient: age, sex, period before PHN treatment, co-morbid disease, PHN site, routes to pain clinic visit, parenteral/topical medications for treatment, types and frequency of nerve blocks, additives used for nerve blocks, and other treatment methods used. PASW® version 17.0 software (Chicago, IL, USA) was used for the statistical analysis. Descriptive statistical analyses were conducted from these data and the results are expressed as frequency, percentage, and means ± standard deviation (SD).
Go to : 
A total of 1,414 patients from 11 hospitals were enrolled for this study. The period before PHN treatment was ranged from 0 to 312 months (median 1 month). The demographic data were presented in the Table 1.
Among the data available for the 1,361 patients, only 274 patients (20.1%) had co-morbid disease, which were related to immune problems; diabetes (192 patients, 14.1%), cancer (75 patients, 5.5%), and immune-suppression (7 patients, 0.5%). However, contrary to our expectations, 603 patients (44.3%) had other chronic diseases that were not related to immune-compromised states (e.g., hypertension or hypercholesterolemia, etc.), and the remaining 496 patients (36.4%) were free from any co-morbid diseases.
The most commonly affected site was the thoracic area (772 patients, 52.9%), followed by the trigeminal area (228 patients, 15.6%; V1/V2/V3 = 136/54/38). The suspected zoster sine herpete (ZSH) was only found in 2 patients (0.1%). The affected PHN sites are presented in Fig. 1.
Only the data for 881 patients were available for this retrospective study. Among these cases, the main route for the pain clinic visit was through a referral from another department of the hospital (711 patients, 80.7%). Other patients visited the pain clinic without any referrals; via recommendations for pain clinic visits by acquaintances (31 patients, 3.5%), via internet searching (4 patients, 0.5%), and via mass media (newspaper, TV, and radio, 3 patients 0.3%). The remaining patients (15.0%) visited the pain clinic via other routes.
A total of 1,362 patients' data for this category was available, with most of these patients taking a combination of 2 or more kinds of medication. The most frequently used medication was anticonvulsants (1,141 cases, 83.8%), followed by acetaminophen/non-steroidal anti-inflammatory drugs (NSAIDs) (773 cases, 56.8%), tricyclic antidepressants (TCA) (742 cases, 54.5%), tramadol (725 cases, 53.2%), and opioids (251 cases, 18.4%). Fig. 2 illustrates the parenteral/topical medications used for the treatment of PHN.
A total of 1,398 patients were available, among them, 1,184 patients were affected with PHN at the spinal (from cervical to sacral dermatome) region, and 214 patients were affected at the craniofacial region. In the 1,184 patients who were affected with PHN at the spinal area, a total of 1,126 patients received nerve blocks; interlaminar (IL) epidural injection was the most frequently performed (368 cases, 32.7%), followed by peripheral nerve block (317 cases, 28.2%), transforaminal (TF) epidural injection (219 cases, 19.4%), paravertebral block (113 cases, 10.0%), and sympathetic block (109 cases, 9.7%). In the 214 patients who were affected with PHN at the craniofacial area, a total of 208 patients received nerve blocks; on the contrary to the patients who were affected with PHN at the spinal region, the sympathetic block was most frequently performed (87 cases, 41.8%) in the craniofacial region. Cranial nerve block and peripheral nerve block were performed in 77 cases (37.0%) and 44 cases (21.2%), respectively, both performed in the craniofacial region. The local anesthetics used for the nerve block are illustrated in Fig. 3.
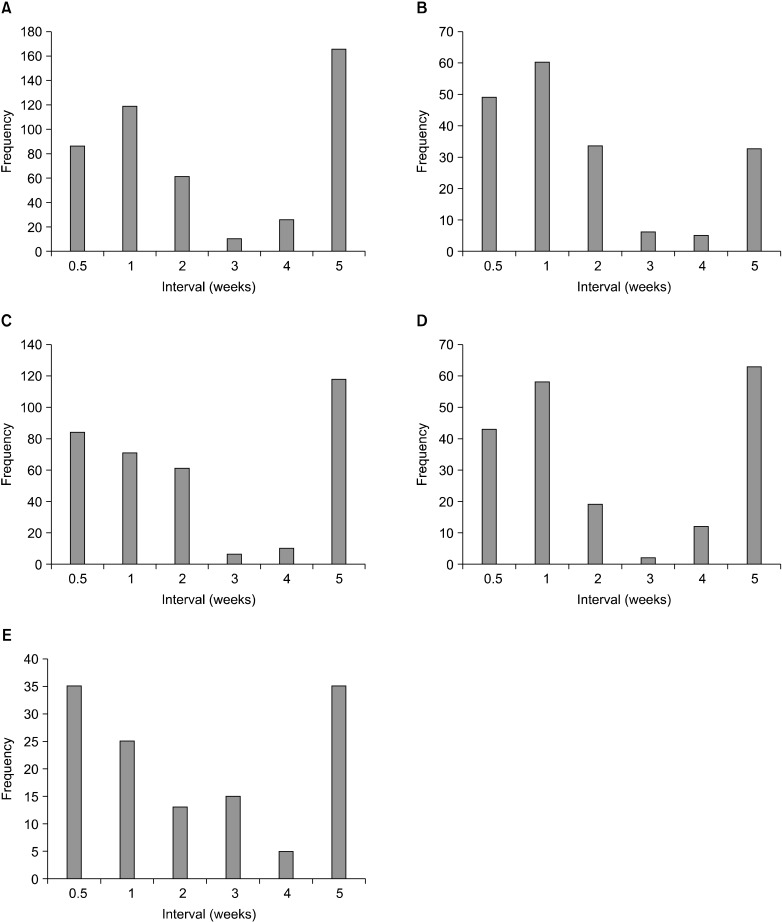
A total of 457/183/350/196/128 patients' data were available for epidural (interlaminar or transforaminal)/sympathetic/peripheral/paravertebral/cranial nerve block, respectively. There were 2 distinctive peaks in the distribution for the injection intervals. For the epidural injections, 5 or more-week intervals were the most popular (162 patients, 35.4%), followed by the 1-week intervals (116 patients, 25.4%). The sympathetic blocks were performed with short intervals; mainly performed with 1 week intervals (59 patients, 32.2%). For the peripheral nerve blocks, 5 or more-week intervals were the most popular (118 patients, 33.7%), followed by the twice-a-week intervals (84 patients, 24.0%). For the paravertebral block, the most popular interval was the 5 or more-week intervals (62 patients, 31.5%), followed by the 1 week intervals (58 patients, 29.4%). For the cranial nerve block, twice-a-week intervals and 5 or more-week intervals were equally popular (35 patients, 27.3%), Fig. 4 illustrates the intervals of each type of block.
Intravenous infusion treatments were used in 335 patients; ketamine (58 patients, 17.3%), magnesium (48 patients, 14.3%), lidocaine (25 patients, 7.5%), vitamin C (29 patients, 8.7%), and multi-vitamin and/or other drugs (175 patients, 51.9%).
A total of 963 patients' data were available. Triamcinoline acetonide was the most frequently used additive for the nerve blocks (509 patients, 52.9%), followed by ketamine (149 patients, 15.5%), betamethasone (63 cases, 6.5%), and dexamethasone (52 patients, 5.4%). Magnesium and other additives were used in 190 cases (19.7%). The mean dosage of the additives employed for the single nerve blocks are described in Table 2.
Among the 1,414 patients, pulsed radiofrequency (RF) lesioning and heat RF were performed only on 70 (4.95%) and 14 patients (0.99%), respectively. Only 1 patient (0.07%) received both pulsed and heat RF in combination. The intrathecal steroid injection was performed on 3 patients (0.21%), and alcohol neurolysis was performed on 4 patients (0.28%).
Go to : 
In this study, we found that anticonvulsants were the most frequently used in the treatment of PHN, which is in accord with the findings of the previous guidelines for neuropathic pain management [7,11]. However, there were considerable variations in applying interventional treatments, especially for the intervals of the nerve block; the nerve blocks were performed with 1 week intervals or intervals of 5 or more weeks (2 distinctive peaks). These findings meant that there was no consensus on the proper interval for nerve block treatment of PHN. Although there have been several interventional treatment guidelines for spinal pain [8,12,13], there is no information available on how to apply and when to apply these interventional methods for the treatment of PHN. Moreover, whether epidural steroid administration itself has an additive effect on the remedy of PHN is also questioned [14]. Therefore, further studies or expert meetings are required to establish recommendations for the interventional treatment of PHN.
The most frequently used nerve block for PHN in the spinal region was IL epidural injection; this may be due to the result of the ease in performing this procedure, because the IL approach is usually performed in a blind manner. Although there are no comparative studies on the effect of interlaminar and transforaminal injections for PHN treatment, based on the fact that the TF approach has advantages over the IL approach due to its precise flow to the targeted dorsal root ganglion and spinal nerve with the smallest volume, there is no evidence and there seems to be no specific reason to prefer the IL approach over the TF approach in the epidural injection for PHN treatment.
In our study, the incidence of suspected ZSH was 0.2%. ZSH is difficult to diagnose and is often confused with other diseases [15] because it does not have the typical vesicular skin lesions. Currently, there is no information available on the incidences of ZSH. Although the incidence of ZSH in our study is not proven serologically, based on the clinical suspicion of ZSH however, the results seem to be the first report on the incidence of ZSH among PHN patients.
For the co-morbid disease, only 274 patients (20.1%) had co-morbid diseases which were related to compromised immunity, and 496 patients (36.4%) were free from any co-morbid diseases. These findings suggest that even a healthy elderly person, who does not have any co-morbid diseases, can suffer from PHN, and the zoster vaccine can be beneficial for the prevention of herpes zoster and PHN in these elderly patients.
There are some limitations to our study. First, this is a retrospective study therefore, large amounts of missing or unknown data existed. To overcome this problem, prospective cohort studies are required. Second, this study included only teaching hospitals in Korea. At the initial planning stages of this survey, the Korean Pain Society sent official mail to all society members to participate in this survey however, there were only responses from 11 teaching hospitals, and none from private hospitals. Therefore, the results of this survey may not reflect the circumstances of private hospitals. Third, this survey did not investigate the treatment effects of each interventional treatment. In this survey, we did not focus on 'which treatment is effective', but on the 'how PHN is treated in Korea'. Although the topic of 'what is the best practice for PHN treatment' cannot be answered in our study, we think that the results of our study can be a cornerstone in the development of treatment strategies for PHN. Further research should be carried out to obtain more conclusive information. In conclusion, the methods for PHN treatment vary among hospitals. The establishment of treatment recommendations for PHN is necessary as a result.
Go to : 
References
1. Drolet M, Brisson M, Schmader KE, Levin MJ, Johnson R, Oxman MN, et al. The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. CMAJ. 2010; 182:1731–1736. PMID: 20921251.

2. Gauthier A, Breuer J, Carrington D, Martin M, Rémy V. Epidemiology and cost of herpes zoster and post-herpetic neuralgia in the United Kingdom. Epidemiol Infect. 2009; 137:38–47. PMID: 18466661.

3. Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007; 82:1341–1349. PMID: 17976353.

4. Gialloreti LE, Merito M, Pezzotti P, Naldi L, Gatti A, Beillat M, et al. Epidemiology and economic burden of herpes zoster and post-herpetic neuralgia in Italy: a retrospective, population-based study. BMC Infect Dis. 2010; 10:230. PMID: 20682044.

5. Sim WS, Choi JH, Han KR, Kim YC. Treatment of herpes zoster and postherpetic neuralgia. Korean J Pain. 2008; 21:93–105.

6. Argoff CE. Review of current guidelines on the care of postherpetic neuralgia. Postgrad Med. 2011; 123:134–142. PMID: 21904096.

7. Dworkin RH, O'Connor AB, Backonja M, Farrar JT, Finnerup NB, Jensen TS, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007; 132:237–251. PMID: 17920770.

8. Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. ASIPP-IPM. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009; 12:699–802. PMID: 19644537.
9. Baek IY, Park JY, Kim HJ, Yoon JU, Byoen GJ, Kim KH. Spinal cord stimulation in the treatment of postherpetic neuralgia in patients with chronic kidney disease: a case series and review of the literature. Korean J Pain. 2011; 24:154–157. PMID: 21935494.

10. Byun SH, Jeon Y. Administration of vitamin c in a patient with herpes zoster: a case report. Korean J Pain. 2011; 24:108–111. PMID: 21716609.

11. Attal N, Cruccu G, Haanpää M, Hansson P, Jensen TS, Nurmikko T, et al. EFNS Task Force. EFNS guidelines on pharmacological treatment of neuropathic pain. Eur J Neurol. 2006; 13:1153–1169. PMID: 17038030.

12. Deer T, Ranson M, Kapural L, Diwan SA. Guidelines for the proper use of epidural steroid injections for the chronic pain patient. Tech Reg Anesth Pain Manag. 2009; 13:288–295.

13. Boswell MV, Shah RV, Everett CR, Sehgal N, McKenzie Brown AM, Abdi S, et al. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Physician. 2005; 8:1–47. PMID: 16850041.
14. Hempenstall K, Nurmikko TJ, Johnson RW, A'Hern RP, Rice AS. Analgesic therapy in postherpetic neuralgia: a quantitative systematic review. PLoS Med. 2005; 2:e164. PMID: 16013891.

Go to : 




 PDF
PDF Citation
Citation Print
Print







 XML Download
XML Download