This article has been
cited by other articles in ScienceCentral.
Abstract
A C2-3 zygapophygeal joint is a major source of cervicogenic headache. Radiofrequency (RF) neurotomy is preformed widely for zygapophygeal joint pain. Conventional RF denervation technique is generally performed under fluoroscopic control. Recently, ultrasound-guided radiofrequency on zygapophygeal joint has emerged as an alternative method. We report our experiences of two successful ultrasound-guided pulsed radiofrequencies on 39-year-old and 42-year-old males, who complained occipital headache and posterior neck pain.
Go to :

Keywords: pulsed radiofrequency, third occipital nerve, ultrasound
A cervical zygapophygeal joint is one of the common causes of chronic neck pain. The origin of pain can be one or more cervical zygapophygeal joints in more than 50% of chronic neck pain patients after whiplash injury. An experimental study on normal volunteers have indicated that pain from C2-3 zygapophygeal joint is expressed as a headache [
1]. This form of headache has been named as third occipital headache [
2,
3]. Among patients with whiplash injury, the prevalence of third occipital headache is 27% [
3]. A C2-3 zygapophygeal joint is a major source of cervicogenic headache, and third occipital nerve (TON) mainly innervates this joint [
4].
Since the introduction of radiofrequency (RF) neurotomy by Sluijter et al. [
5] in 1980, it has been validated as an effective treatment for zygapophysial joint pain. Nowadays, pulsed radiofrequency is performed widely to minimize thermal injury of the neural tissue [
6].
Diagnostic block or RF of cervical medial branch are commonly performed under fluoroscopic control, however, target nerve is radiolucent, not visualized by fluoroscopy. Furthermore, with use of fluoroscopy, patients and physicians can be exposed to considerable amount of radiation.
Unlike fluoroscopy, ultrasound does not involve radiation. Recently, ultrasound guidance of procedure has emerged as an alternative method for lumbar medial branch block. Further, there have been a few reports on ultrasound-guided cervical zygapophygeal joint block and RF neurotomy [
7,
8].
We report our experience of two successful pulsed radiofrequency treatments of TON using an ultrasound.
CASE REPORT
The first patient is a 39-year-old male who complained of posterior neck pain and occipital headache on the right side after a rear-end collision, which occurred one month ago. At the time of the accident, he suffered from radiating pain in the right arm, but the radiating symptom subsided by the time of his first visit to the clinic. There were no specific findings on cervical MRI. Diagnostic block on the right TON was performed with 0.9 ml of 1% lidocaine. Two weeks later, the block was done with 0.9 ml of 0.25% bupivacaine. There were 50% pain reductions after each block. After confirmation of positive responses, the patient underwent pulsed radiofrequency of the right third occipital nerve under fluoroscopic control. A 22-gauge, 10-cm-long, 10-mm active tip RFK needle (Radionics Inc., Burlington, MA, USA) was used. Symptom subsided, but 8 months later, the same symptom on the right occipital area and posterior neck pain recurred. Another diagnostic block was performed under ultrasound control, and pain relief was achieved. With pain relief, we decided to perform ultrasound guided pulsed radiofrequency of TON.
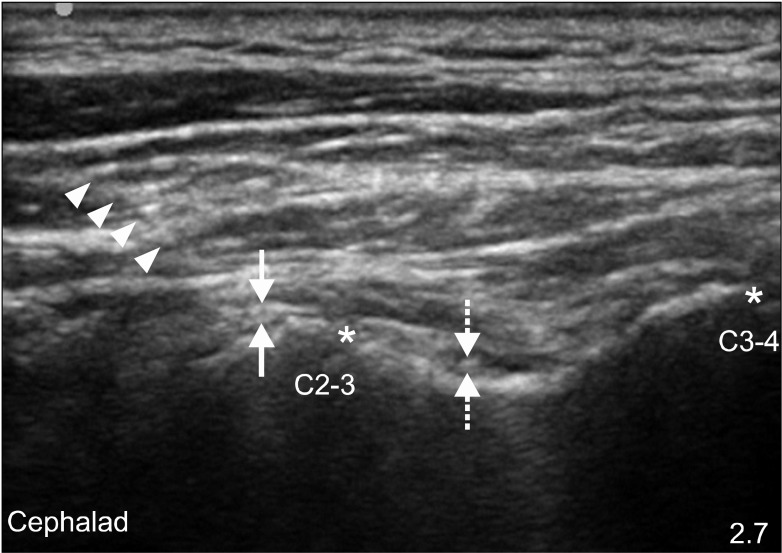
The patient was in the left lateral decubitus position. We first located 5-12 MHz linear ultrasound transducer (SonoSite Inc., Washington, USA) on the mastoid process, longitudinally. Moving the transducer more caudally, we found C2-3 zygapophygeal joint. TON was founded as a hypoechoic oval shape encircled by a hyperechoic halo at C2-3 zygapophygeal joint line (
Fig. 1). C3 deep medial branch nerve was also founded at the middle of the articular pillar of C3 (
Fig. 1). The RFK needle used in previous pulsed radiofrequency was inserted to TON craniocaudally, using an in-plane approach (
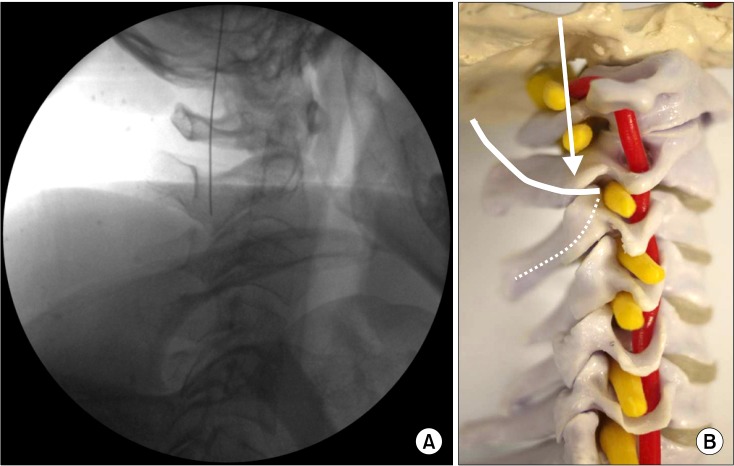
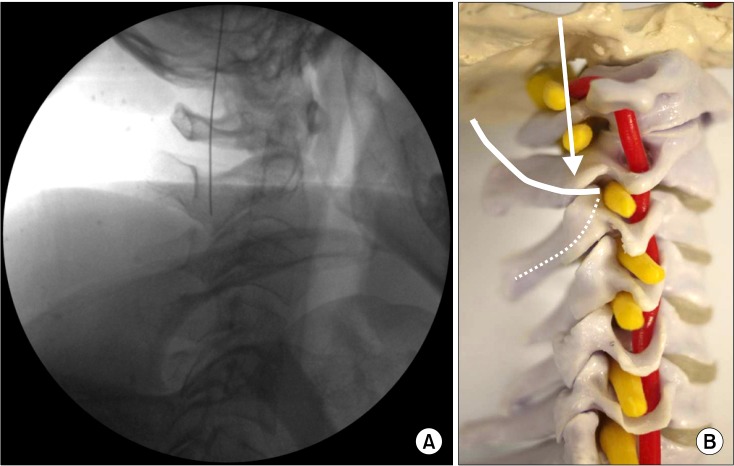
Fig. 2). Response to sensory stimulation was checked at 50 Hz, 0.5 V, and pulsed radiofrequency was conducted twice for 120 seconds on 42℃. In order to confirm the exact location, we cross checked the image with fluoroscopic view (
Fig. 3A). Same manner of approach was used for C3 deep medial branch, and we terminated the procedure. Patient's numerical rating scale (NRS) decreased from 7 to 2. Four months after the procedure, patient's pain is maintained at NRS 2, and he is on a regular departmental outpatient follow up.
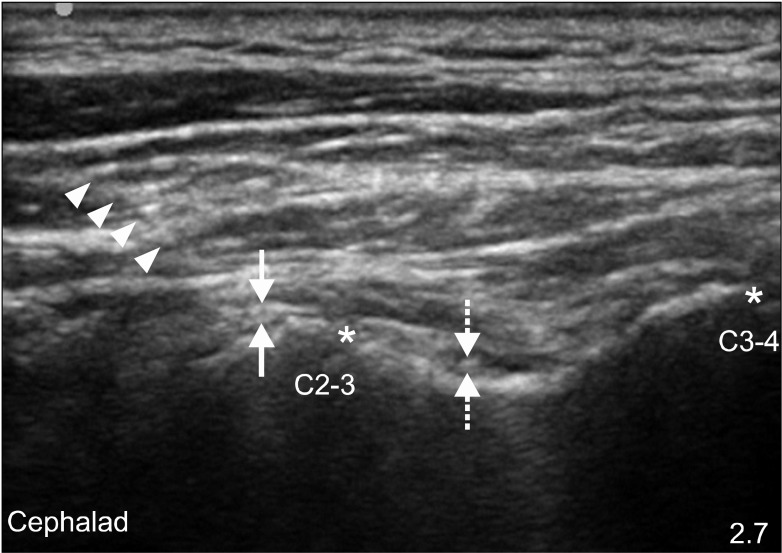 | Fig. 1Ultrasound images of pulsed radiofrequency on the third occipital nerve. Arrowheads indicate radiofrequency (RF) needle. Arrows indicate third occipital nerve. Dotted arrows indicate C3 medial branch nerve. Asterisks indicate zygapophygeal joints. 
|
 | Fig. 2Craniocaudal insertion of needle electrode using in-plane technique. 
|
 | Fig. 3Fluoroscopic image to confirm needle tip placement (A) and schematic drawing of TON and C3 deep medial branch nerve (B). (A) Needle electrode is placed in accurate level and in relatively perpendicular to TON. (B) Upper solid line indicates to TON. Lower dotted line indicates to C3 deep medial branch nerve. Arrow indicates to expected direction of electrode needle. 
|
The second patient is a 42-year-old male with right occipital headache, and posterior neck pain after artificial disc implantation at C4-5 and C6-7 levels. Before his visit to our hospital, he received cervical epidural injections, neuroplasty, and physical therapy at other hospitals, but effects were minimal. We first performed percutaneous neuroplasty. After neuroplasty, posterior neck pain was relieved. However, pain on the right occipital area remained. Two times of diagnostic TON blocks were performed as same as the first case and the patient showed positive responses to each blocks. We decided to perform pulsed radiofrequency under ultrasound guidance. The procedure was done as the same manner as the first. Patient's NRS decreased from 8 to 3. One year after the procedure, patient does not show increase in NRS, and he is also on a regular follow up.
Go to :

DISCUSSION
There was a report in the mid-80's, where TON block showed relief of headache in 70-80% of occipital headache patients [
2]. This report suggested C2-3 zygapophygeal joint as the main cause of cervicogenic headache. C2-3 zygapophygeal joint is mainly innervated by TON, C3 deep medial branch and C2 communicating branch also innervate C2-3 zygapophygeal joint. In this study, we performed pulsed radiofrequency on both TON as well as C3 deep medial branch.
Diagnostic block of cervical medial branch is the sole method of cervical zygapophygeal joint pain diagnosis [
9]. Two individual blocks should be performed on a different day to reduce false positive response [
10]. Following positive response to diagnostic blocks, RF neurotomy is then indicated.
Considering the possible anatomical variations of TON, blocks on three target points are required for diagnostic block or RF neurotomy under fluoroscopic control [
11].
Recently, there are several studies on an ultrasound anatomy of cervical zygapophygeal joints and cervical medial branches [
12], and ultrasound-guided cervical medial branch blocks [
7]. Siegenthaler et al. [
12] reported a successful visualization of TON in 96%. Eichenberger et al. [
7] also reported that they could find the correct level of C2-3 joint and were able to perform TON block on ultrasound guidance. They reported that TON was seen under ultrasound in 27 of 28 cases. According to their study and anatomy of TON, the nerve can be visualized better in a longitudinal view, rather than in a transverse one. In present cases, we were also able to easily visualize TON in a longitudinal view.
In nerve block under ultrasound guidance, relatively large amount of injection is used, and ambiguous visualization of the target nerve is acceptable. However, if RF neurotomy is to be performed, accurate visualization of target nerve may be very crucial.
There has been a report on ultrasound-guided cervical medial branch RF neurotomy [
8], but no reports on ultrasound-guided TON radiofrequency. Lee et al. [
8] described RF neurotomy in the cervical spine. In their cases, zygapophygeal joint level and medial branch nerve were confirmed in the longitudinal view, once confirmed, transducer was rotated 90 degrees for a parallel introduction of the electrode to the target nerve with an in-plane technique.
When performing RF neurotomy at the other levels, the waist of articular pillar was served as a bony landmark. However, in case of TON, they could not find appropriate bony landmark in transverse view for ultrasound-guidance radiofrequency lesioning Therefore, RF neurotomy of TON could not be performed in their study.
Unlike the conventional RF neurotomy, it is believed that therapeutic effect of pulsed radiofrequency is obtained by delivering an electromagnetic field procuced by RF current [
13]. Recent experimental studies show pulsed radiofrequency causing an increase in the c-fos expression [
14,
15] and synaptic change in transmission [
16]. However, the exact analgesic mechanism is yet to be known.
Although, there is a lack of evidence for equal effectiveness compared to that of the conventional RF, pulsed radiofrequency is now performed with worldwide popularity in order to reduce thermal injury to the neural tissue.
Density of electrical field is greatest at the distal tip of an electrode. So when performing a pulsed radiofrequency, electrode should be placed perpendicular to the target nerve, whereas, in conventional RF, electrode is placed parallel to the nerve [
17,
18].
While performing pulsed radiofrequency on TON, craniocaudal insertion of needle electrode with longitudinal view is expected to make relatively perpendicular placement of the electrode to TON. When pulsed radiofrequency is to be performed on a lateral decubitus position, needle handling is interferred by shoulder joint. In order to reduce such interference, we used craniocaudal approach, and to avoid C2 nerve root injury during needle insertion, we took careful attention to neurologic sign, such as parasthesia.
It can be checked with fluoroscopic image of our cases (
Fig. 3A, B). It is difficult to perform with conventional method under fluoroscopic guidance.
In order to accommodate a possible anatomical variation of TON, the conventional RF technique with fluoroscopy need to place needle electrode onto three target points. This multiple placements of the needle can lead to prolongation of the procedure time, causing excessive exposure to radiation.
Ultrasound guidance may overcome these limitations. Since the target nerve can be visualized, the needle electrode can be introduced directly onto the nerve in real-time. Also, multiple needling can be reduced, and related complications can be minimized, such as bleeding, tissue injury, and infections.
In this study, we suggest a new method of pulsed radiofrequency on TON with ultrasound guidance. Due to physical characteristics of pulsed radiofrequency, parallel placement of active needle tip to target nerve is not necessary. Therefore, ultrasound-guided pulsed radiofrequency attempt on other cervical medial branches can be made as in the same manner as our report, and further study is needed.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download