Abstract
Infective spondylodiscitis is a rare complication that can occur after interventional spinal procedures, of which symptoms are usually back pain and fever. Early diagnosis of infective spondylodiscitis is critical to start antibiotics and to improve prognosis. Laboratory examinations including complet blood cell count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are conventional tools for the early detection of infectious spondylitis. However, we experienced infective spondylodiscitis after cervical nucleoplasty which did not display any laboratory abnormalities, but was diagnosed through an MRI. A patient with cervical disc herniation received nucleoplasty at C5/6 and C6/7. One month later, the patient complained of aggravated pain. There were neither signs of chill nor fever, and the laboratory results appeared normal. However, the MRI findings were compatible with infectious spondylodiscitis at the nucleoplasty site. In conclusion, infectious spondylodiscitis can develop after cervical nucleoplasty without any laboratory abnormalities. Therefore, an MRI should be taken when there is a clinical suspicion for infection in order to not miss complications after interventional procedures, even if the laboratory findings are normal.
Infectious spondylodiscitis is a rare complication that can occur after spinal procedures, and its incidence is known to be 0.05-5.3% [1,2]. Suspicion and clinical diagnosis of this complication can be made within a few days or even up to 8 years after the spinal procedure, which depends on the pathogen and the individual's immune status [3-5]. It is important to diagnose this complication at its early stage in order to shorten hospitalization and reduce sequelae. Usually, spondylodiscitis is companied by back pain and fever as its general symptoms [6]. Laboratory findings are important for diagnosis. C reactive protein (CRP) and the erythrocyte sedimentation rate (ESR) are the most sensitive tests [6,7], and the sensitivity and specificity of CRP is reported to be 63% and 82% [8]. It is suggested that infection should be suspected when the ESR is higher than 45 mm/hr and the CRP is higher than 2.5 mg/dl on the 5-6th day [1]. Cervical nucleoplasty is a minimally invasive intradiscal procedure for cervical disc disorders, which uses the coblation technique [9]. Theoretically, spondylodiscitis can develop as a complication to nucleoplasty. However, there have been no case reports on spondylodiscitis without any laboratory findings after cervical nucleoplasty. Here, we report postoperative spondylodiscitis after cervical nucleoplasty, which displayed no abnormalities in the laboratory findings, but was diagnosed through magnetic resonance imaging (MRI).
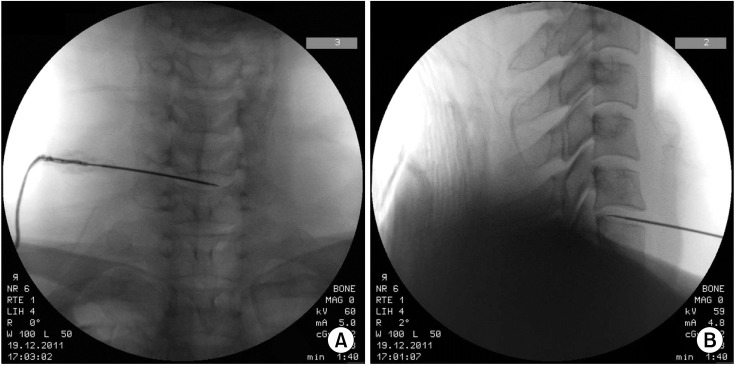
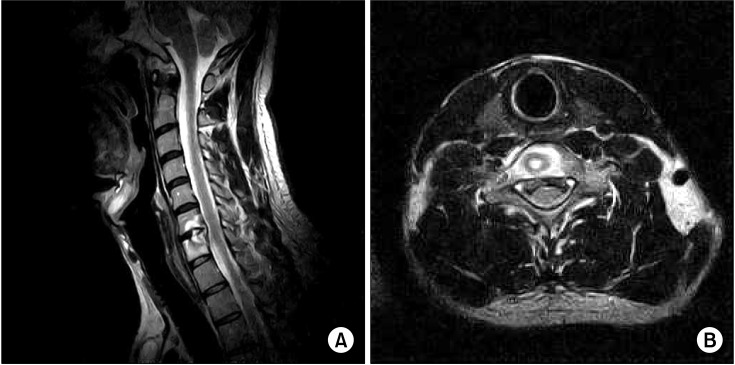
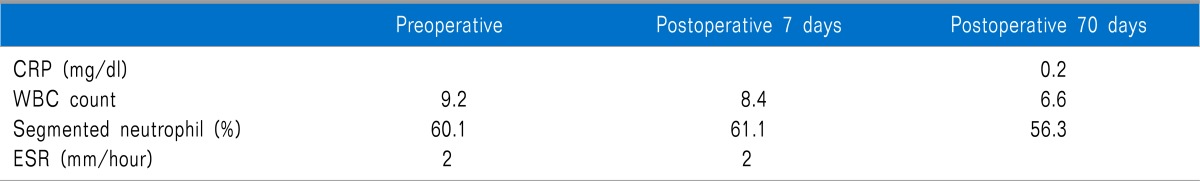
A 33-year-old male (height 172.3 cm and weight 61.5 kg) visited our pain clinic due to neck pain radiating to both shoulders, which started 3 years ago. He complained of tingling sensations of the bilateral hand along with shoulder pain, and difficulty in neck flexion. Upon physical examination, the results of the Jackson compression test and the Spurling's test did not appear positive. On the cervical MRI, C5/6 and C6/7 intervertebral disc protrusions were found and chronic right C6 radiculopathy was found on the electromyography. This patient had already received an epidural steroid injection and decompressive neuroplasty using a Racz's catheter at a local hospital. However, the symptoms were not relieved. Therefore, we decided to perform cervical nucleoplasty at the C5/6 and C6/7 intervertebral discs. On the pre-procedural laboratory tests, there were no abnormalities in the CBC, ESR, and blood chemistry test (Table 1). In addition, there were no general underlying diseases. Nucleoplasty was performed on the C5/6 and C6/7 intervertebral discs without any perioperative events. Under a supine position, skin preparation was performed with betadine soap and 2% chlorhexidine-70% isoprophyl alcohol solution, and a sterile surgical drape was applied. The nucleoplasty procedure was performed in the same manner as reported previously [9]. After the internal carotid was laterally displaced, a 19 gauge 3 inch introducer needle was introduced till the anterolateral annulus fibrosus. After the needle was advanced deeper, the position of the needle was adjusted to reach the target site of the herniated disc under a C-arm guide. When the needle reached the proper target site, the stylet of the introducer needle was withdrawn, and the Perc™ DC spine Wand™ (ArthroCare Co., Sunnyvale, CA, USA) was replaced and fastened to the needle hub. Next, the Perc™ DC spine Wand™ was connected to the Arthrocare system 2,000®. After confirming that there was no cervical root stimulation, Coblation® was then carried out by rotating the flange 180° for 20 seconds. After this, the wand was retracted 1-2 mm under C-arm guidance and the same procedure was repeated 3 times. This procedure was repeated at each disc level (Fig. 1). During the hospital stay, the body temperature was 36.7-36.9℃ and there were no signs or symptoms of acute complications. Prophylactic antibiotic therapy with intravenous cefazoline 1 g was administered prior to nucleoplasty. An additional amount of intravenous cefazolin was administered three times a day and a routine prophylaxis for 2 more days during the hospital stay. Additional oral cefradine was prescribed 1,000 mg/day for 1 week after the patient's discharge. After 8 days, the patient revisited our outpatient clinic for routine postoperative checkup, but there were no improvements in the patient's symptoms. In addition, there were no symptoms or signs of infection including fever or chills, and the laboratory findings, such as the CBC and ESR, were in the normal range. After 2 months, during his second postoperative visit to our clinic, the patient complained of right shoulder pain and worsening neck pain during flexion. He also complained of feelings of weakness in both arms, but his motor functions were intact when a physical examination was performed. In addition, new physical signs developed; the Jackson compression test and Spurling's test were positive, with radiating pain in both shoulders. There was tenderness on the right cervical facet joint, but no tenderness was observed on the left side. The CBC and CRP were normal. The body temperature was normal, and there was no sensation of chills. In order to evaluate the focus of the pain, a cervical MRI was performed, and the findings were compatible with spondylodiscitis at the C6/7 intervertebral disc and the vertebral body (Fig. 2). The patient was referred to the neurosurgery department immediately, and intravenous antibiotics therapy was planned. However, with the patient's will, he was transferred to another hospital for long-term antibiotics therapy. After 6 weeks of antibiotics treatment, the patient's symptoms were relieved markedly.
Early diagnosis and treatment of spondylodiscitis is important for the prevention of catastrophic sequelae and huge additional expenses [2]. Therefore, it is essential to understand the natural course of postoperative spondylodiscitis. Usually, short-term relief of the symptoms comes first after surgery, and then back pain recurs within 6 weeks [10,11]. According to Bavinzski et al. [6], most patients became symptomatic within four weeks [6]. In addition, fever was a typical symptom associated with this infection. In our case, neck pain was aggravated and new positive signs in the physical exam appeared 8 weeks after the procedure. Moreover, our patient was afebrile, which can be explained by the lack of elevation of an inflammatory marker. The ESR and CRP are known as the earliest and most sensitive screening tools for the infection. Furthermore, they are cost-effective as well. Meyer et al. suggested the sensitivity and specificity of CRP as 100% and 95.8%, respectively, when predicting postoperative infections [12]. In addition, Mustard et al. conducted a study on 108 patients, and a positive CRP response was defined as meeting two criteria [8]: ① on days 3 and 4, the CRP level is >80% of day 2 (positive diagnosis by day 4); and ② after day 4, the CRP rises on 2 consecutive days with a level greater than 15 mg/L for each day (positive diagnosis by day 6). The above criteria had a sensitivity of 63%, a specificity of 82%, a positive predictive value of 68% and a negative predictive value of 78%. Bircher et al. recommended that an ESR of more than 50 mm/hr for more than 2 weeks after surgery be used as an early diagnostic marker for spondylodiscitis, indicating a need to perform more tests [13]. However, during the early postoperative period, the CRP and ESR may rise as a consequence of tissue damage caused by the surgery itself. Kwon et al. found that the CRP and White blood cell (WBC) rose starting on the first day of surgery and decreased after the third postoperative day, and the ESR elevation lasted up to 11 days after spine surgery [14]. To screen postoperative infections with laboratory tests, adequate follow up periods and tests should be considered, with further evaluations being needed to confirm spondylodiscitis. Based on the previous studies, CRP should be checked 4 days after the surgery and compared with a baseline value (preoperative value), while the ESR should be checked 12 days after the surgery. There has been a reported case of spondylodiscitis following cervical nucleoplasty: in theat case, the complication was detected 3 weeks after the procedure [3]. In our case, outpatient follow-ups were performed 9 days and 8 weeks after the operation. During the first visit, the ESR was normal and not different from the preoperative laboratory results. In our case, neither the infection nor the procedure itself increased the ESR and CRP. This may be due to the minimal invasiveness of cervical nucleoplasty. Further research is needed to clarify the changes of the inflammatory marker after nucleoplasty. At the second visit, the CRP was checked and was identified to be within the normal range. During the 8-week postoperative follow-up, we could not find any abnormalities in the laboratory tests even when the MRI showed apparent infection. There have been many studies on this feature of spondylodiscitis. Citak et al. reported that 43.7% of 183 patients with spondylodiscitis had neurologic deficits and variable pain [15]. Bavinzski et al. reported a series of 13 patients with postoperative disc space infection. All patients suffered from severe local lumbar pain with muscle cramps and radiating pain to the hips, abdomen, legs, scrotum, groin, or perineum. Many patients were unable to stand, with the pain exacerbated by motions of the spine segments [6]. In a recent review article, the typical course of spondylodiscitis is the return of low back pain approximately six weeks later [16]. Similar to the previous studies, our patient also complained about pain being aggravated by motion and local tenderness around the infection site about 8 weeks after the spinal procedure. Therefore, clinicians should be careful if patients complain of aggravated pain about 6 weeks post-operation, while additional studies are required to diagnose the infection. When spondylitis or discitis is identified, medical or surgical treatment should be performed. If there is no neurologic or structural instability, it is recommended that antimicrobial therapy should be withheld until positive identification of the organism is achieved unless back pain is accompanied by systemic symptoms [1]. However, in our case, the infection was identified at the site of nucleoplasty 2 months later, and the patient's symptoms were aggravated. Therefore, the infection was considered to be a procedure-related problem and empirical antibiotics therapy was initiated. Surgical intervention is recommended in cases of impending pathologic fractures, functionally significant neurologic deficits, paravertebral or epidural abscess formations, persistent septicemia despite antibiotic treatment, intractable pain, and unacceptable saggital or coronal plane deformity [17]. We postulate that the pathogen may be sequestrated from the blood stream completely, therefore, systemic inflammatory changes were not triggered, or the immunity of this patient (33 year-old man) was strong enough to overcome the dispersion of the pathogen. For detecting postoperative discitis, MRI is the imaging method of choice, with its high sensitivity and specificity [18]. MRI is considered to be the most sensitive and specific method, 93% and 97%, as reported [19,20]. Furthermore, MRI is the gold standard for diagnosing spondylodiscitis. In conclusion, infectious spondylodiscitis can develop after cervical nucleoplasty without any laboratory abnormalities. Therefore, an MRI should be taken when there is clinical suspicion of infection in order to not miss the complications after interventional procedures, even if the laboratory findings were normal.
References
1. Di Martino A, Papapietro N, Lanotte A, Russo F, Vadalà G, Denaro V. Spondylodiscitis: standards of current treatment. Curr Med Res Opin. 2012; 28:689–699. PMID: 22435926.

2. Jiménez-Mejías ME, de Dios Colmenero J, Sánchez-Lora FJ, Palomino-Nicás J, Reguera JM, García de la Heras J, et al. Postoperative spondylodiskitis: etiology, clinical findings, prognosis, and comparison with nonoperative pyogenic spondylodiskitis. Clin Infect Dis. 1999; 29:339–345. PMID: 10476739.

3. Bonaldi G, Baruzzi F, Facchinetti A, Fachinetti P, Lunghi S. Plasma radio-frequency-based diskectomy for treatment of cervical herniated nucleus pulposus: feasibility, safety, and preliminary clinical results. AJNR Am J Neuroradiol. 2006; 27:2104–2111. PMID: 17110676.
4. Chen F, Lü G, Kang Y, Ma Z, Lu C, Wang B, et al. Mucormycosis spondylodiscitis after lumbar disc puncture. Eur Spine J. 2006; 15:370–376. PMID: 16328227.

5. Lotfinia I, Vahedi P. Late-onset post-diskectomy tuberculosis at the same operated lumbar level: case report and review of literature. Eur Spine J. 2010; 19(Suppl 2):S226–S232. PMID: 20446000.

6. Bavinzski G, Schoeggl A, Trattnig S, Standhardt H, Dietrich W, Reddy M, et al. Microsurgical management of postoperative disc space infection. Neurosurg Rev. 2003; 26:102–107. PMID: 12962295.

7. Schulitz KP, Assheuer J. Discitis after procedures on the intervertebral disc. Spine. 1994; 19:1172–1177. PMID: 8059276.

8. Mustard RA Jr, Bohnen JM, Haseeb S, Kasina R. C-reactive protein levels predict postoperative septic complications. Arch Surg. 1987; 122:69–73. PMID: 3800652.

9. Sim SE, Ko ES, Kim DK, Kim HK, Kim YC, Shin HY. The results of cervical nucleoplasty in patients with cervical disc disorder: a retrospective clinical study of 22 patients. Korean J Pain. 2011; 24:36–43. PMID: 21390177.

10. Ozuna RM, Delamarter RB. Pyogenic vertebral osteomyelitis and postsurgical disc space infections. Orthop Clin North Am. 1996; 27:87–94. PMID: 8539056.

11. Rohde V, Meyer B, Schaller C, Hassler WE. Spondylodiscitis after lumbar discectomy. Incidence and a proposal for prophylaxis. Spine. 1998; 23:615–620. PMID: 9530794.
12. Meyer B, Schaller K, Rohde V, Hassler W. The C-reactive protein for detection of early infections after lumbar microdiscectomy. Acta Neurochir. 1995; 136:145–150. PMID: 8748845.

13. Bircher MD, Tasker T, Crawshaw C, Mulholland RC. Discitis following lumbar surgery. Spine. 1988; 13:98–102. PMID: 3381147.

14. Kwon SC, Kim SJ, Shin HS, Park SK. Erythrocyte sedimentation rate, C-reactive protein, and white blood cell count after lumbar discectomy. J Korean Neurosurg Soc. 1998; 27:1508–1511.
15. Citak M, Backhaus M, Kälicke T, Hilal Z, Muhr G, Frangen TM. Myths and facts of spondylodiscitis: an analysis of 183 cases. Acta Orthop Belg. 2011; 77:535–538. PMID: 21954765.
16. Gerometta A, Bittan F, Rodriguez Olaverri JC. Postoperative spondilodiscitis. Int Orthop. 2012; 36:433–438. PMID: 22307558.

17. Zarghooni K, Röllinghoff M, Sobottke R, Eysel P. Treatment of spondylodiscitis. Int Orthop. 2012; 36:405–411. PMID: 22143315.

18. Palestro CJ, Love C, Miller TT. Infection and musculoskeletal conditions: imaging of musculoskeletal infections. Best Pract Res Clin Rheumatol. 2006; 20:1197–1218. PMID: 17127204.
19. Khan IA, Vaccaro AR, Zlotolow DA. Management of vertebral diskitis and osteomyelitis. Orthopedics. 1999; 22:758–765. PMID: 10465488.

20. Maiuri F, Iaconetta G, Gallicchio B, Manto A, Briganti F. Spondylodiscitis. Clinical and magnetic resonance diagnosis. Spine. 1997; 22:1741–1746. PMID: 9259785.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download