This article has been
cited by other articles in ScienceCentral.
Abstract
Trigeminal neuralgia (TN) is characterized by recurrent paroxysms of unilateral facial pain that typically is severe, lancinating, and activated with cutaneous stimulation. There are two types of TN, classical TN and atypical TN. The pain nature of classical TN are the same as those described above, whereas atypical TN is characterized by constant, burning pain. We describe the case of a 49-year-old male presenting with right-sided facial pain. The patient was diagnosed with temporomandibular joint disorder at a dental clinic and was on medical treatment, but his symptoms worsened gradually. He was referred to our pain clinic for further evaluation. Radiologic evaluation, including MRI, showed a parapharyngeal tumor. For the relief of TN, a right mandibular nerve (V3) root block was performed at our pain clinic, and then he was scheduled for radiation and chemotherapy.
Go to :

Keywords: parapharyngeal tumor, trigeminal neuralgia, trigeminal neuritis
Trigeminal neuralgia (TN) is a pain syndrome consisting of sharp, lancinating pain in the face nerve distribution. This definition, strictly speaking, applies to classical TN, which is a major form of TN that has an idiopathic pathogenesis. It is thought that classical TN may result from compression of the trigeminal nerve by a blood vessel at or near the root entry zone [
1,
2].
Atypical TN is a rare disorder of the fifth cranial nerve, characterized by facial pain that has a constant or fluctuating timing, with heavy, aching, burning, or boring quality. Its pathogenesis includes head and neck tumors, intracranial infections, and multiple sclerosis, among others [
1,
3].
Although it may be difficult to differentiate between classical and atypical TN, pain clinicians should consider the possibility of atypical TN when the patient's symptoms are described as burning pain rather than lancinating, as this could indicate neuritis. Here, we introduce a case of atypical TN. The patient was transferred to our pain clinic from a dental clinic under the diagnosis of temporomandibular joint disorder, but he was eventually diagnosed with a parapharyngeal squamous cell carcinoma.
CASE REPORT
A 49-year-old male visited our pain clinic with the chief complaint of burning pain and sensory loss in the right temporal area and tongue for the previous 2 months. The pain intensity was 10 out of 10 on the numeric rating scale (NRS). The patient had felt a burning sensation on the tongue, as though tasting something hot, for one year before visiting our clinic. During a previous dental clinic visit, the patient had been diagnosed with temporomandibular joint disorder and put on treatment with daily ibuprofen (2,400 mg). Despite this medical treatment, he did not experience symptom relief. Therefore, the patient was transferred to our pain clinic.
With regard to medical history, the patient had experienced an episode of herpes zoster at the T4 dermatome 10 months earlier. On physical examination, the patient had neuropathic pain and allodynia in the distribution of the right mandibular nerve (V3). Flexion of the neck and compression of the occipital area induced heavy pain in the patient's head and neck, causing an inability to sleep in the supine position. However, there were no vesicles on his skin and no tenderness in the temporal area. The symptoms corresponded with trigeminal neuritis rather than classical TN. Thus, we first diagnosed the patient as having atypical TN and prescribed carbamazepine (CBZ) 100 mg bid, alprazolam 0.25 mg bid, and nortriptyline 10 mg daily. In addition, enhanced MRI was performed to identify the cause of neuritis.
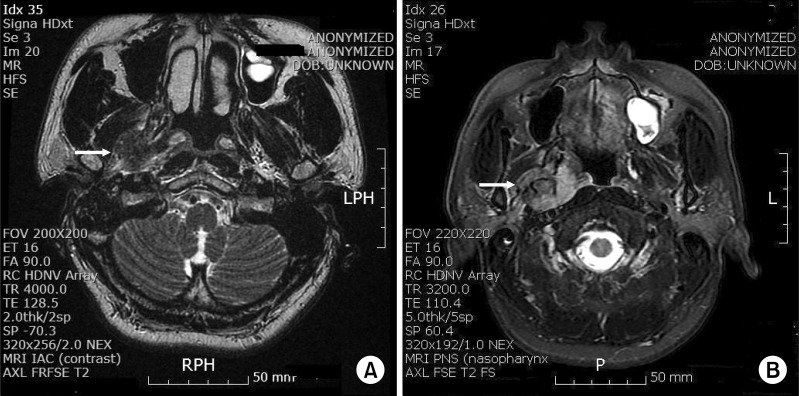
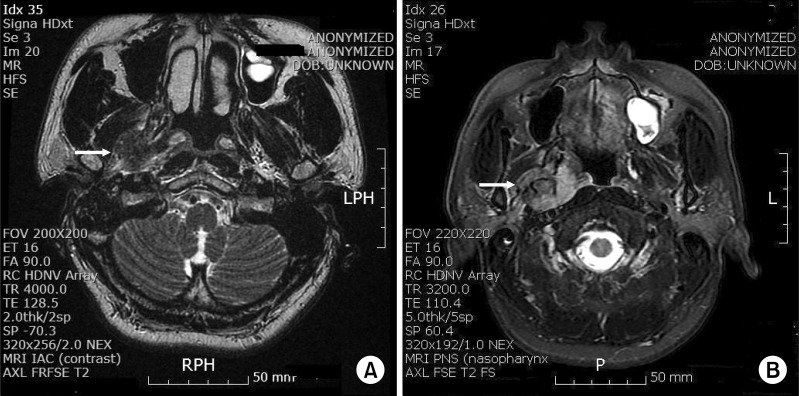
An MRI of the internal auditory canal (IAC) showed a mass in the right parapharyngeal space through the foramen ovale. For further evaluation, an MRI of the paranasal sinus (PNS) with contrast was performed, revealing a 2.3 × 3 × 5.1 cm-sized, ill-defined, heterogeneously enhancing mass in the right parapharyngeal space and the right masticator space (
Fig. 1). We had a high suspicion that the mass was a neurogenic tumor. The whole-body fluorodeoxyglucose (FDG) fusion PET showed suggestive of malignancy in the right parapharyngeal space and the right masticator space, while other areas showed no abnormal FDG uptake suggesting malignancy (
Fig. 2). For the relief of TN, a right V3 root block via an infrazygomatic approach was performed in our pain clinic (
Fig. 3), and then an otolaryngologist performed an endoscopic transpterygoid biopsy for pathologic evaluation.
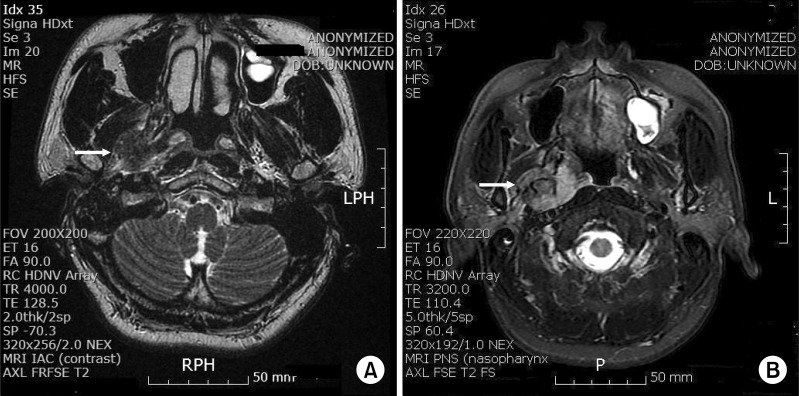 | Fig. 1MRI scan showed a mass (white arrows) in the right parapharyngeal space through foramen ovale. (A) T2 weighted MRI-IAC transverse view. (B) T2 weighted MRI-PNS transverse view. 
|
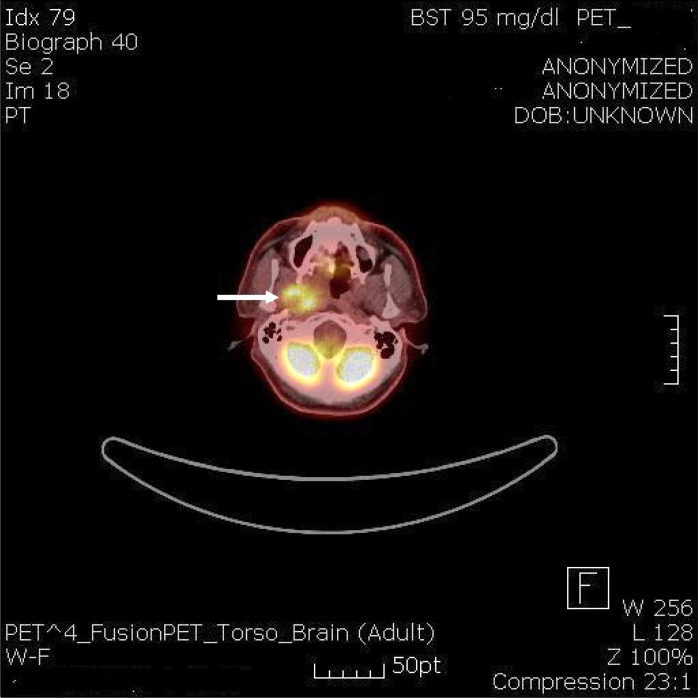 | Fig. 2The whole body FDG fusion PET showed hypermetabloic mass (white arrow), suggestive of malignancy in the right parapharyngeal space and right masticator space. 
|
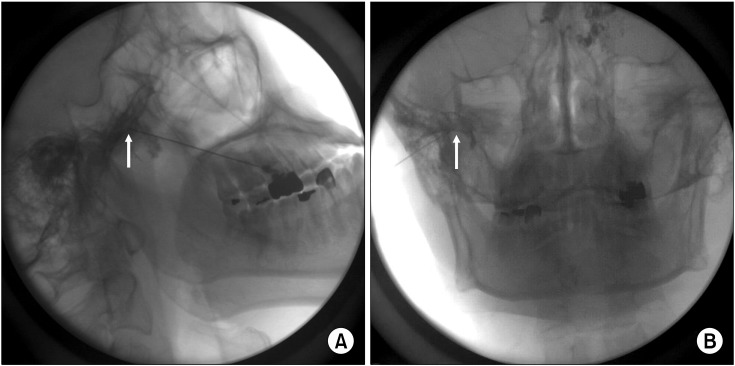 | Fig. 3Right V3 root block via infrazygomatic approach. The needle tip (white arrows) is positioned through foramen ovale. (A) Lateral view. (B) Anteroposterior view. 
|
CBZ was very effective in treating the patient's TN, as the NRS value decreased from 10 to 3. However, a skin rash on the entire body developed suddenly 20 days later, which was thought to have been induced by CBZ. Thus, we stopped CBZ and started the patient on gabapentin 300 mg tid and oxycodone 5 mg tid. After 3 days, the skin rash disappeared, and the pain was well-controlled, with the NRS value maintained at 1 or 2. The patient was scheduled for radiation and chemotherapy.
Go to :

DISCUSSION
TN is a syndrome characterized by unilateral pain in the distribution of one or more branches of the trigeminal nerve. There are two types of TN. One is the well-known classical TN, which causes a sharp, stabbing, or electric-shock-like pain. These attacks may last for several minutes or hours, and pain-free periods between attacks are common, possibly continuing for weeks or even several years [
4]. Although the pathogenesis of classical TN is still unclear, the proposed mechanism is focal demyelination caused by chronic compression and cross excitation between adjacent touch and pain-conducting fibers [
1]. Classical TN can be diagnosed when the pain is of unknown cause and there are no other neurologic problems.
The other type is atypical TN, characterized by pain that is constant, burning, crushing, throbbing, or grinding in nature. These attacks may last for days, weeks, months, or years, and the pain-free periods are absent or of short duration. In addition, such pain can arise without a definite trigger [
3]. Possible causes of atypical TN include cerebral aneurysms, head and neck tumors, multiple sclerosis, and cerebral abscesses, among others. In the case of tumors, especially, the symptoms of atypical TN are similar to neuritis, which are caused by either compressing the nerve directly or eliciting an inflammatory reaction indirectly by the release of its contents. Most of the tumors that are known to lead to the development of TN (acoustic and trigeminal schwannomas, meningiomas, epidermoid cysts, lipomas, and metastases) are generally located in the posterior fossa. The non-specific symptoms of atypical TN make diagnosis of the disorder difficult. Atypical TN can mimic not only classical TN, but also dentoalveolar disease and temporomandibular joint disorder [
5].
In our case, the patient had a tumor in the parapharyngeal space. The parapharyngeal space is located deep within the neck, lateral to the pharynx, and medial to the ramus of the mandible. This is an area of complex anatomy, which is difficult to examine clinically. Tumors of the parapharyngeal space are very rare, accounting for approximately 0.5% of all head and neck tumors. Therefore, the signs and symptoms of parapharyngeal space neoplasms can be subtle, and clinical evaluations of this space are difficult [
6].
In this patient, several clinical features besides the burning pain led to the suspicion of atypical TN; these were the patient's age, sex, sensory changes, and dermatome of pain. The overall incidence of TN is 12.7 per 100,000 persons per year, but the incidence is lower in men than in women (7.3 versus 17.8 per 100,000 persons per year) and increases rapidly for people in their 70s (25.6 per 100,000 persons per year). The mean age at the diagnosis of TN is 51.5 years [
7]. In a study on cerebellopontine angle epidermoid tumors presenting with TN, epidermoid patients were clinically indistinguishable from patients with classical TN from vascular causes, apart from the fact that symptom onset occurred at a younger age in the former group. Patients' ages at the onset of symptoms (42.95 in epidermoids, 52.51 in classical TN: t-test,
P = 0.0189) were significantly lower among patients with TN who had epidermoids when compared to those with classical TN. In young patients with TN, neuroimaging studies must be performed carefully in order to avoid overlooking small tumors [
8]. The etiology in 80-90% of patients with TN is the compression of the trigeminal nerve at or near the nerve root by an overlying vessel, which results in the demyelination of the trigeminal sensory fibers [
3], whereas the etiology in 5-8% of patients with TN is a brain tumor. Facial pain caused by tumors is often related to neurologic abnormalities, such as sensory changes, loss of reflexes, and constant pain [
9,
10].
In our patient, clinical features that may correspond with the features of atypical TN are male gender, age of 49, sensory changes such as allodynia in the distribution of the right mandibular nerve, and pain in multiple dermatome levels. However, the efficacy of CBZ and the presence of a distinct trigger zone are irrelevant to the features of atypical TN.
In a previous study regarding the differential diagnosis between classical TN and atypical TN, 7 of 50 TN patients (14%) were diagnosed with atypical TN after intracranial tumors were detected by an MRI or CT. The other 43 patients were diagnosed with classical TN. CBZ was effective in 5 (71%) of the atypical TN patients and 40 (93%) of the classical TN patients. Twenty-five (58%) of the classical TN patients and 5 (71%) of the atypical TN patients had a distinct trigger zone. There were no significant differences in the efficacy of CBZ and the presence of a trigger zone between the classical TN and atypical TN patients (
P > 0.05) [
11]. Han et al. reported that CBZ was not at all effective in 23 (11%) of 231 classical TN patients [
12]. In our case, CBZ was very effective, although a distinct trigger zone did not exist. Thus, the efficacy of CBZ and the presence of a distinct trigger zone may not be a diagnostic indicator between classical TN and atypical TN.
In conclusion, the clinical factors leading to suspicion of atypical TN are a constant burning sensation, pain in multiple dermatome levels, sensory deficits, age under 70, and male gender. The more of these features that are present, the higher the suspicion of atypical TN should be. In addition, we should consider not only intracranial tumors, but also parapharyngeal tumors as possible underlying causes of atypical TN.
Go to :