This article has been
cited by other articles in ScienceCentral.
Abstract
Background
C-arm fluoroscope has been widely used to promote more effective pain management; however, unwanted radiation exposure for operators is inevitable. We prospectively investigated the differences in radiation exposure related to collimation in Medial Branch Block (MBB).
Methods
This study was a randomized controlled trial of 62 MBBs at L3, 4 and 5. After the patient was laid in the prone position on the operating table, MBB was conducted and only AP projections of the fluoroscope were used. Based on a concealed random number table, MBB was performed with (collimation group) and without (control group) collimation. The data on the patient's age, height, gender, laterality (right/left), radiation absorbed dose (RAD), exposure time, distance from the center of the field to the operator, and effective dose (ED) at the side of the table and at the operator's chest were collected. The brightness of the fluoroscopic image was evaluated with histogram in Photoshop.
Results
There were no significant differences in age, height, weight, male to female ratio, laterality, time, distance and brightness of fluoroscopic image. The area of the fluoroscopic image with collimation was 67% of the conventional image. The RAD (29.9 ± 13.0, P = 0.001) and the ED at the left chest of the operators (0.53 ± 0.71, P = 0.042) and beside the table (5.69 ± 4.6, P = 0.025) in collimation group were lower than that of the control group (44.6 ± 19.0, 0.97 ± 0.92, and 9.53 ± 8.16), resepectively.
Conclusions
Collimation reduced radiation exposure and maintained the image quality. Therefore, the proper use of collimation will be beneficial to both patients and operators.
Go to :

Keywords: collimation, image quality, radiation absorbed dose, radiation exposure
INTRODUCTION
C-arm fluoroscope is a commonly used equipment for effective pain management; however, operators are unavoidably exposed to ionizing radiation during the procedure [
1-
3]. Therefore, different protective equipment is used and numerous methods to reduce the level of radiation exposure have been introduced [
1-
5]. Among those introduced methods, collimation is known to reduce the levels of radiation exposure for both patients and operators.
Lumbar medial branch block (MBB) does not require as many radiographs as other fluoroscopy-guided blocks and is often operated on both sides. It is easy to compare the left MBB and right MBB. We prospectively investigated the differences in radiation exposure related to collimation in MBBs.
Go to :

MATERIALS AND METHODS
After approval from our institutional review board, a prospective randomized controlled trial of MBB at the L3, 4 and 5 level was carried out. Patients who were over 20 years old and scheduled for lumbar MBB were included in this study. A thorough explanation of collimation was given to the patients, and only the ones who agreed to provide and disclose their personal biographical data information (gender, age, height, and weight) were included in this study.
The patients who did not give their approval or who had severe lumbar scoliosis, lumbar spine fixation, or a history of compression fractures at L4 or 5 were excluded.
For MBB, the patient was laid in the prone position on the operating table and only AP projections of the fluoroscope were used. The height of fluoroscope was adjusted until the operating table was centered between the X-ray generator and the image intensifier. Based on a concealed random number table, MBB was performed with (collimation group) and without (control group) collimation.
In the collimation group, the width of the X-ray field was reduced from 26 cm to 14.5 cm, as shown in
Fig. 1A. The distance between the operating surgeons' chest and the center of the X-ray field was measured when the fluoroscope was in use.
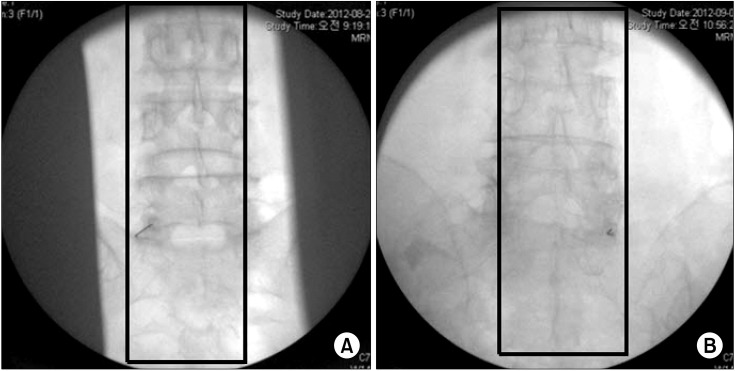 | Fig. 1(A) Fluoroscopic image with collimation in collimation group. (B) Conventional fluoroscopic image in control group. Rectangles: The lumbar spine area was cutted in the fluoroscope pictures to compare the exposure of image using the Photoshop program. The width was trimmed to the same as width of lower L5 body. The height was cut from bottom to top in the circular fluoroscopic image. 
|
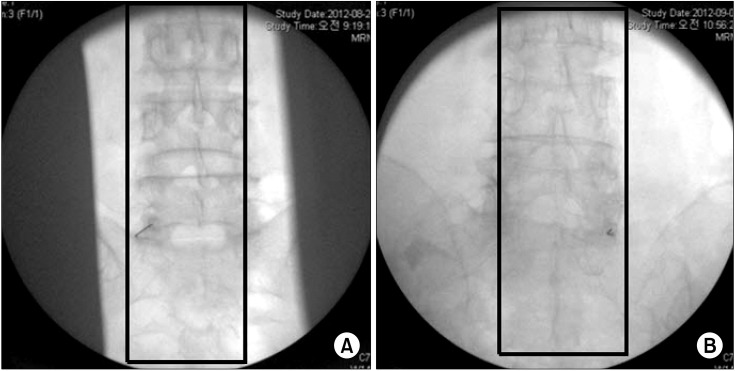
After performing the MBB on the L3, 4 or 5, the radiation absorbed dose (RAD), the exposure time from the fluoroscope and the effective dose (ED) from the dosimeters (one dosimeter [PDM 227, Aloka, Tokyo, Japan] at the side of table and the other one [PDM 127, Aloka, Tokyo, Japan] at the operating surgeon's left chest) were collected (
Fig. 2).
 | Fig. 2(A) Table: effective dose at side of operating table. (B) Body: effective dose at physician's left chest. 
|
To compare the image quality, we investigated whether the operator could see the target point in the fluoroscopic image during the procedures. Additionally, the brightness of the fluoroscopic images was compared. The lumbosacral spine in the fluoroscopic image was cutted shown by the rectangles in
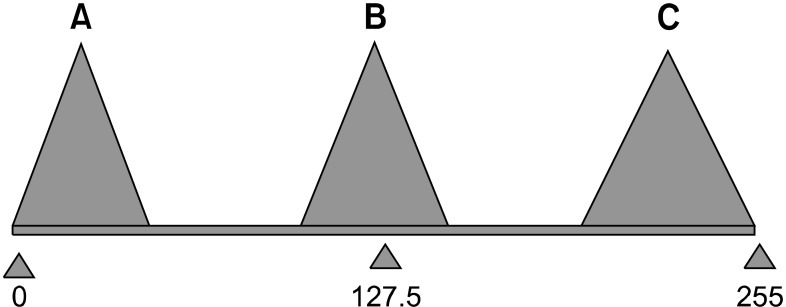
Fig. 1A and B. Then those were compared by obtaining the mean value related to the 256 brightness levels using the histogram function (
Fig. 3) in Photoshop.
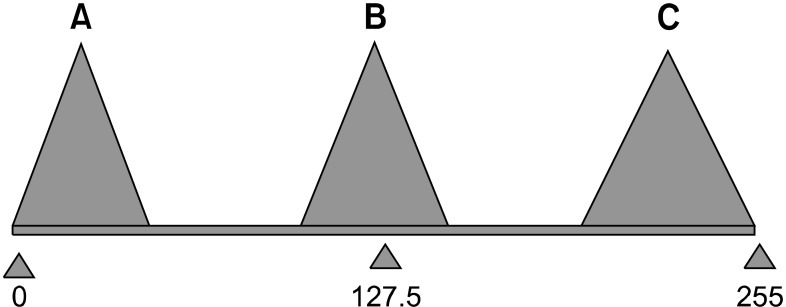 | Fig. 3The figure indicates the histogram on the Photoshop. As the mean value approaches to 0, it indicates the picture was dark, whereas it indicates light when the mean value closes to 255. We assumed that medium value and proper exposure is 127.5. 
|
To investigate the differences between the two groups, age, height, weight, RAD, time of exposure, brightness of fluoroscopic image and ED were analyzed by student T-test. Gender, operation site (left or right) and operator were analyzed by chi - square test. A P < 0.05 was considered to be statistically significant.
Go to :

RESULTS
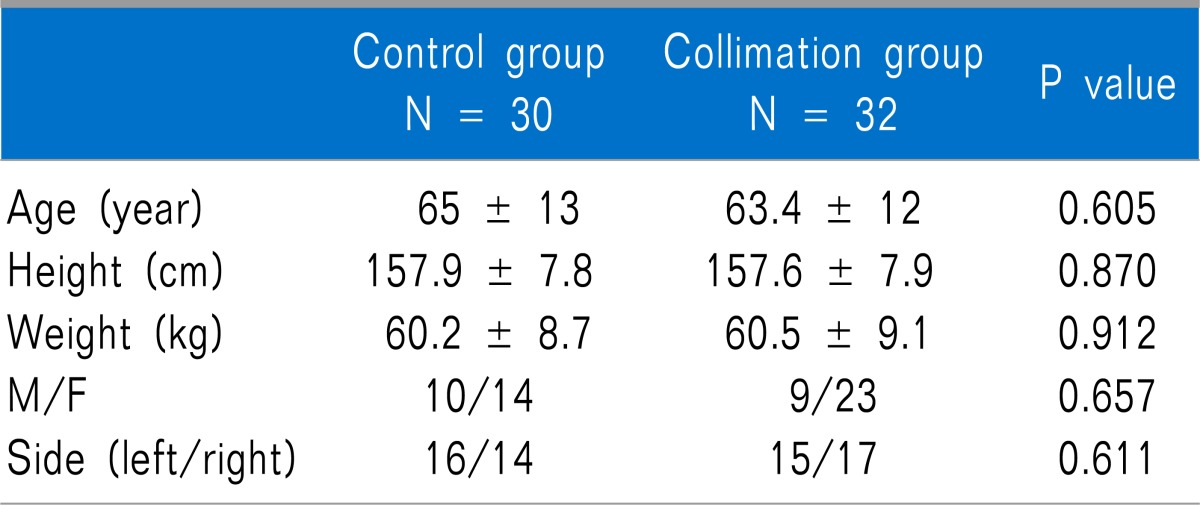
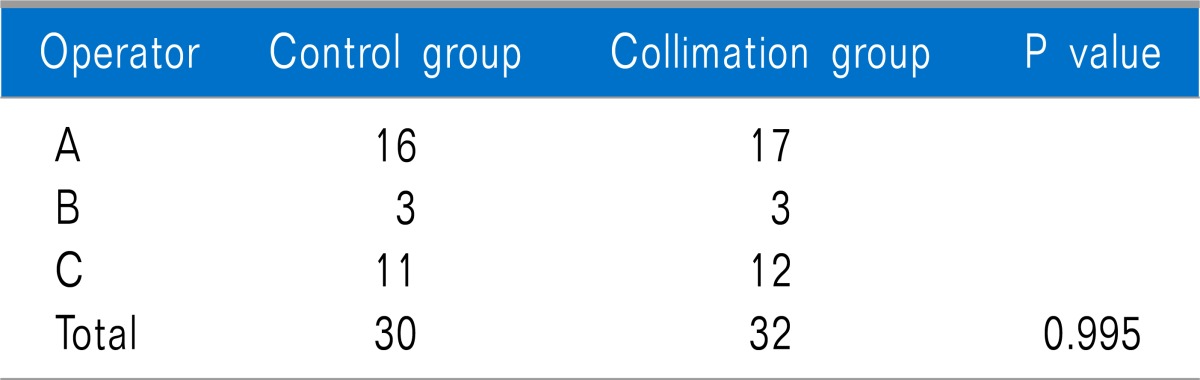
The data were collected from 62 cases of MBB, and the control group had 30 cases while the collimation group had 32 cases.
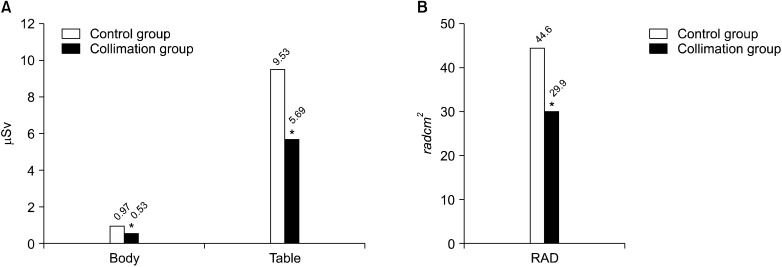
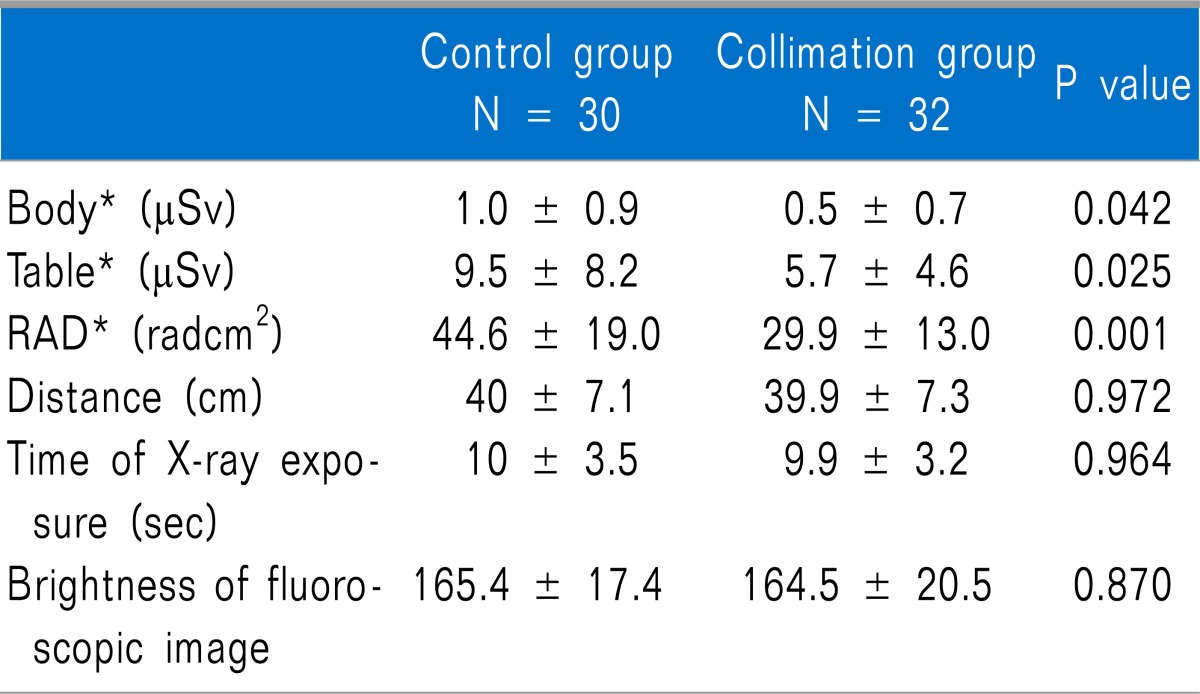
No significant differences were noted in the demographic data such as age, height, weight, male to female ratio, operation site (left or right), operator, distance (40 ± 7.1 cm in the control group vs. 39.9 ± 7.3 cm in the collimation group,
P = 0.972), time of X-ray exposure (10 ± 3.5 sec in the control group vs. 9.9 ± 3.2 sec in the collimation group,
P = 0.964) and the mean value of brightness in the fluoroscopic images (165.4 ± 17.4 in the control group vs. 164.5 ± 20.5 in the collimation group,
P = 0.870) between the two groups (
Tables 1,
2 and
3). In all cases, the operators could easily see the target point in the fluoroscopic image with or without collimation during the procedures. A significant difference was only observed in the RADs and EDs. The RAD (29.9 ± 13.0 radcm
2,
P = 0.001), ED (0.5 ± 0.7 µSv,
P = 0.042) at the operators' chest and ED (5.7 ± 4.6 µSv,
P = 0.025) at the side of the table in the collimation group were lower than that of the control group (44.6 ± 19.0 radcm
2, 1.0 ± 0.9 µSv and 9.5 ± 8.2 µSv, respectively) (
Fig. 4A, B and
Table 3).
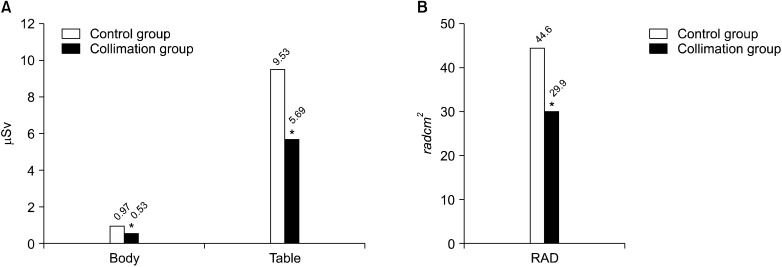 | Fig. 4(A) Comparison between effective dose at left chest of operator, and side of the table, among group. Body: *P value : 0.042, Table : *P value : 0.025. (B) Comparsion of RAD (radiation absorbed dose) between control group and collimation group. 
|
Table 1
Demographic Data of Control Group and Collimation Group
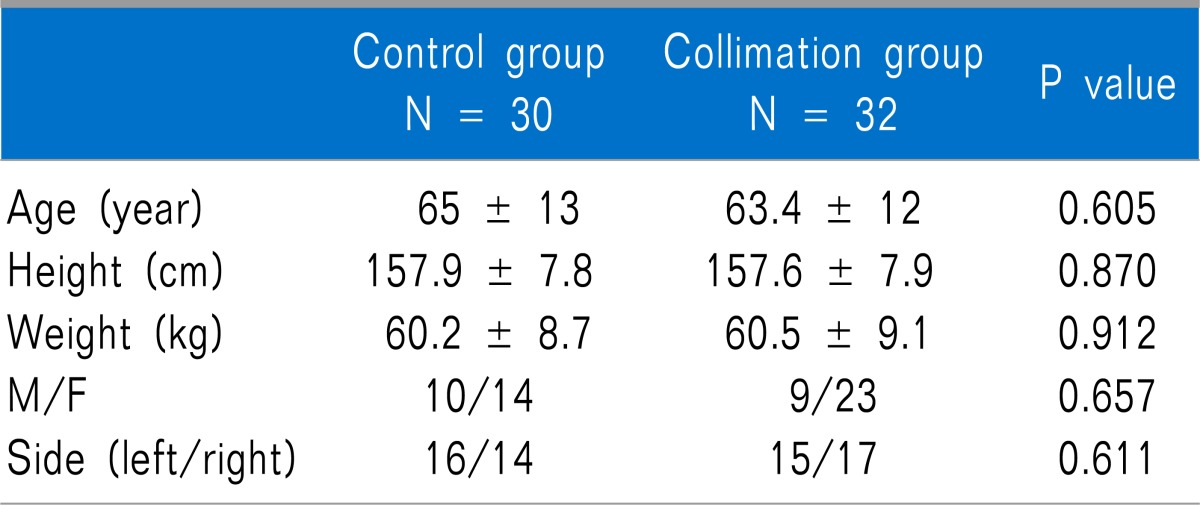

Table 2
The Numbers of MBB Which Each Physician Performed in Each Group
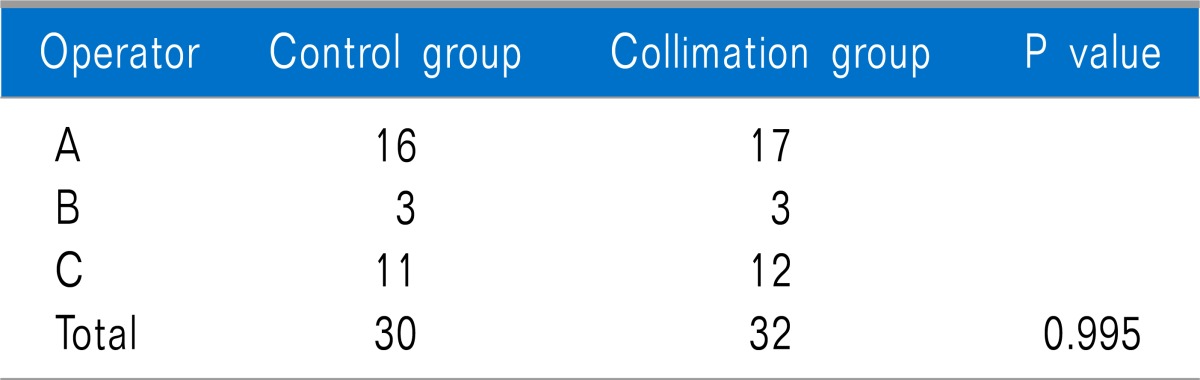

Table 3
Comparisons Between Control Group and Collimation Group
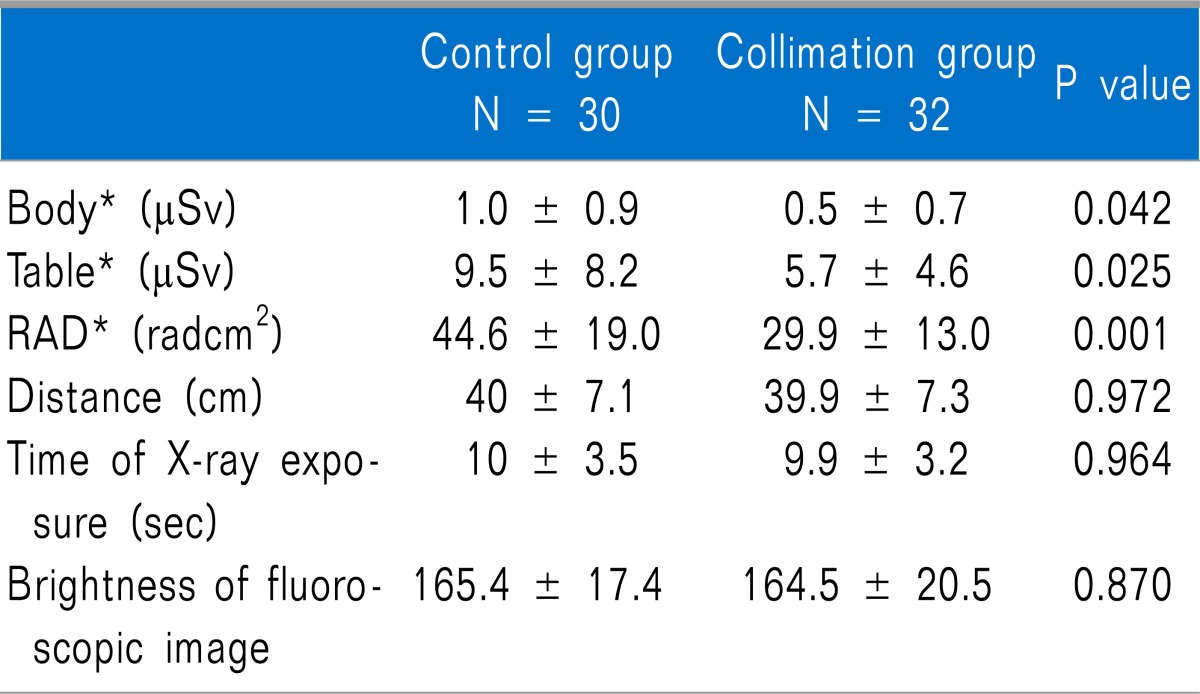

At the monitor, the area of the X-ray field without collimation was 530 cm2 whereas the area of the X-ray field with collimation was 355 cm2.
Go to :

DISCUSSION
Most radiation to which pain physicians are exposed does not result from the primary beam but from scattered radiation reflected off the floor and the patient [
1,
3]. Therefore, it is important to reduce patients' exposure to radiation for the safety of not only patients but also physicians [
6]. Furthermore, numerous methods have been attempted to reduce the level of radiation exposure. Among these, shielding through collimation has also been introduced. The cardinal principles of radiation protection are as follows: (A) maximize the distance from the radiation source; (B) use shielding materials; (C) minimize exposure time; (D) use pulsed fluoroscopy; (E) minimize the use of magnification; (F) wear personal dosimeters to measure the cumulative dose of practitioners; and (G) use the last image-hold function instead of taking a spot-photo to prevent additional radiation exposure when the test (or inspection) does not require any high-resolution photo. The use of collimation also reduces unnecessary radiation exposure [
7,
8]. A decreased X-ray field from collimation reduces the overall integral dose to the patient, and thus minimizes the radiation risk of the patient and physician [
9]. When clinicians do not need detailed image quality such as MBB, they can use the pulsed and low-dose modes together to reduce the radiation exposure [
10]. However, the use of pulsed and/or low-dose modes can decrease the image quality. Nevertheless, collimation is helpful in optimizing the image quality [
11]. Therefore, X-ray beam collimation for radiography and fluoroscopy is important for reducing the patient's exposure dose and improving the image quality. The literature suggests that by limiting the field size of the beam, less material interacts with the primary beam, thus reducing the likelihood of secondary scatter radiation arising from beam interactions within and outside of the patient [
11]. The decreased secondary scatter radiation could be related to the improved image quality. A good example is imaging of the thoracic spine, where the large density differences between the spine and the adjacent air-filled lungs can make it difficult to see the bony elements of the spine with any resolution. Linear collimation to limit the field to the spine itself can dramatically improve the image quality. Likewise, imaging of the cervical spine is fraught with the same difficulties when air on either side of the neck is included in the X-ray field. Either liner collimation or circular collimation (
Fig. 5) can be used to limit the field to the area of interest, improving the image quality and reducing the radiation exposure. Modern fluoroscopic units may also allow for better visualization of the image by electronically magnifying smaller areas of interest. Magnification, however, can lead to increased radiation exposure as the system increases output to compensate for losses in gain. To minimize the dose to the patient, the largest field of view, in conjunction with the tightest collimation should be used [
12].
 | Fig. 5Use of adjustable (iris) collimator to limit the field to the area of interest reduces radiation exposure to the patient and improves image resolution by decreasing the range of tissue density included in the image field. 
|
To compare the image quality, we investigated whether the operators could see the target point in the fluoroscopic image and compared the brightness of the fluoroscopic images. During all the MBBs with and without collimation, the operators could easily see the target point in the fluoroscopic image.
Fig. 3 shows the histogram from Photoshop to compare the degree of brightness in the fluoroscopic images. The histogram displays 256 brightness levels, with 0 being pure block and 255 bring pure white. Data points clustered near zero indicate dark pictures (histogram A), while those near 255, the brightest possible tone, indicate bright pictures (histogram C). Thus, the mid-point of 127.5, shown in histogram B, was assumed to be the median value and the proper exposure. According to the results, no significant difference in the brightness of the images was found between the control and collimation groups. To conclude, there was no significant difference in image quality in this study. Although the results could not prove the image quality in the collimation group was higher than that in the control group, there was no significant decreased in image quality for MBBs in the collimation group.
Most fluoroscopes have both liner and circular collimation. Linear collimation employs shutters that can be moved in from either side of the exposure field and are helpful in imaging long and thin structures such as the spine (
Fig. 1A). Circular or "iris" collimation can be helpful when a small, circular area is to be imaged (
Fig. 5). Walters et al. evaluated the impact of collimation of the "minimal required field size" on the clinically significant parameters of radiation exposure. There was a significant 60% reduction in the total radiation dose with collimation of the minimum required visual field [
13]. In this study, we used a 14.5 cm width of collimation because the width easily permitted physicians to see the target point in the L3, 4 and 5 MBBs as shown in
Fig. 1A. The 33% reduced X-ray field in the collimation group resulted in 40.3% reduced RAD at the fluoroscope, 41% reduced ED at side of the table and 46% reduced ED at the operator's chest. Although the ED at the physician's chest for the control group was a low dose for the MBB procedure (
Fig. 4), cumulative exposure over a long time can be dangerous to a physician. Therefore, 46% reduction of exposure with collimation is meaningful and effective for radiation safety.
In conclusion, the use of collimation reduced the radiation exposure to the patient and operator and did not decrease the image quality in MBB compared to the conventional mode. Therefore, the proper use of collimation will be beneficial to both patients and operators.
Go to :





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download