This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Previous studies have shown that if performed without radiographic guidance, the loss of resistance (LOR) technique can result in inaccurate needle placement in up to 30% of lumbar epidural blocks. To date, no study has shown the efficacy of measuring the depth of the posterior complex (ligamentum flavum, epidural space, and posterior dura) ultrasonographically to distinguish true and false LOR.
Methods
40 cervical epidural blocks were performed using the LOR technique and confirmed by epidurograms. Transverse ultrasound images of the C6/7 area were taken before each cervical epidural block, and the distances from the skin to the posterior complex, transverse process, and supraspinous ligament were measured on each ultrasound view. The number of LOR attempts was counted, and the depth of each LOR was measured with a standard ruler. Correlation of false and true positive LOR depth with ultrasonographically measured depth was also statistically analyzed.
Results
76.5% of all cases (26 out of 34) showed false positive LOR. Concordance correlation coefficients between the measured distances on ultrasound (skin to ligamentum flavum) and actual needle depth were 0.8285 on true LOR. Depth of the true positive LOR correlated with height and weight, with a mean of 5.64 ± 1.06 cm, while the mean depth of the false positive LOR was 4.08 ± 1.00 cm.
Conclusions
Ultrasonographic measurement of the ligamentum flavum depth (or posterior complex) preceding cervical epidural block is beneficial in excluding false LOR and increasing success rates of cervical epidural blocks.
Go to :

Keywords: cervical, epidural, ultrasonography
INTRODUCTION
Cervical epidural blocks (CEBs) are widely used to treat acute and chronic pain conditions involving the head, neck, and upper extremities [
1-
3]. But they also carry a risk of rare but serious complications like epidural abscess [
4], epidural hematoma [
5], arachnoiditis [
6] and permanent spinal cord injury [
7]. The proximity of the spinal cord to ligamentum flavumin the cervical region is coupled with smaller cervical epidural spaces as compared with lumbar levels, leading cervical epidural injections to be prone to complications if the procedure is performed blindly.
The risks associated with performing CEBs are higher than those of lumbar epidural blocks. Previous studies have shown that if performed without radiographic guidance, loss of resistance (LOR) technique can result in inaccurate needle placement in up to 30% of lumbar epidural steroid injections [
8]. Anatomic studies have also found high rates of discontinuity of the ligamentum flavum in the cervical region [
9].
Therefore, accurate knowledge of the depth to discriminate false and true loss of resistance may increase success rates of cervical epidural injections. For this reason, some authors recommend the routine use of fluoroscopy for CEBs [
10], but because of cost efficacy and portability, it is rather difficult to apply this technique to all CEBs. Ultrasound imaging for CEBs is also recommended to improve the quality of prepuncture diagnostics for neuraxial analgesia and to reduce the possibility of complications [
11].
To date, no study has examined the accuracy of LOR technique or shown a correlation to true or false positive LOR depth by ultrasonographic guidance using demographic data such as height, weight, and BMI. Also, no study has shown the efficacy of measuring the depth of the posterior complex (ligamentum flavum, epidural space, and posterior dura) ultrasonographically to distinguish true and false LOR. Our goal was to determine whether ultrasonographic measurements of the depth of the posterior complex could exclude false LOR depth, and to evaluate the accuracy and precision of these measurements in relation to the true LOR depth.
Go to :

MATERIALS AND METHODS
Following the guidelines of the local Ethics Committee, written informed consent was obtained for all 40 cervical epidural injections performed through LOR technique and confirmed with epidurograms. Demographic data (sex, age, height, weight, and body mass index) were obtained. Patients with spinal anomalies, infectious diseases, drug allergies, and coagulopathies were excluded from the study.
CEBs were performed on patients in a prone position with neck flexion by placing a pillow under their chest, so that maximal interlaminal space was secured. After palpating the spinous processes of the cervical spine, we marked a needle insertion point at the midpoint of the C6/7 interspace, noting that C7 was the most prominent spinous process.
Transverse ultrasound images of the C6/7 area were taken before each cervical epidural block, and the distance from the skin to the posterior complex (US-lf), transverse process (US-trans), and supraspinous ligament (US-spin) were measured on each ultrasound view using a 2-5 MHz curved array probe (M-Turbo® SonoSite, Inc.) (
Fig. 1). All ultrasound examinations were performed by one pain physician.
 | Fig. 1Transverse ultrasonographic image at the level of C6-7. Each number indicates supraspinous ligament (1), transverse process (2), ligament flavum (3), posterior dura (4), anterior complex (anterior dura, posterior longitudinal ligament, vertebral body)(5). 
|
Using a fluoroscopic anteroposterior (AP) view, the desired cervical interlaminar space was located. After anesthetizing the skin with 1% lidocaine, a 22-gauge Touhy needle was inserted using a coaxial (tunneled) view just lateral to the midline (ipsilateral to the patient's symptoms), so that it was aligned with the lateral border of the spinous process. During advancement of the needle, AP images were taken as needed to ensure the continuation of a true coaxial view. In all instances, the epidural space was located by using loss of resistance to air. The number of LOR technique attempts was counted, and the depth of each LOR was measured with a standard ruler. After LOR was encountered, accuracy of needle placement was assessed through the injection of 0.5 ml of Iopamiro® contrast medium. AP, lateral, and oblique fluoroscopic views were obtained. Fluoroscopic imaging was performed each time with injection of contrast medium, and the type of pattern of contrast medium spread was documented, whether it was true LOR (epidural pattern) or false LOR (non-epidural or muscular pattern) (
Fig. 2). In the event that the physician was not satisfied that the contrast medium spread was consistent with epidural injection, the needle was repositioned and the process was repeated until adequate contrast medium spread was obtained. When the needle was confirmed to be in the epidural space, a total of 1 ml of contrast medium was injected into the epidural space. AP and lateral radiographs were taken.
 | Fig. 2Lateral fluroscopic images of cervical epidural block at the level of C6-7. Note that the contrast medium spread show non-epidural pattern (A) and epidural pattern (B) on a same patient. 
|
Descriptive statistics were calculated using means and standard deviations for continuous data and percentages for discrete variables. Bland-Altman analysis was performed to determine the magnitude of the difference between the ultrasonographic measurements and LOR depths. We used concordance correlation coefficients (CCC) to evaluate agreement between ultrasonographic measurement and depth of LOR. CCCs provide sound intuitive interpretations because they include components of both precision (degree of variation) and accuracy (degree of location or scale shift). Statistical calculations were performed using MedCalc software 9.3.6.0 (MedCalc Inc., Mariakerke, Belgium).
Go to :

RESULTS
Table 1 summarizes the demographic data of 34 out of 40 patients. 6 patients were excluded because we could not obtain their complete data due to patients' refusals or personal situations.
Table 1
Demographic Data of the Patients


76.5% of all cases (26 out of 34) showed false positive LOR once. There were no ultrasonographically undetectable cases, but the ligamentum flavum was distinguishable from the posterior dura in only 4 cases. In the other 30 cases, ultrasonographic depth to the ligamentum flavum was measured to the posterior aspect of the detectable posterior complex.
True positive LOR showed a mean depth of 5.64 ± 1.06 cm, while the mean depth of false positive LOR was 4.08 ± 1.00 cm (
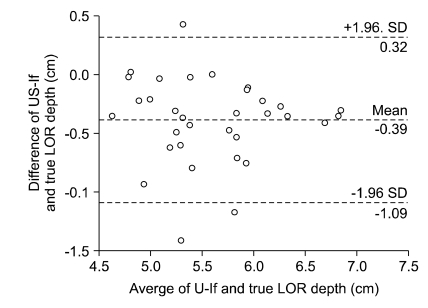
Table 2). Bland-Altman analysis between US-lf and true LOR depth indicated a mean difference of ± 1.96 SD with -0.39 ± 0.7 cm (
Fig. 3). Bland-Altman analysis between US-trans and false LOR depth indicated a mean difference of ± 1.96 SD with +0.43 ± 0.7 cm. Compensated with means of difference calculated by Bland-Altman plot, US-lf showed high CCC and accuracy with compensated depth of true LOR (CCC = 0.8285, 95% CI: 0.6814-0.9113, accuracy 0.9996), but low CCC and accuracy with false LOR (CCC = 0.4444, 95% CI: 0.2498-0.6045, accuracy 0.5510) respectively (
Table 3,
Fig. 4).
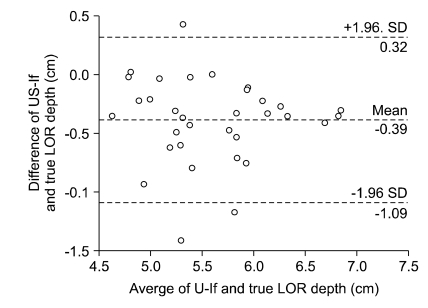 | Fig. 3Bland-Altman precision analysis of the measured differences between ultrasound-measured depth of skin to ligamentum flavum and depth of true loss of. LOR: loss of resistance, US-lf: measured depth from skin to ligamentum flavum or posterior complex. 
|
 | Fig. 4Concordance correlation between ultrasound-measured depth of skin to ligament flavum and depth of compensated true loss of resistance. LOR: loss of resistance, US-lf: measured depth from skin to ligament flavum or posterior complex. 
|
Table 2
Measured Depth of Positive LORs and Ultrasonographic Findings


Table 3
Agreement Between Ultrasonographic Depth and Depth of True and False Loss of Resistance


Depth of true and false positive LOR showed a tendency to correlate linearly with the demographic data, such as height and weight, but this tendency was not statistically significant (P > 0.05).
Go to :

DISCUSSION
Based on our results, the expected true LOR depth can be predicted from the ultrasound views within a range of ± 0.7 cm by Bland-Altman analysis. More importantly, a high CCC for compensated LOR depth and mean value of difference between true and false LOR depth [0.43 cm - (-0.39 cm) = 0.82 cm] implies that ultrasound provides accurate information for distinguishing true and false LOR in cervical spinal regions.
We can conclude that ultrasonographic depth of the posterior complex and transverse process can be useful to identify whether the positive LOR is true or false. Cervical epidural blocks are widely used not only in pain clinics for the management of a variety of acute, chronic, and cancer-related pain syndromes involving the face, head, and upper extremities, but also in the field of anesthesiology. In clinical practice, the most commonly used technique for identifying the epidural space is the loss of resistance to air or saline (LOR) technique. Cervical epidural injections are also often performed in a "blind" manner, such as by using LOR technique at outpatient pain clinic.
A high rate of false LOR (76.5%) was observed in this study. It is higher than that seen in previous studies involving the lumbar region [
8] and even higher than the rate previously observed in the cervical region [
10]. This may be mainly because of the anatomy, such as the discontinuity of the ligamentum flavum in the cervical level [
9]. This finding is supported by the fact that the rate of false LOR in patients who underwent previous laminectomy is much higher than that in surgery-free patients [
10]. The LOR failure rate for the placement of lumbar epidural catheters has been shown to be less than 10% [
12,
13].
The act of inserting an epidural catheter and the size of the needle may also be possible explanations for the higher incidence of false positive LOR rates in cervical epidural blocks [
10]. However, there are no or limited studies exploring these causes.
This high rate of false LOR explains the restrictive effect of cervical epidural blocks which are performed solely using LOR technique without any other information about the depth of the neuraxial structures. Because of the potentially dangerous complications of cervical epidural block [
4-
7], physicians who encounter false LOR cannot easily advance the epidural needle toward the epidural space when CEBs are performed in a "blind'" manner. Therefore, they make the injections into the wrong space and, this restricts their effect.
Accurate information regarding the depth of true loss of resistance may increases safety and success rates, while other imaging methods to provide guidance such as fluoroscopy, MRI, and ultrasound are helpful in accurate needle placement during such procedures.
Stojanovic et al. have reported that loss of resistance technique is a poor tool for locating the epidural space in cervical epidural steroid injection if used without fluoroscopic guidance [
10]. They suggest that fluoroscopy and epidurography can improve the accuracy of needle placement and medication delivery to targeted areas of pathology in cervical epidural steroid injections. However, it is difficult to apply these techniques to all outpatient pain clinics because equipment for fluoroscopy is expensive and poorly portable. Ultrasonography can be a good alternative for this reason.
At the level of the lumbar spine, the correlation between ultrasound-measured depth and actual needle insertion depth has been evaluated in multiple studies [
14-
20]. At the level of the thoracic and cervical spine, visualization of the epidural space is much more difficult than that in the lumbar spine but there are a few studies that have been published about the clinical utility of the ultrasound-guided neuraxial technique [
11,
21,
22]. Correlation was excellent in all studies (Pearson correlation coefficients, 0.80-0.99), whether measurements were made in the sagittal, oblique, or transverse views. Even if the vertebral canal is not clearly visible, a preprocedural ultrasonographic scan may provide sound information for accurate epidural needle depth.
Therefore ultrasonographic measurement of the ligamentum flavum depth (or posterior complex) preceding cervical epidural injection is beneficial in excluding false LOR and increasing success rates of cervical epidural injections. Loss of resistance technique alone may not be adequate for confirming the cervical epidural space because of the high rate of false positive loss of resistance.
Go to :






 PDF
PDF Citation
Citation Print
Print







 XML Download
XML Download