This article has been
cited by other articles in ScienceCentral.
Abstract
Lumbar spinal stenosis is a commonly treated with epidural injections of local anesthetics and corticosteroids, however, these therapies may relieve leg pain for weeks to months but do not influence functional status. Furthermore, the majority of patients report no substantial symptom change over the repeated treatment. Utilizing balloon catheters, we successfully treated with three patients who complained persistent symptoms despite repeated conventional steroid injections. Our results suggest that transforaminal decompression using a balloon catheter may have potential in the nonsurgical treatment of spinal stenosis by modifying the underlying pathophysiology.
Go to :

Keywords: decompressive neuroplasty, epidural injection, spinal stenosis
Lumbar spinal stenosis is a common condition in older adults that causes pain in the lower back and extremities, impairs walking, and results in other types of disability. The majority of symptomatic patients managed non-operatively report no substantial change over the course of 1 year [
1,
2], and epidural injections of steroids may relieve leg pain for weeks to months but do not influence functional status [
3-
5]. Utilizing Fogarty balloon catheters to decompress the intervertebral foramen, we successfully treated spinal stenosis in patients with persistent symptoms despite repeated conventional steroid injections.
CASE REPORT
1. Patient 1
An 82-year-old male, a retired teacher, presented as an outpatient with pains in his lower back and radiating down his left leg in the distribution of L4, 5 dermatome, as well as tingling sensation in the affected region. He rated his leg pain as 8 of 10 and his back pain as 3 of 10. He had a 15-year history of symptoms, which became aggravated over the previous year. His leg pain resulted in a moderate impairment of activities of daily living, and his functional score on the Oswestry Disability Index was 38%. Physical examination showed mild left lower extremity weakness, and motor strength testing revealed 4+/5 in left quadriceps and tibialis anterior muscle, suggesting pain-induced reduction of strength. His sensations to light touch and pin prick were normal, his straight leg rising test results were negative, and his dorsalis pedis and tibial arterial pulsation were normal. Although he previously had no limitations in walking, he had recently experienced leg pain after walking for more than five minutes, with relief of pain after sitting or bending forward. His lumbar x-rays showed Grade I retrolisthesis at L1-2-3-4-5 and a multiple old compression fracture at L2, L3, and L4. He had been treated with Celebrex® (200 mg/day) and Ultracet® (325 mg acetaminophen plus 37.5 mg tramadol), a durogesic patch (25 µg/hr), and repeated epidural steroid injections (seven injections of caudal and/or transforaminal epidural blockers). Despite these injections and a further increase in analgesic dosage, he complained of persistent symptoms, with only 10-20% improvement over 1-2 weeks, and there were no improvements in functional status and walking distance.
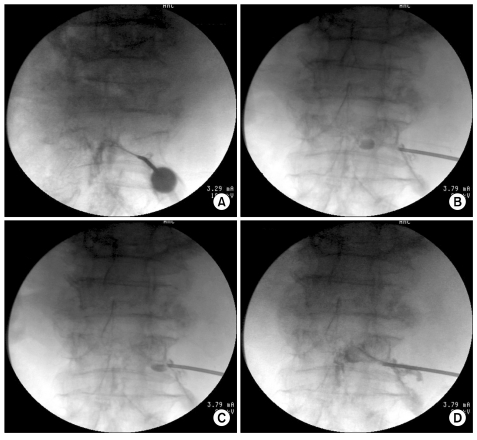
After obtaining IRB approval and written informed consent from the patient, we performed a transforaminal balloon decompression procedure to alleviate his radicular pain and to extend the duration of pain relief. The patient was placed in the prone position, and a pillow was placed under his abdomen to minimize lumbar lordosis. After sterile preparation of the surgical field, an 18 G R-K needle (Epimed International, Gloversville, USA) was introduced into the L5 intervertebral foramen, and its tip was confirmed as being in the anterior epidural space by injection of contrast medium (
Fig. 1). Fluoroscopy was used to visualize the target during the procedure. A 3 Fr Fogarty catheter (Edward Lifescience, Irvine, CA, USA) filled with contrast medium was introduced into the epidural space of the L5 inter-vertebral foramen, and placed in the medial portion of the stenotic area. The needle was slightly withdrawn, and repeated balloon decompression and deballooning were performed throughout the affected region, from the lateral recess to the dural sleeve, with each ballooning session lasting less than 5 seconds. L4 intervertebral transforaminal decompression was also performed in the same manner. After removing the Fogarty catheter, the R-K needle was reinserted and then 3 mL of a mixture of 0.8% lidocaine, 20 mg triamcinolone, and 1,500 IU of hyaluronidase was administered. There were no complications such as bleeding or pain throughout the procedure. After the procedure, however, the patient complained of pain for three days. For the next 15 weeks, the patient reported markedly reduced leg pain (2-3/10), improved functional status (20-26%) and increased claudication distance (40 minutes). Beginning 16 weeks after treatment, his symptoms recurred, but were more tolerable than those before the treatment.
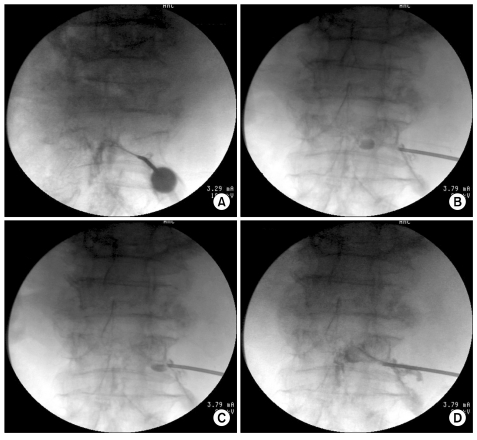 | Fig. 1Serial images of balloon decompressive foraminoplasty using a 3 Fr Fogarty catheter filled with contrast medium. (A) A needle was placed in the L4 intervertebral foramen and contrast medium was injected to confirm the epidural space. The contrast agent spread to the sleeve region in a slit-like pattern. (B, C) Balloon decompression was serially performed along with intervertebral neural foramen. (D) After balloon decompression, the spread pattern of contrast agent appeared wider, suggesting that perineural adhesiolysis had been achieved. 
|
2. Patient 2
A 65-year-old male, a farmer, presented with pains in his lower back and right leg in the distribution of L5 dermatome. He had a medical history of well controlled hypertension and gout. His symptoms had started 6 months earlier, but had become aggravated over the previous month. His pain score was 7/10 and his Oswestry Disability Index was 42%. Physical examination showed no weakness in his lower extremities, normal reactions to light touch and pin prick, and normal arterial pulsations. His claudication distance was about ten minutes. A lumbar MRI scan for back pain one month earlier showed bilateral foraminal stenosis, L4-5 and L5-S1, due to disc protrusion and bulging discs of the entire lumbar spine. He had been treated with meloxicam 7.5 mg/day and repeated epidural steroid injections (4 injections of interlaminar and/or transforaminal epidural blockers), but the effects of this treatment persisted for only one month. We performed a transforaminal balloon decompression procedure, as described above. A 3 Fr Fogarty catheter was introduced into the epidural space of his right L5 intervertebral foramen, followed by serial balloon decompression. After removal of the Fogarty catheter, he was administered 3 mL of a mixture of 0.8% lidocaine, 20 mg triamcinolone, and 1,500 IU of hyaluronidase. There were no complications throughout the procedure. Over the next 24 weeks, the patient reported no leg pain (0/10), markedly improved functional status (4-8%) and increased claudication distance (no limitation to walking).
3. Patient 3
A 77-year-old male, a retired soldier, presented with pain in his lower back, radiating down his right leg in the distribution of L4 dermatome and his left leg in L4, 5 dermatome. He had a 3-year history of symptoms, which became aggravated during the previous three months. He rated his leg pain as 9/10 and his back pain as 4/10. The pain disturbed his sleep, and his Oswestry Disability Index was 52%. Motor strength testing showed 4/5 in both quadriceps and tibialis anterior muscles, suggesting pain-induced reduction of strength. He had a tingling sensation and numbness in his lateral calf and experienced leg pain after walking more than 10 m, making him unable to go to the bathroom in his house. A lumbar MRI scan for back pain two years earlier showed degenerative spondylolisthesis of L4 on L5, causing severe central stenosis, with the cross-sectional area of his dural sac at the narrowest point being 40.4 mm2. Lumbar MRI also showed stenosis of both lateral recesses and both neural foramens, as well as retrolisthesis of L5 on S1 with disc bulging and facet arthrosis causing left neural foraminal stenosis. He had been treated with Opalmon® 15 mg/day, Lyrica® 150 mg/day, Ultracet® and a fentanyl patch (25 µg/hour), and had received 17 epidural steroid injections of transforaminal epidural blockers and decompressive neuroplasty. Despite these injections and a further increase in analgesic dosage, he reported no improvements in pain and functional status. He was not indicated for surgery because of his poor general condition, but was regarded as a candidate for spinal cord stimulation. We elected to perform a transforaminal balloon decompression procedure. A 3 Fr Fogarty catheter was introduced into epidural space of the left L4, L5 and the right L4 intervertebral foramen, and balloon decompression and drug administration were performed serially. There were no complications throughout the procedure. Over the next 24 weeks, the patient reported moderately reduced leg pain (3-4/10), improved functional status (38-40%) and increased claudication distance (70 m).
Go to :

DISCUSSION
Although little is known regarding the nonoperative management of spinal stenosis, conservative treatment usually includes physical therapy, NSAIDs, muscle relaxants and/or mild narcotics, as needed by individual patients. In addition, local anesthetics and corticosteroids are usually administered to relieve symptoms of persistent pain. Although lumbar epidural corticosteroid injections have not consistently shown efficacy, they may relieve pain in patients with symptoms resulting from inflammation at the interface between the nerve root and the compressing tissues [
6]. Epidural injection of steroids is thought to reduce inflammatory edema of the injured nerve root and thus improve intraneural blood flow [
7], decrease sensitization of the dorsal horn neurons and suppress the transmission of nociceptive C-fibers [
8,
9]. Local anesthetics induce sympathetic nerve blockade and vasodilation, thereby improving blood flow to the ischemic neural element [
10,
11]. Co-administration of hyaluronidase has also been used to enhance the effect of lysis of epidural adhesion [
12].
Epidural injection of steroids and local anesthetics in patients with spinal stenosis has been shown to result in only short-lived improvements in pain and function, because the symptoms of spinal stenosis reflect a combination of pathological processes caused by space occupying lesions or fibrosis, such as interruption of blood flow, venous congestion, ischemia, axonal damage and intraneural fibrosis [
13]. Since serial injections of conventional epidural steroids into our three patients did not result in symptom relief, we utilized an alternative technique focused on resolving the underlying pathophysiology of spinal stenosis, consisting of percutaneous epidural foraminoplasty with 3 Fr Fogarty catheters, balloon decompression of the epidural space of the intervertebral foramina, and administration of drugs to the target region. Fogarty catheters were initially utilized in thrombectomy to remove fresh, soft emboli and thrombi from arteries and veins. Using its pliable distal tip, designed to minimize trauma to the venous valves, to manipulate around perineural structures enables a relatively safe procedure. Instead of inflating with air, however, we used contrast medium, enabling visualization of ballooning and de-ballooning during the procedure.
Several factors may be responsible for post-decompression pain relief and functional improvement in our patients. For example, balloon distension of the epidural space may result in effective mechanical detachment of perineural adhesion, which may play a role in restoring the mobility of the nerve roots to some extent, thus contributing to long-term symptom relief. Moreover, mechanical ballooning of a narrow intervertebral foramen may reduce venous congestion and mechanical irritation. Venous congestion has been regarded essential in precipitating circulatory disturbance, thus inducing neurogenic claudication [
14]. Furthermore, initial improvements of symptoms after the decompressive procedure may be due to local anesthetics and steroids that reach the areas causing these symptoms. Balloon dilatation and adhesiolysis, however, may also contribute to the effective delivery of epidural injections to regions of spinal stenosis, thereby improving the effects of drugs in these target lesions [
15].
We found that balloon decompression did not yield consistent results in our patients, which may be due to differences in disease severity and/or physical condition. Patient one achieved 4 months of modest symptom relief, whereas Patient two had 6 months symptom-free. Patient three showed incomplete improvement, but this seemed acceptable because this patient was considered a candidate for a spinal cord stimulator. Additional studies involving more patients are needed to establish the proper criteria for selecting patients for balloon decompression.
Patient safety should also be considered in the effects of acute compression on spinal nerves. Increasing pressure and its duration have been found to induce more pronounced effects such as intraneural edema [
16]. The safe limits of nerve compression in vivo have not been established, however, transforaminal balloon decompression would be regarded as safe if the balloon pressure is increased slowly and the procedure is limited to less than 2-4 h [
17,
18].
There have been previous attempt to use various balloon catheter for epidural adhesiolysis in patients with failed back surgery syndrome [
19]. To our knowledge, however, this is the first report describing the use of epidural balloon catheters to decompress the intervertebral foraminal space in the treatment of patients with spinal stenosis. Over the past several years, minimally invasive surgical techniques have been introduced, using smaller incisions and more limited removal of the innate structure, to achieve decompression. Although our case series provides only anecdotal evidence, the results suggest that transforaminal decompression using a balloon may have potential in the nonsurgical treatment of this condition by modifying the underlying pathophysiology of segmental stenosis. Ongoing randomized controlled trials with larger sample sizes will address the effects of this treatment on pain improvement, functional score and claudication distance.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download