This article has been
cited by other articles in ScienceCentral.
Abstract
The superior hypogastric plexus block (SHPB) is used for treating pelvic pain, especially in patients with gynecological malignancies. Various approaches to this procedure have been reported due to the anatomic obstacles of a high iliac crest or large transverse process of the 5th lumbar vertebra. Here, we report a new technique of superior hypogastric plexus block using a unilateral single-needle approach to block the bilateral superior hypogastric plexus with a Tuohy needle and epidural catheter. We have confidence that this new technique can be another option in performing the SHPB when the conventional bilateral approach is difficult to perform.
Go to :

Keywords: catheter, hypogastric plexus, nerve block, pain
In patients with pelvic cancer pain, the pelvic pain is severe, which makes it difficult to treat, as well as lowering the quality of life of the patient. Administration of opioids orally or intravenously can reduce the pain, but can frequently cause systemic side effects, so pain control is not easy. In such cases, nerve blocks can minimize systemic side effects while decreasing pain, so this technique is used commonly in patients with cancer pain. In particular, the superior hypogastric plexus block (SHPB) is commonly performed to reduce pain in the pelvic area [
1].
Since the introduction of the traditional SHPB in 1990 by Plancarte et al. [
1], various methods of approach have been attempted. The reason for such various methods is that approach is difficult due to anatomical barriers such as the nerve root, iliac artery and vein, iliac crest, and transverse process of the L5 vertebra. In addition, in patients complaining of cancer pain, approaching the superior hypogastric plexus is not easy because of invasion of the cancer into surrounding tissue as well as metastasis into other viscera [
2]. Approach under computed tomography (CT) has been attempted, and this method provides accurate images, but also has its drawbacks, including the amount of time and equipment required, as well as the significant level of radiation exposure for the performing surgeon [
3,
4]. Recently the transdiscal approach has been attempted, but despite the easy approach, there is the possibility of serious complications such as disc infection or disc rupture [
5,
6]. For these reasons the traditional approach is still mainly used.
The authors of the study discussed here had a patient with severe pelvic pain due to ovarian cancer, so SHPB through the traditional method was performed. During the procedure, approach was difficult because the right transverse process of the L5 vertebra and the iliac crest were in contact. Therefore, we used a unilateral single-needle approach with an epidural catheter and successfully performed the SHPB. Thus we are reporting this case.
CASE REPORT
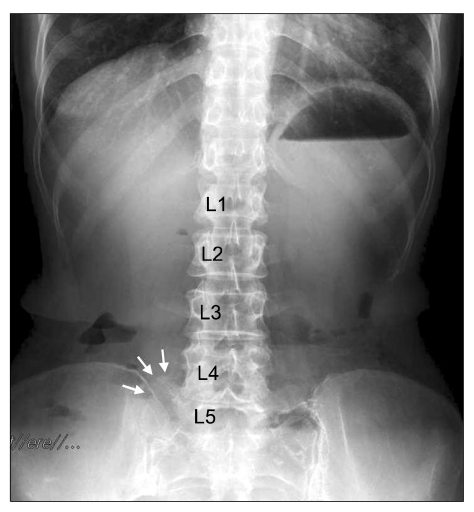
A 60-year-old female patient with a height of 150 cm and weight of 42 kg visited the pain clinic for continuous pelvic and coccyx pain which began simultaneously with multiple metastases 8 months earlier. The patient had been diagnosed with ovarian cancer 5 years previously and had undergone transabdominal hysterectomy and bilateral salpingo-oophorectomy. At the time of her visit, metastases to the lung, spleen, and peritoneum were observed, but there was no evidence of bone metastasis. The patient complained of splitting pain of the perianal area which continued for about 2 hours 3 times a day, on average, and of dull pelvic pain. The visual analogue scale (VAS) score was 9/10 and worsened during coughing or the Valsalva maneuver, and eased with standing or walking. Ultracet® 3 T/day and nortriptyline 10 mg/day were administered as drug treatment, and a caudal block was performed for pain control. The patient's pudendal pain had decreased, but she complained of continuous pelvic pain, so an additional SHPB was planned. During the procedure, the patient was placed in the prone position and a pillow was propped beneath her lower abdomen to decrease the lumbar lordosis. After checking the lumbar 4-5 intervertebral space with C-arm fluoroscopy, the skin was disinfected with betadine. Local anesthesia was performed using 1% lidocaine at a skin insertion point 5 cm to the right of the midline. Using a 15 cm, 22 G Chiba needle (Cook Medical Inc., Bloomington, IN, USA), we attempted to insert the needle at a 45 degree angle medioinferiorly, avoiding the transverse process of the L5 vertebra. However, the transverse process of the L5 vertebra and the iliac crest were in contact due to degenerative changes, so needle insertion failed (
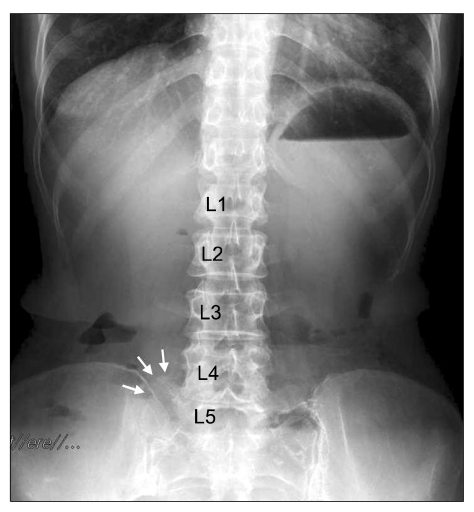
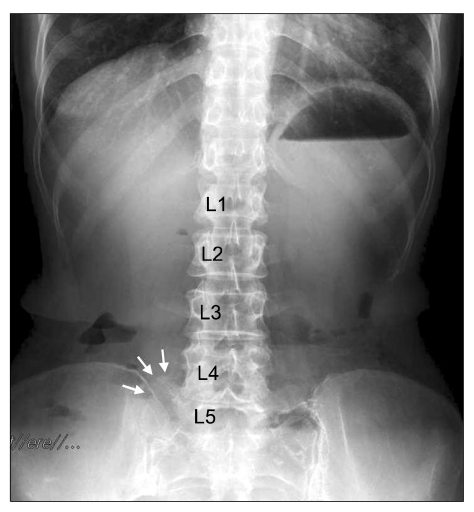
Fig. 1). Therefore, we decided to perform bilateral SHPB by inserting a catheter through the left superior hypogastric plexus. After checking the lumbar 4-5 intervertebral space through C-arm fluoroscopy, local anesthesia was performed using 1% lidocaine with at a skin insertion point 5 cm from the left of the midline. Then an 8 cm, 18 G epidural needle (Perican®, B-Braun Inc., Melsungen, Germany) was inserted and positioned. When the epidural catheter (Perifix®, B-Braun Inc., Melsungen, Germany) was inserted, a slight resistance was felt. It was similar to the resistance felt when inserting an epidural catheter through an epidural needle. Therefore, we advanced the epidural catheter approximately 3 cm farther from the epidural needle tip. Then, 2 ml of contrast media (Omnipaque300®) was injected, and after verifying the adequate spread of the contrast media, 0.38% ropivacaine 8 cc was injected (
Fig. 2,
3). After the procedure, the patient reported reduced pelvic pain, with a VAS score of 3/10, so three days later SHPB was performed by the same method. After confirming that there was no motor nerve loss, 6 ml of 99% dehydrated ethanol was injected, followed by 0.5 ml of normal saline to inject all the alcohol left in the catheter, and the catheter was removed. The patient's pain improved to 3/10 on the VAS without complications, and she was discharged.
 | Fig. 1Simple X-ray of the lumbar spine. The enlarged right L5 transverse process can be identified (arrows). 
|
 | Fig. 2Unilateral, single-needle approach to perform the superior hypogastric plexus block. A catheter is inserted through the Tuohy needle. 
|
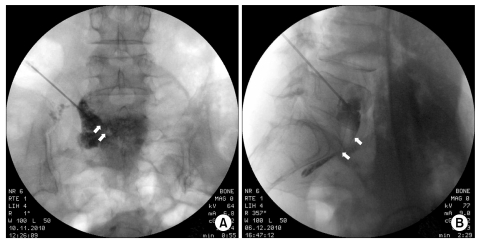 | Fig. 3AP (A) and lateral views (B) of fluoroscopic X-ray of left unilateral approach. Radio-opaque dye spread from the left margin of L5 vertebral body to the right margin in the retroperitoneal space. The arrows indicate the epidural catheter tip at the level of the upper margin of the sacrum. 
|
Go to :

DISCUSSION
There are many known methods of approach for SHPB. Plancarte et al. first introduced the traditional method of fluoroscopic-guided bilateral posterior approach in 1990 [
1]. However, there are cases where approach is difficult, and for a more accurate approach than simple fluoroscopy, Waldman et al. performed a CT-guided unilateral posterior approach in 1991 [
3]. Afterwards, Kanazi et al. performed a CT-guided unilateral anterior approach in 1999 [
4], and Ina et al. [
5] performed a posterior paramedian transintervertebral disc approach in 1996. Turker et al. performed SHPB through a posterior median transintervertebral disc approach [
6]. Each of these various methods of approach had its advantages and disadvantages. The traditional method of Plancarte et al. is similar to the existing celiac plexus block performed by Moore [
1]. The disadvantages of this method are that it needs to be performed with two needles, it is difficult to avoid contact with the transverse process of the lumbar vertebra, and it is not easy to position the needle in the accurate position [
1]. Despite these disadvantages, this traditional method is still the most widely used. Walder's approach method, which uses only one needle, is performed under CT guidance, so the patient and medical staff are not free from the risk of exposure to radiation [
3]. Kanazi's CT-guided unilateral anterior approach is liable to damage the colon, bladder, and surrounding vessels [
4]. The posterior median transintervertebral disc approach has the advantage that it can be performed in the lateral position for patients unable to be in the prone position [
6]. However, the transintervertebral disc approach used by Ina and Turker carries the small possibility of causing severe complications such as disc infection and disc rupture [
5,
6]. Hence, thorough sterilization of the skin before the procedure is necessary, along with the preventive use of broad-spectrum antibiotics [
6]. When performing the procedure through the traditional method was difficult, however, SHPB has been successfully performed through the transintervertebral disc approach [
2]. The reason for such various methods of approach is that there are many cases in which approach is anatomically difficult.
SHPB can be used as one of the methods to reduce analgesic complications by reducing the required amount of opioids for control of pain due to pelvic cancer. This pain is not limited to the terminal stages of cancer, so when SHPB is used aggressively from the early stages, it may improve the quality of the patient's remaining life [
7]. When performing SHPB as an aggressive pain control method for pelvic cancer pain, the performing surgeon needs to remember that there are various approach methods and select the most suitable method for each patient for a successful block.
The new attempt of the authors discussed here uses the same approach method as the traditional Plancarte method, but it is different in that bilateral SHPB can be successfully performed using only one needle. Of course there are disadvantages to this method, as it can be difficult to reach the appropriate location when inserting the catheter, and there is the possibility of tissue injury due to the use of a thicker needle for the insertion of the catheter. However, the method discussed here is one of the methods that can be attempted when bilateral approach is difficult because of anatomical barriers due to degenerative changes, such as in our case. Many advantages can be considered, such as reducing the frequency of pain from surgery compared to the bilateral approach, reducing the risk of complications such as disc infection or disc rupture compared to the transintervertebral disc approach, reducing the risk of damaging other viscera compared to the anterior approach, and reducing the performing surgeon's exposure to radiation compared to the CT-guided approach. The authors' method can be difficult to use in obese patients. However, patients in the terminal stages of cancer are generally cachexic, such as in our case (body mass index = 18.6), so bilateral SHPB can be performed with a single-needle technique using the epidural catheter. A long Tuohy needle is also available on the market, so this method can even be used in obese patients, for whom the regular Tuohy needle is too short.
In conclusion, a unilateral approach using the epidural catheter is an effective method that can be considered when performing a bilateral SHPB in patients with anatomical barriers due to degenerative changes.
Go to :