Abstract
The pain around the posterior knee, called 'popliteal fossa', has been known to be caused by a variety of disease entities. Venous malformation is a very rare cause of popliteal area pain, and its diagnosis is frequently delayed, missed, or given incorrectly. Here, we report a case of a patient with popliteal fossa pain for 2 years and was diagnosed as intramuscular venous malformation using ultrasound.
Popliteal fossa pain is developed by a wide variety of causes. The most common causes are Baker's cyst, soft tissue or bone tumor and injury to the meniscus, hamstring, popliteal tendon or ligament. However, neurological causes such as entrapment of the common peroneal nerve or tibial nerve and vascular causes like popliteal artery entrapment or vascular malformation are less common causes of pain [1]. Here, the authors report a case of a patient who could not be diagnosed and treated appropriately for 2 years and was finally correctly diagnosed as intramuscular venous malformation in our clinic.
A 24-year-old female patient visited our pain clinic with the chief complaint of right popliteal fossa area pain and intermittent swelling for 2 years. There was no history of trauma or any other known medico-surgical history. Although she had visited many local clinics for 2 years, she could not be diagnosed properly. In addition, the medications and physical therapy from different local clinics did not help to improve her symptoms. The pain became worse when she changed her position from sitting to standing, with characteristics like sharp pricking, pulling and picking. The severe pain was rated 6 to 8 on the visual analogue scale (VAS). Sometimes, soft tissue swelling was accompanied with pain in affected area.
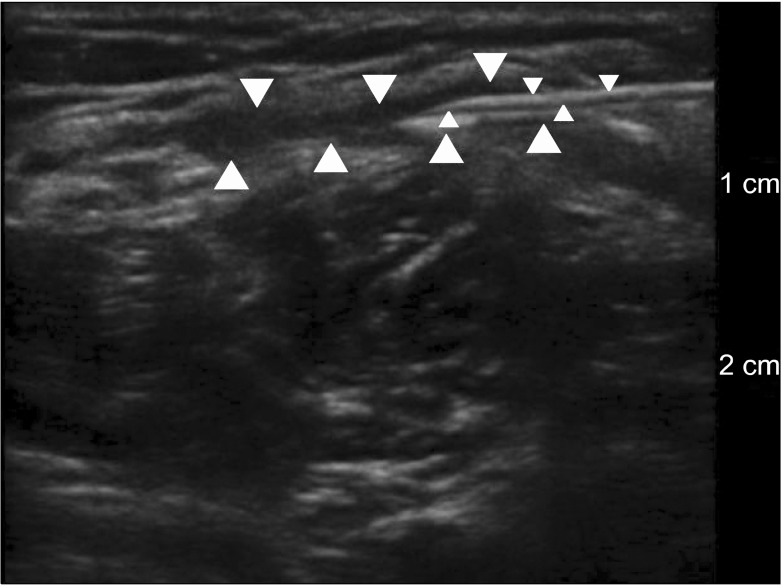
After ultrasound (S-nerve, Sonosite®, Bothell, WA, USA) scanning in the standing position, a compressible hypoechoic fluid collection pocket with a diameter thickness of 0.5 cm was found between the subcutaneous tissue and gastrocnemius muscle in the right popliteal area. Then, we tried to aspirate the fluid under ultrasound guidance; venous-blood like fluid was aspirated continuously but the pocket did not collapse (Fig. 1). Thus, we suspected that the fluid collection pocket was related to a vascular anomaly; therefore, we decided to perform computed tomography venogram.
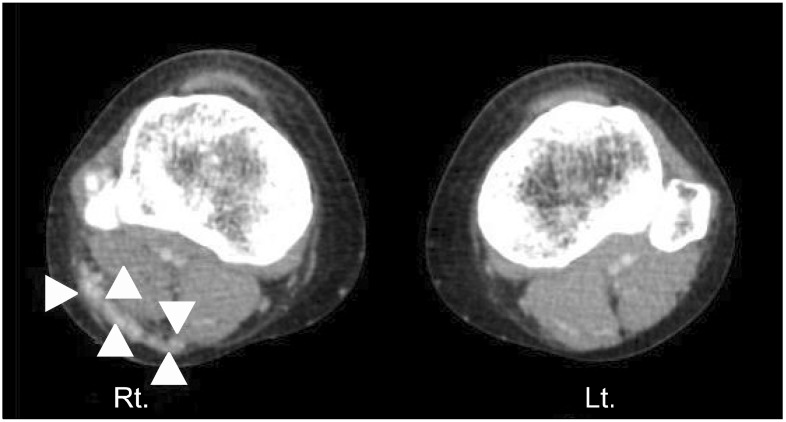
The official reading of the radiologist was that there was a venous malformation between the superficial fascia and gastrocnemius muscle of the right popliteal fossa (Fig. 2). Thus, we referred the patient to the vascular surgery department. The patient was referred to the department of radiology again where she received sclerotherapy with sodium tetradecyl sulfate.
The patient has been in a symptom free state for 6 weeks after the sclerotherapy and has been followed-up by the radiology department.
Venous malformations are known to be one of the rare causes of knee pain. The total prevalence of venous malformations is approximately 1 in 5,000 to 10,000 childbirths [2]. Among these, venous malformations are the most common vascular anomalies of the limbs and account for approximately one-half to two-thirds of all venous malformations [3]. In a recent study, it was reported that women are more commonly affected than men (64%) [4] and that most of the patients are young people [5]. The pain is more commonly associated with the involvement of the lower limbs than the upper ones, and is related frequently to muscle involvement, thrombosis and hamartoma [3]. Furthermore, when the knee joint is invaded by venous malformation, functional limitation, hemarthrosis, and arthropathy are accompanied with the pain [3]. Hypertrophic changes of the musculo-skeletal systems in the affected site are uncommon; however, most of the cases have a tendency to have normal, atrophic or hypotrophic changes [3]. Although, among venous malformations of the limbs, the incidence of knee venous malformation is unknown as this entity is rare [5]. Therefore, a patient who visits a clinic with popliteal pain can be misdiagnosed if the clinician does not suspect the possibility of venous malformations of knee. Particularly, if there are accompanying symptoms or signs like lower limb edema or swelling when in the standing position and skin color change with pain around the knee joint, it is necessary for the clinician to consider knee venous malformation.
Ultrasound is an easily accessible non-invasive screening tool to diagnosis venous malformation within the popliteal fossa, and CT and MRI can be used as confirmative imaging tests for the diagnosis [3,5-7].
In this case, we were able to diagnose and treat the cause of intractable popliteal fossa pain that had been occurring for 2 years. If patients visit a pain clinic with the chief complaint of popliteal pain, the possibility of venous malformation of knee should be considered along with other common causes such as musculoskeletal disease, cysts, and soft tissue or bone tumors.
References
1. Muché JA, Lento PH. Posterior knee pain and its causes: a clinician's guide to expediting diagnosis. Phys Sportsmed. 2004; 32:23–30.
2. Vikkula M, Boon LM, Mulliken JB. Molecular genetics of vascular malformations. Matrix Biol. 2001; 20:327–335. PMID: 11566267.

3. Redondo P, Aguado L, Martínez-Cuesta A. Diagnosis and management of extensive vascular malformations of the lower limb: part I. Clinical diagnosis. J Am Acad Dermatol. 2011; 65:893–906. PMID: 22000870.

4. Mazoyer E, Enjolras O, Bisdorff A, Perdu J, Wassef M, Drouet L. Coagulation disorders in patients with venous malformation of the limbs and trunk: a case series of 118 patients. Arch Dermatol. 2008; 144:861–867. PMID: 18645137.
5. Tsai A, Chaudry G, Spencer S, Kasser JR, Alomari AI. Misdiagnosis of knee venous malformation as juvenile idiopathic arthritis. J Pediatr Orthop. 2011; 31:683–690. PMID: 21841446.

6. Theruvil B, Kapoor V, Thalava R, Nag HL, Kotwal PP. Vascular malformations in muscles around the knee presenting as knee pain. Knee. 2004; 11:155–158. PMID: 15066631.

7. Rogalski R, Hensinger R, Loder R. Vascular abnormalities of the extremities: clinical findings and management. J Pediatr Orthop. 1993; 13:9–14. PMID: 8416363.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download