Abstract
Posterior neck pain is a common complaint of patients in the pain clinic. The atlas (C1) burst fracture is known to be a cause of posterior neck pain and instability. Although the atlas burst fracture and instability can be discovered by plain X-rays which show lateral mass displacement or widening of the atlantodental interval, assessment of an atlas burst fracture can be difficult if there is no instability in the imaging study. Here we report a case of a 46-year-old female patient who had complained of sustained posterior neck pain for 6 months. Plain X-rays showed only disc space narrowing at C4/5 and C5/6, without any cervical instability. However, an unrecognized C1 lateral mass fracture was detected by CT and MRI. The patient's pain was then successfully treated after atlantoaxial joint injection with a C2 DRG block.
Go to : 
The atlas, the first cervical vertebra (C1), is a crucial component of the craniocervical junction or upper cervical spine. C1 has a unique ring shape, which allows it the greatest range of motion and flexibility among the levels of the spinal column [1]. Its flexibility produces unique complicated fractures when coupled with traumatic force vectors acting in flexion, extension, compression, distraction, or in combination [1]. Atlas fractures can also be accompanied by disruption of the transverse ligament, which plays a critical role in determining atlantoaxial stability. Transverse ligamentous disruption has been implicated as the most crucial pathological abnormality responsible for atlantoaxial instability [2,3].
It is difficult to assess atlas fractures with or without disruption of the transverse ligament using only plain X-rays. On lateral views, the atlantodental interval reflects its physiological integrity. The open-mouth view shows the possibility of ligament rupture and instability in C1 fractures. However, these plain radiographs reveal only indirect information about atlas fractures and transverse ligamentous disruption. Computerized tomography (CT) is the optimal imaging modality to assess atlas fractures, but this method is insufficient to demonstrate the integrity of the transverse ligament [1,2].
Here we report a case of a 46-year-old female patient who had complained of sustained posterior neck pain for 6 months. Plain X-rays revealed only disc space narrowing at C4/5 and C5/6, without any cervical instability. An unrecognized C1 lateral mass fracture was detected by CT and MRI, however, and the patient's pain was successfully treated after atlantoaxial joint injection with a C2 DRG block.
A 46-year-old female patient visited our hospital with pain in the right posterior neck area, which had continued since she had fallen from a chair six months previously. She said that she had fallen down from a chair with small wheels in her house at the time of the accident. The patient had a history of undergoing medical treatment for rheumatoid arthritis. The degree of pain was 8/10 on the visual analog scale (VAS), and the pain was localized mainly in the right posterior neck and occipital area. The patient reported a twinge of pain and paresthesia at rest. The pain was aggravated by head rotation or flexion. Jackson's compression test was positive and Spurling's test was positive on the right side. There were no relieving factors. Biceps, triceps, and brachioradialis tendon reflexes were normal.
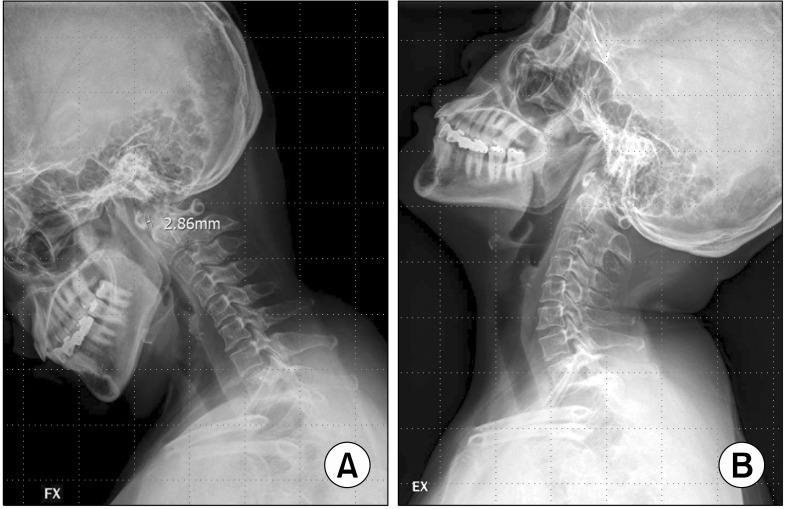
On lateral flexion-extension views of plain X-rays (Fig. 1), there was narrowing of the disc spaces at the C4/5 and C5/6 levels. There was no sign of atlantoaxial instability, however, because the atlantodental interval (ADI) was 2.86 mm. Therefore, the patient's pain was considered to be caused by a cervical herniated intervertebral disc and of myofascial origin, so a greater occipital nerve block, trigger point injection, and cervical epidural block were performed. However, these treatments were ineffective for her pain.
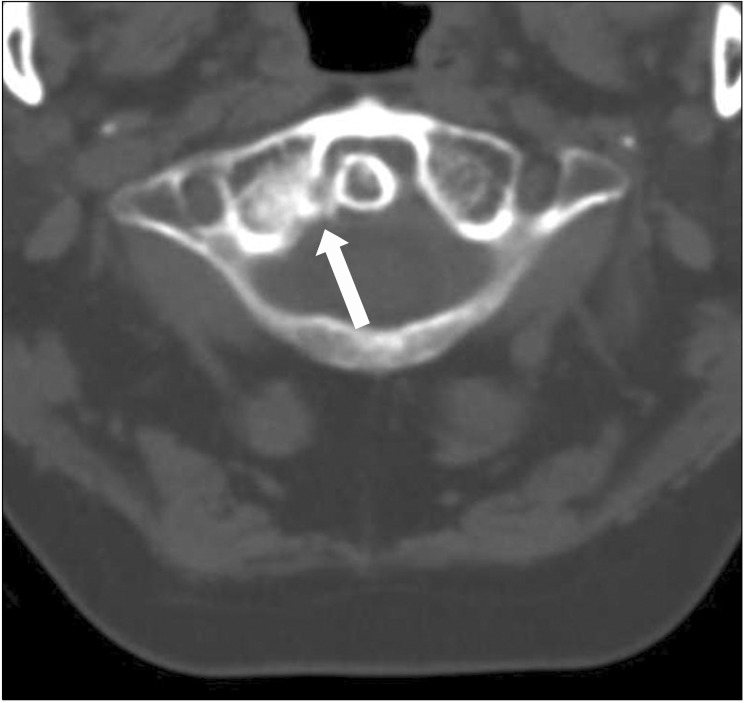
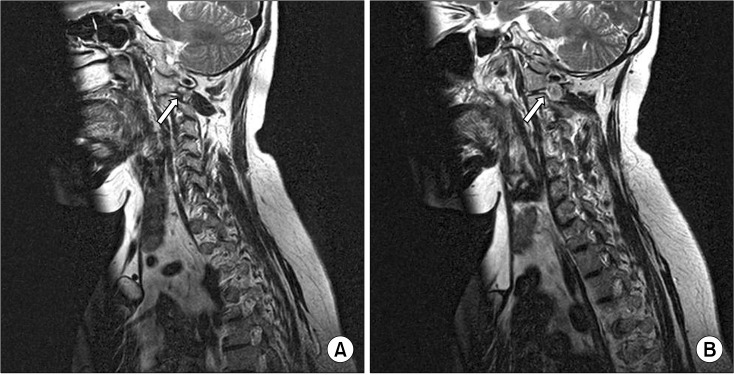
Considering the patient's medical history of rheumatoid arthritis, we performed an open-mouth odontoid view on plain radiograph and a CT of the cervical spine for evaluation of the C1/2 joint, although there was no sign of instability on flexion/extension lateral images. The open-mouth view showed narrowing of the right atlantoaxial joint space, and the CT of the cervical spine showed an old fracture of the lateral mass at C1 and was suspicious for an avulsion injury of the right transverse ligament (Fig. 2). Therefore, atlantoaxial joint injection was performed, after which the patient's pain was improved by 20%. MR imaging additionally revealed right facet subluxation at C1/2 with C2 nerve root compression (Fig. 3). Therefore, an additional right C2 DRG block and C2 pulsed radiofrequency lesioning were performed. As a result, the patient experienced improvement in her pain, down to a VAS score about 3/10.
She reported that the twinge of pain she felt was improved but that head flexion continued to be difficult. We recommended surgical fusion at C1/2, but the patient refused surgery. The patient's current medication regimen is Ultracet® (Janssen Korea, Ltd.) 3 tablets/day, and her pain intensity remains 3/10 on the VAS.
Go to : 
The stability of the craniocervical junction comes from bony structures and the ligaments of the facet capsules of occiput-C1 and C1-C2. Craniocervical instability can result from vertebral fractures or ligamentous injuries caused by trauma.
Atlas fractures occur in 2-13% of cervical spine injuries and represent about 1-2% of all spinal fractures [4]. Since Jefferson first described, in 1920, an anterior and posterior arch fracture of the atlas, there has been no standard classification system of atlas fractures [1]. The classification system modified by Gehweiler distinguishes between isolated and combined arch fractures, lateral mass fractures, and transverse fractures of the anterior arch [1]. Type I fractures involve the posterior arch alone, whereas Type II fractures involve the anterior arch alone. Type III fractures involve bilateral posterior arch fractures related to unilateral or bilateral anterior arch fracture. Type IV fractures involve the lateral mass, and type V fractures are transverse fractures of the anterior arch. According to Landells and Van Peteghem's classification [5], type I fractures involve the anterior or posterior arch alone. Type II fractures involve fractures of both the anterior and posterior arches. Type III fracture is a fracture of the lateral mass with or without a fracture of the arch. The present case would be classified as a Gehweiler type IV, Landells type III fracture involving the lateral mass.
The transverse ligament is the primary and crucial component of atlantoaxial stability, as the largest, thickest, and strongest of the cervical ligaments [1,2]. The transverse ligament is a very firm, inelastic band of tissue, and its injury can occur suddenly when either rapid or slow loading forces are applied [6]. It can rupture in the central portion of the transverse ligament, or it can cause an osteoperiosteal failure at the medial tubercle of the C1 lateral mass [2,6]. Dickman et al. [7] proposed the following classification of transverse ligamentous injuries. They distinguished Type I injuries involving the mid-portion or the insertion point of the transverse ligament and Type II injuries involving avulsion fractures of the tubercle for insertion of the transverse ligament. Type I injuries are incapable of healing with external immobilization, but Type II injuries are capable of healing with only external immobilization. The present case was classified as a Dickman's Type II injury; however, it was incapable of healing with external immobilization because it was an old injury that had happened six months ago.
Patients with fractures of the upper cervical spine mainly complain of neck pain, spasm of the cervical muscles, and limitation of neck motion [1]. Neuralgia and paresthesia also frequently result from compression or injuries of the C2 nerve [8], as in the present case.
To evaluate atlas fractures, it is necessary to obtain lateral, flexion-extension, and open-mouth views on plain X-rays. On lateral flexion-extension views, an ADI greater than 3 mm in adults and greater than 5 mm in children is highly suggestive of disruption of the transverse ligament [1]. On the open-mouth view, displacement of the C1 lateral mass is suggestive of an atlas burst fracture, with displacement greater than 7 mm resulting in instability by transverse ligamentous disruption [2,3]. However, if the ADI is less than 3 mm with fractures of the C1 lateral mass, as inthis case, diagnosis by plain X-ray alone is of limited value. Moreover, plain X-rays are relatively insensitive for detecting injuries of the transverse ligament [1,7]. In this case, computerized tomography is more useful. The cervical CT scan showed clearly the fracture of the C1 lateral mass missed by plain X-rays, known as the best modalities for evaluating osseous abnormalities. However, CT scan is incomplete for visualization of the transverse ligament. Although CT scan is insufficient to demonstrate the anatomy of the transverse ligament [2], axial views on CT scans can detect ligament avulsion fractures, even if the displacement is less than 7 mm [1]. On the other hand, MR imaging can be reliable to obtain visualization of the transverse ligament as well as to evaluate the spinal cord after trauma. MR imaging is highly sensitive fordetection of transverse ligamentous disruption [1], with MR imaging showing the anatomical continuity of the ligament, and abnormal signal intensity revealing ligamentous disruption [2].
In the present case, the posterior neck pain was initially considered to be caused by a herniated cervical intervertebral disc ormyofascial origin, because plain radiographs showed only narrowing of the disc space without C1/2 instability. However, further evaluation by CT scan was performed on the basis of the patient's history of old trauma and rheumatoid arthritis. A cervical CT scan revealed an unrecognized C1 lateral mass fracture and an avulsion fracture of the transverse ligament. Moreover, compression of the C2 nerve root caused by C1/2 facet subluxation was discovered by MR imaging, and proper treatment was therefore possible. In these types of patients, detailed history taking and aggressive imaging assessment are necessary to allow accurate diagnosis and proper treatments. It is most important to assess atlantoaxial stability by CT scan and MR imaging, especially when apatient with a history of trauma complains of occipital neuralgia and has limited range of motion of the cervical spine. Additionally, atlantoaxial joint injection and C2 DRG block can be considered as conservative treatments for atlas fractures.
Go to : 
References
1. Kakarla UK, Chang SW, Theodore N, Sonntag VK. Atlas fractures. Neurosurgery. 2010; 66:60–67. PMID: 20173529.

2. Dickman CA, Mamourian A, Sonntag VK, Drayer BP. Magnetic resonance imaging of the transverse atlantal ligament for the evaluation of atlantoaxial instability. J Neurosurg. 1991; 75:221–227. PMID: 2072158.

3. Spence KF Jr, Decker S, Sell KW. Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg Am. 1970; 52:543–549. PMID: 5425648.

4. Sherk HH, Nicholson JT. Fractures of the atlas. J Bone Joint Surg Am. 1970; 52:1017–1024. PMID: 5479472.

5. Landells CD, Van Peteghem PK. Fractures of the atlas: classification, treatment and morbidity. Spine (Phila Pa 1976). 1988; 13:450–452. PMID: 3187689.
6. Fielding JW, Cochran GB, Lawsing JF 3rd, Hohl M. Tears of the transverse ligament of the atlas. A clinical and biomechanical study. J Bone Joint Surg Am. 1974; 56:1683–1691. PMID: 4434037.
7. Dickman CA, Greene KA, Sonntag VK. Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1996; 38:44–50. PMID: 8747950.

8. Kesterson L, Benzel E, Orrison W, Coleman J. Evaluation and treatment of atlas burst fractures (Jefferson fractures). J Neurosurg. 1991; 75:213–220. PMID: 2072157.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download