Abstract
Tarlov or perineural cysts are nerve root cysts found most commonly at the sacral spine level arising between covering layers of the perineurium and the endoneurium near the dorsal root ganglion and are usually asymptomatic. Symptomatic sacral perineural cysts are uncommon but sometimes require surgical treatment. A 69-year-old male presented with pain in the buttock. He was diagnosed as having a sacral cyst with magnetic resonance imaging. For the nonoperative diagnosis and treatment, caudal peridurography and block were performed. After the treatment, the patient's symptom was relieved. We suggest a caudal peridural block is effective in relieving pain from a sacral cyst.
A perineural cyst is a cyst comprised of the arachnoid membrane of the intradural nerve root, and was first reported by Tarlov in 1938 [1]. Perineural cysts are most common in the sacral area, and are mostly asymptomatic in which coccygodynia or lower back pain occurs in approximately 1% of the cases [1-3]. Symptomatic perineural cysts are treated with conservative treatment such as medication or surgery, and there is debate regarding the effect of the treatment [4,5]. Here, the authors report a case of perineural cyst with symptoms of nerve root compression, which was treated with a caudal epidural block.
A 69-year-old male patient visited the hospital complaining of left sacral pain and radiating pain in the right lower extremities, which had occurred starting 5 years ago. There were no abnormalities in the past medical history of the patient, and the sacral pain had worsened during the last two years and it became more severe when standing or walking for about 10 minutes. The patient was treated in a private hospital but there was no effect so he visited the orthopedics department of our hospital for treatment. The results of the MRI-enhancement showed hypertrophy of the lumbar facet joints, spinal stenosis with thickened yellow ligament between L2-3, L3-4, and L4-5, and a perineural cyst with the dimensions of 1 × 1.1 cm2 in the left S2 area (Fig. 1). The orthopedics department diagnosed the pain as a spinal stenosis so they performed conservative treatment by administering NSAIDs, limaprost, and steroids; however, the pain did not improve so the patient was referred to our department.
When visiting our department, the patient was continually complaining of numbness and stabbing pain in the sacral area of VAS (visual analog scale) 5-6, and complained that the symptoms worsened when standing for about 10 minutes. In addition, when walking for long periods, there was numbness and a pulling pain in the right leg. There were no abnormalities in the straight leg raising test, and there were no other symptoms other than pain in the physical and neurological examination. Since the patient complained of the pain continually and regularly occurring only in the left sacral area and radiating pain occurring in the right, the pain was believed to be caused by a perineural cyst in the S2 area together with the pain caused by the spinal stenosis. In addition, since the patient had received a facet joint block in a previous private hospital with no effect, the possibility of degenerative change such as degenerative arthritis was low. Especially since the chief complaint of the patient was continuous numbness and stabbing pain in the left sacral area, which was coincidental with the location of the perineural cyst according to the dermatome, it was decided for the differential diagnosis to first perform a caudal peridurography to confirm the cyst and perform a caudal epidural block. After having observed changes in the symptoms, treatment for spinal stenosis was supposed to perform.
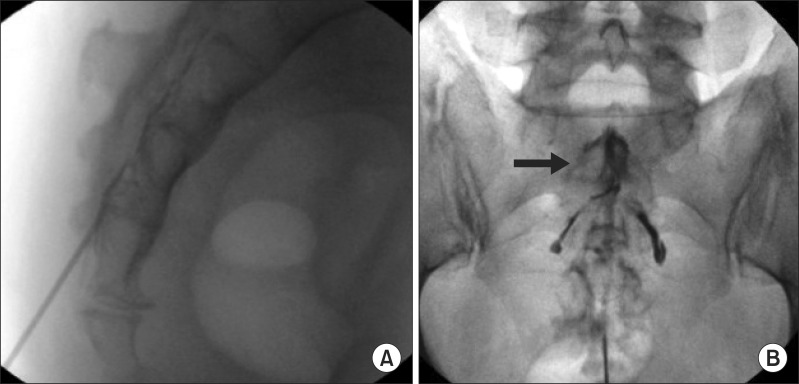
In the operating room, the patient was put in a prone position while showing stable vital signs. Local infiltration was performed with 1% lidocaine on the needle insertion site. With the guidance of a C-arm, a Tuhoy needle was inserted, and contrast medium was injected with continually contrasting of the epidural space. After 3 ml of contrast medium were injected, a perineural cyst was observed so the contrast medium was discontinued (Fig. 2A). The contrast results showed a filling defect of the epidural space caused by a perineural cyst in the left S2 area (Fig. 2B), and 8 ml of 0.75% mepivacaine (Mepivacaine HCl Injection 2% Hana®, Hana Pharm., Korea), triamcinolone acetonide (TAMCETON INJ®, Han All Bio Pharma, Korea) 20 mg, and hyaluronidase (H-LASE®, Kuhnil Pharm., Korea) 1,500 IU were prepared and slowly injected. The C-arm was continually used to confirm the diffusion of the medication, and the medication was inserted while observing that the contrasted area around the cyst became weaker as the contrast medium was diluted by the medication. After injecting 6 ml of medication and the authors felt that the medication had sufficiently spread around the cyst and the injection of medication was discontinued. The medication was injected slowly; thus, it only spread around the perineural cyst and did not spread into the epidural space, and special caution was taken to insert only a small amount of medication so the pressure would not rupture the cyst.
After the procedure, the patient showed improvement in his symptoms with the left sacral pain disappearing and only a slight numbness left. One month after the procedure, the patient again visited the hospital complaining of numbness and radiating pain in the right lower extremities of about VAS 5. According to the physical examination, there was pain in the L5 dermatome; therefore, the pain was suspected to be caused by a spinal stenosis; thus, a selective transforaminal block was performed on the right L5. Afterwards, the radiating pain in the right lower extremities had improved and the patient was able to perform daily activities without discomfort.
Perineural cysts generally have no symptoms; therefore, in many cases, it is discovered by chance while performing CT, MRI, or pain treatment for other reasons [5]. However, there could be symptoms such as radicular pain, sensory abnormality, motor weakness, impotence, and urinary dysfunction depending on several factors such as the cyst's location, size, and association with the nerve root [2,6,7]. Especially when it causes various problems in the anatomy such as pressuring, pulling, or distorting the adjacent nerve root, it can cause radicular pain with various aspects. These symptoms can worsen when the pressure of the cerebrospinal fluid (CSF) increases such as when coughing, the Valsalva maneuver, climbing stairs, and changing position, and can be eased when the patient lies on the opposite side and takes a rest [8-10]. The patient in our case had worse symptoms when standing for about 10 minutes, and this is believed to be from the increase in pressure of CSF to the perineural cyst compared to lying down or sitting.
However, perineural cysts cause symptoms in less than 1% of occurrences, and even when there are symptoms, it is similar to other spinal lesions such as disc herniation, so it is difficult to differentiate with only the symptoms [11]. Therefore, it is better to start treatment considering the possibility of other spinal lesions, and when there is no improvement from the initial treatment of spinal lesions, doctors should consider the possibility of a perineural cyst for their diagnosis and treatment. In our case, the patient had already been diagnosed using MRI images and had been transferred to our department after experiencing no effect for various treatments regarding degenerative facet joint syndrome or spinal stenosis; thus, it was possible to start the diagnosis and treatment related to a perineural cyst right away.
When planning the diagnosis and treatment of a cyst, it is important to decide the association between the imaging findings and the symptoms. When approaching a diagnosis for perineural cysts, it is necessary to differentiate between three circumstances as follows: when another disease is causing the symptoms irrespective of the cyst; when the cyst becomes the secondary cause for the symptoms of another disease, and when the cyst is the only pathologic observation that is causing the symptoms [11]. Especially for disc herniation, intervertebral foraminal stenosis, or spinal stenosis like in our case accompanies a perineural cyst, and it can be hard to differentiate the area in which the lesion is causing the primary symptoms. If surgical treatment is performed first for the accompanying disease and it is not the major lesion causing the symptoms, this can waste time and cause economic loss for the patient. Therefore, it is believed that it is better to actively attempt treatment when a differential diagnosis shows a high association between the location of a cyst and a clinical manifestation [5]. The patient in our case had an accompanying perineural cyst and spinal stenosis; however, in the physical examination, the patient mainly complained of left sacral pain rather than intermittent claudication in the right lower extremities caused by the spinal stenosis. In addition, the patient had shown no improvement from the treatment of spinal stenosis before visiting our hospital; therefore, a perineural cyst was decided to be the main lesion and treatment was first carried out for the cyst. Mitra et al. [4] reported that in patients showing radiculopathy due to a perineural cyst, the pain was immediately eased with one administration of an epidural steroid injection and that the symptoms did not recur for two weeks. The patient in our study also showed immediate improvement in his symptoms with the caudal epidural block and the symptoms did not recur for a month; therefore, the perineural cyst had been the cause for the chief complaint.
Conservative treatment and surgical treatment can be performed for perineural cysts; however, it is unclear which is more effective, and there is still much debate. However, even when surgical treatment is performed, there is no improvement in approximately 28% of patients, and there are reports that it instead causes complications such as CSF leakage, urinary dysfunction, and cerebral hemorrhage [12]. Therefore, there should be caution when selecting surgical treatment and it may be more beneficial for patients when conservative treatments such as epidural block are considered first.
In conclusion, effective improvement in symptoms can be obtained in a patient with a symptomatic perineural cyst by performing a caudal epidural block while being cautious of complications such as a cyst rupture. Thus, an epidural block can be considered as a non-operative treatment of perineural cysts.
References
1. Tarlov IM. Perineural cysts of the spinal nerve roots. Arch Neurol Psychiatry. 1938; 40:1067–1074.
2. Langdown AJ, Grundy JR, Birch NC. The clinical relevance of Tarlov cysts. J Spinal Disord Tech. 2005; 18:29–33. PMID: 15687849.

3. Voyadzis JM, Bhargava P, Henderson FC. Tarlov cysts: a study of 10 cases with review of the literature. J Neurosurg. 2001; 95:25–32. PMID: 11453427.

4. Mitra R, Kirpalani D, Wedemeyer M. Conservative management of perineural cysts. Spine (Phila Pa 1976). 2008; 33:E565–E568. PMID: 18628699.

5. Kang MS, Lim YJ, Lee SC. Sacral meningeal cyst detected during caudal epidural block. J Korean Pain Soc. 1999; 12:258–262.
6. Shao Z, Wang B, Wu Y, Zhang Z, Wu Q, Yang S. CT-guided percutaneous injection of fibrin glue for the therapy of symptomatic arachnoid cysts. Am J Neuroradiol. 2011; 32:1469–1473. PMID: 21835944.

7. Zhang T, Li Z, Gong W, Sun B, Liu S, Zhang K, et al. Percutaneous fibrin glue therapy for meningeal cysts of the sacral spine with or without aspiration of the cerebrospinal fluid. J Neurosurg Spine. 2007; 7:145–150. PMID: 17688053.

8. Ju CI, Shin H, Kim SW, Kim HS. Sacral perineural cyst accompanying disc herniation. J Korean Neurosurg Soc. 2009; 45:185–187. PMID: 19352483.

9. Mummaneni PV, Pitts LH, McCormack BM, Corroo JM, Weinstein PR. Microsurgical treatment of symptomatic sacral Tarlov cysts. Neurosurgery. 2000; 47:74–78. PMID: 10917349.

10. Park HJ, Kim IS, Lee SW, Son BC. Two cases of symptomatic perineural cysts (tarlov cysts) in one family: a case report. J Korean Neurosurg Soc. 2008; 44:174–177. PMID: 19096672.

11. Lucantoni C, Than KD, Wang AC, Valdivia-Valdivia JM, Maher CO, La Marca F, et al. Tarlov cysts: a controversial lesion of the sacral spine. Neurosurg Focus. 2011; 31:E14. PMID: 22133181.

12. Matsumoto H, Matsumoto S, Miki T, Miyaji Y, Minami H, Masuda A, et al. Surgical treatment of sacral perineural cyst-case report. Neurol Med Chir (Tokyo). 2011; 51:867–871. PMID: 22198114.
Fig. 1
T2 weighted MR images show disc bulging and spinal stenosis of L2-3, L3-4, and L4-5 (line) intervertebral spaces (A). Axial view of T2 weighted MR images at L4-5 intervertebral space shows compressed spinal cords due to spinal stenosis (B). Perineural cyst located on the S2 level is typically seen as well circumscribed and ovoid in shape (arrow, C and D). Water density structures of a cyst appear black in T1 weighted MRI (C) and white in T2 weighted MRI (D).





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download