This article has been
cited by other articles in ScienceCentral.
Abstract
Sacral nerve stimulation through the retrograde approach has been used for peroneal or irritable bowel syndrome through the retrograde approach. However, several reasons, lead could not be advanced down ward. In this case, anterograde sacral nerve stimulation through the sacral hiatus could be used. The aim of this report is to present of technique of sacral nerve root stimulation through the sacral hiatus approach.
Go to :

Keywords: anterograde, sacral nerve stimulation, spinal cord stimulation
Spinal cord stimulation (SCS) has been used since 1967 for the treatment of a variety of chronic pain conditions. The two most important conditions amenable to treatment with spinal cord stimulation are neuropathic pain of peripheral origin and ischemic pain in peripheral vascular disease.
Sacral nerve stimulation has been used for peroneal or irritable bowel syndrome through the retrograde approach [
1-
4]. Occasionally, the lead could not be advanced past the area of prior surgery in the lumbar spine region. Here, we report a anterograde sacral nerve stimulation through the sacral hiatus.
TECHNIQUE
Under prone, a Tuohy needle was advanced into the sacral hiatus under fluoroscopy. A percutaneous leads were then passed through the needle and advanced into posterior sacral epidural space (
Fig. 1). After confirming the location of the lead, the Tuohy needles were carefully removed under fluoroscopic guidance to ensure a lack of migration. Then, about a 5 cm incision was then made at the Tuohy needle insertion site and surgical dissection was accomplished (
Fig. 2). For the lead anchor, a second incision was made between the lead insertion site and the implantable pulse generator (IPG) pocket site (
Fig. 3). The anchor was attached and sutured to the surrounding tissues to anchor the leads securely. A 4-cm incision was made above right buttock to create the pocket for the rechargeable IPG. The leads were tunneled to the pocket and connected to the generator (
Fig. 4).
 | Fig. 1A 15-gauge Tuohy needle was advanced under fluoroscopic guidance through the sacral hiatus (A) and right and left octapolar lead was passed through the needle until cephalad electrode was at the S3 level (B). 
|
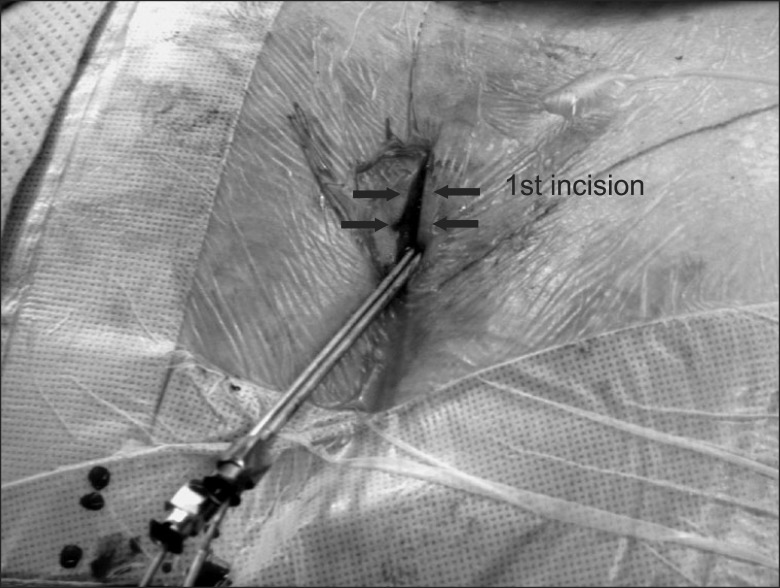 | Fig. 2A 5 cm incision was made at the Tuohy needle insertion site. 
|
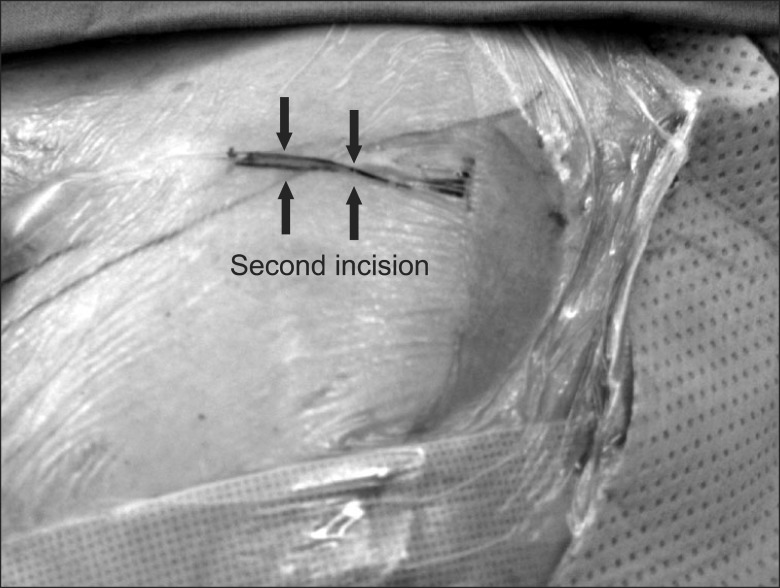 | Fig. 3A second incision was made between the lead insertion site and the implantable pulse generator pocket site and the lead was passed through the tunnel into second subcutaneous pocket. 
|
 | Fig. 4The leads were tunneled to the pocket and connected to the generator. 
|
Go to :

DISCUSSION
The methods approach for sacral stimulation is transacral, retrograde and/or anterograde [
4-
6]. There are pros and cons for each approach. A transsacral foraminal approach of sacral nerve stimulation has been associated with technical failures in maintaining electrode position and inconsistent outcomes [
7]. The advantages of the retrograde approach are the low rate of migration, low risk of infection, and good coverage of the pain site [
8]. However there are contraindications for retrograde stimulation. The alternative is the anterograde approach through the sacral hiatus. The lead could be placed introduced the sacral hiatus like a caudal epidural injection. The anterograde technique may have several advantages. First, it may be technically easier for inexperienced physicians. Second needle insertion for this approach may be safer because it does not risk spinal cord injury, Third, lead navigation may be easier [
9].
To reduce the possibility of technical failure, a preoperative evaluation was needed to determine the distance to the hiatus from the anus, and to determine the amount of coccygeal subcutaneous tissue or fat with ultrasound, and to determine whether the hiatus opening or not etc. If the distance from the anus to the hiatus was short, and little fat was observed, there could be difficulty securing the lead, leading to discomfort when the patient sits, and infection of the wound may occurred [
9]. However, there was no guideline in ths reference regarding the recommended distance to the hiatus from the anus or the depth of coccygeal fat. The anterograde approach would be difficult if anchoring the lead at the hiatus site. Therefore, the anchoring was performed between the lead insertion site and the IPG pocket. We believe this does not guarantee the prevention of lead migration. However, it does provide a decreased probability of lead migration, and/or patient discomfort when sitting. In conclusion, although anterograde sacral nerve stimulation through sacral hiatus had some drawback, this technique could be alternative technique for sacral stimulation in patients with intractable chronic pelvic pain.
Go to :


