Abstract
Kikuchi's disease (KD) is an idiopathic and self-limiting necrotizing lymphadenitis that predominantly occurs in young females. It is common in Asia, and the cervical lymph nodes are commonly involved. Generally, KD has symptoms and signs of lymph node tenderness, fever, and leukocytopenia, but there are no reports on treatment for the associated myofacial pain. We herein report a young female patient who visited a pain clinic and received a trigger point injection 2 weeks before the diagnosis of KD. When young female patients with myofascial pain visit a pain clinic, doctors should be concerned about the possibility of KD, which is rare but can cause severe complications.
Go to : 
Kikuchi's disease (KD) is an idiopathic and self-limiting necrotizing lymphadenitis that predominantly occurs in young females [1,2]. It is a rare disease with a worldwide distribution, but is relatively common in Asia [3]. The cervical lymph nodes are commonly involved in patients from the Far East [4-6]. Most patients visit the hospital because of the presence of cervical masses [4,5], and there are no reports of any patient visiting a pain clinic with cervical pain without a mass. We herein report a case of a young woman who visited a pain clinic because of cervical discomfort and was diagnosed with KD after 2 weeks.
A 27-year-old female patient visited a pain clinic for right-sided cervical tenderness that had continued for 5 days, and painful cervical rotation. She had no history of operations or other diseases or conditions with the exception of emotional stress.
The tenderness and a taut band were present on the right side of the sternocleidomastoid (SCM) muscle, and continuous stiffness with cervical motion pain was observed. The continuous pain was rated 2 on the visual analog scale (VAS), motion-related pain was rated 4, and sleep disturbance was not present. During the physical examination, there was no sensory disturbance, allodynia, skin erythema, mass, or limited range of motion. The patient refused further radiologic and laboratory examinations.
A tender point injection was performed on the tender point of the right SCM under a diagnosis of myofacial pain syndrome (MPS). The cervical motion became smoother immediately after the injection. However, there was no symptomatic improvement at follow-up 3 days after the initial visit.
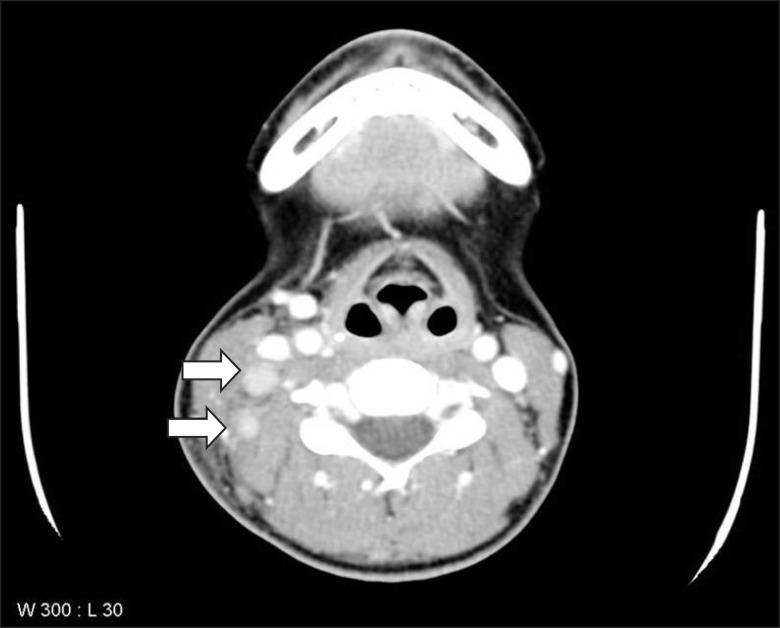
The lesion then started to swell with more severe tenderness, general weakness, and fatigue. On the seventh day, the patient developed febrile sensations, cold sweats, and chills. On the eighth day, her right neck swelling was grossly confirmed, and she visited the emergency department and consulted the otolaryngology department. Laboratory examination results showed a white blood cell count of 3,150/mm3, erythrocyte sedimentation rate of 62 mm/h, C-reactive protein level of 33.2 mg/dl, negative perinuclear antineutrophil cytoplasmic antibodies, negative TB interferon-gamma, and an antinuclear antibody ratio of 1:40. Cervical computed tomography (CT) showed several lymph nodes (<1.8 cm) with internal necrosis at the right level II to IV (Fig. 1). She was diagnosed with KD at the level IV lymph node based on aspiration cytology, which revealed several reactive lymphocytes. After 5 days of supportive care, the symptoms began to subside, so she was discharged without any complications. At the 1-month follow-up, the patient was free of pain and other discomforts.
Go to : 
KD is a rare disease, but is relatively common in Asia. There are several hypotheses on etiology, including viral infection and autoimmune disease. KD is associated with fever, myalgia, and leukocytopenia with elevated ESR, and is usually accompanied by cervical lymphadenopathy [4,5]. About half of patients with cervical lymphadenitis have cervical tenderness, and other organs such as lymph nodes, liver, spleen, and skin can also be involved [7]. Almost every patient's symptoms resolve in 2 months, and the recurrence rate is 2-3% [4,8]. Atypical symptoms are panuveitis with impairment of visual acuity, arthritis, aseptic meningitis, amygdalitis, cryptogenic organizing pneumonia, and renal failure. Although rare, there have been five cases of death associated with heart failure, transplantation, febrile syndrome [9] and SLE complicated with hemophagocytic syndrome [10]. KD is confirmed by lymph node biopsy and histological examination. CT images are similar to those of lymphoma, but the size of the lymph nodes is not as large as that in lymphoma [11]. However, no specific assay is available to confirm the radiologic diagnosis of KD.
Most patients visit clinicians because of lymph node masses, tenderness, or fever, and there is no report of a patient with MPS without any other symptoms. The patient in this case underwent tender point injection because the neck pain was diagnosed as MPS. However, the pain and swelling of the neck worsened after 4 days; thus, the initial MPS of SCM can be regarded as the initial symptom of KD. The patient showed fever, leukocytopenia with elevated ESR, and cervical lymph node enlargement and tenderness without any other accompanying symptoms. Thus, she was discharged later with no complications.
Among publications referenced by pain clinicians, none mentions KD. This report implies a disconcerting situation if clinicians do not consider KD in the care of patients with similar signs and symptoms. Therefore, the possibility of KD in young patients with MPS should be considered and explained to the patients. KD is rare but can be accompanied by severe complications; thus, examinations for diagnosis and consultation might be performed when KD is suspected.
Go to : 
References
1. Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes: a clinicopathological study. Nihon Ketsueki Gakkai Zasshi. 1972; 35:379–380.
2. Fujimoto Y, Kozima Y, Yamaguchi K. Cervical subacute necrotizing lymphadenitis. A new clinicopathological entity. Naika. 1972; 30:920–927.
3. Bosch X, Guilabert A, Miquel R, Campo E. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol. 2004; 122:141–152. PMID: 15272543.
4. Chung PS, Lee SJ, Yoon JS, Park SJ, Kim JS, Moon JH. Clinical and radiologic characteristics of Kikuchi's disease. Korean J Otolaryngol-Head Neck Surg. 2006; 49:85–89.
5. Hong KH, Kim KM, Park JH. A clinical study of histiocytic necrotizing lymphadenitis (Kikuchi's disease). Korean J Otolaryngol-Head Neck Surg. 1999; 42:490–494.
6. Lee HS, Tae K, Jang KJ, Lee EJ, Kim SK. Clinical characteristics of subacute necrotizing lymphadenitis. Korean J Otolaryngol-Head Neck Surg. 1998; 41:640–646.
7. Atwater AR, Longley BJ, Aughenbaugh WD. Kikuchi's disease: case report and systematic review of cutaneous and histopathologic presentations. J Am Acad Dermatol. 2008; 59:130–136. PMID: 18462833.

8. García CE, Girdhar-Gopal HV, Dorfman DM. Kikuchi-Fujimoto disease of the neck. Update. Ann Otol Rhinol Laryngol. 1993; 102:11–15. PMID: 8420463.

9. Silva AF, Focaccia R, Oliveira AC, Sementilli A, Reis GF. Kikuchi-Fujimoto disease: an unusual association with acute renal failure. Braz J Infect Dis. 2010; 14:621–627. PMID: 21340304.

10. Kampitak T. Fatal Kikuchi-Fujimoto disease associated with SLE and hemophagocytic syndrome: a case report. Clin Rheumatol. 2008; 27:1073–1075. PMID: 18465190.

11. Kwon SY, Kim TK, Kim YS, Lee KY, Lee NJ, Seol HY. CT findings in Kikuchi disease: analysis of 96 cases. AJNR Am J Neuroradiol. 2004; 25:1099–1102. PMID: 15205157.
Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download