Abstract
Background
The aim of this study was to document the optimal spacing of two cannulae to form continuous strip lesions and maximal surface area by using water-cooled bipolar radiofrequency technology.
Methods
Two water-cooled needle probes (15 cm length, 18-gauge probe with 6 mm electrode tip) were placed in a parallel position 10, 20, 24, 26, and 28 mm apart and submerged in egg white. Temperatures of the probes were raised from 35℃ to 90℃ and the progress of lesion formation was photographed every 1 minute with the increase of the tip temperature. Approximately 30 photographs were taken. The resultant surface areas of the lesions were measured with the digital image program.
Results
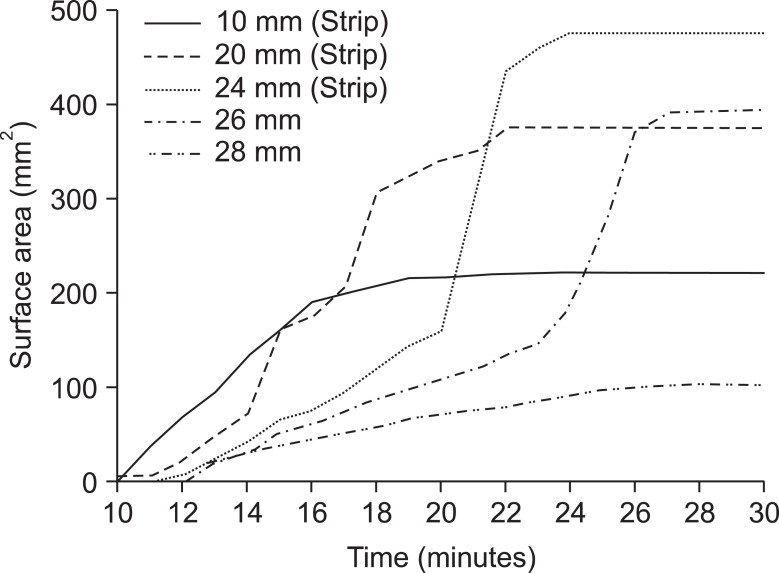
Continuous strip lesions were formed when the cannulae were spaced 24 mm or less apart; monopolar lesions around each cannula resulted if they were spaced more than 26 mm apart. Maximal surface areas through the formation of continuous strip lesion were 221 mm2, 375 mm2, and 476 mm2 in 10, 20, and 24 mm, respectively. Summations of maximal surface area of each monopolar lesions were 394 mm2 and 103 mm2 in 26 and 28 mm, respectively.
Conclusions
Water-cooled bipolar Radiofrequency technology creates continuous "strip" lesions proportional in size to the distance between the probes till the distance between cannulae is 24 mm or less. Spacing the cannulae 24 mm apart and treating about 80℃ for 24 minutes maximizes the surface area of the lesion.
Radiofrequency (RF) is now widely used in various medical departments for treating a wide variety of conditions including cardiac arrhythmia, benign prostatic hyperplasia, malignant tumors and chronic pain. In comparison with traditional monopolar RF, bipolar RF creates a continuous strip lesion that is proportional in size to distance between the electrodes. From this benefit, bipolar RF is reported to be superior in creating a larger and more predictable lesion over monopolar RF [1-3]. For this purpose, accurate prediction of lesion created by ablation is essential for less morbidity and more satisfying result especially in pain management. Water-cooled electrodes are capable of creating larger lesions than non cooled ones by removing heat from adjacent tissue and deliver power without causing high impedance and tissue charring [4]. By comparing the maximum surface area formed by conventional RF and cooled RF in egg white, these benefits of water-cooled RF could be specified.
This study is aimed to evaluate the maximum surface area formed by two parallel electrodes and the distance between them for creating a largest lesion.
Two water-cooled needle probes (15 cm length, 18 gauge probe with 6 mm electrode tip) were placed in a transparent bowel filled with egg white and used to create the lesions. The needles were fixed by the sponge above the bowel to be placed in a parallel position spaced 10 mm, 20 mm, 24 mm, 26 mm, and 28 mm apart. The first probe was connected to the RF electrode system (Trans-Discal™ System, Baylis Medical, Montreal Inc., QC, Canada) in the usual manner recommended by the manufacturer, and the second probe was attached, through an adapter provided by the same manufacturer. Energy level was set to maintain electrodes 20 Watt and the following impedance was around 90 Ω. The temperature of the cooled electrodes maintained 35℃ while the temperature of the second electrodes raised with the same energy level between 10 to 12 Watt. The transparent bowel was used for a clear vision of the RF lesions. From the initiation of the lesion formation, photographs were taken every 1 minute through 30 minutes. The surface areas of the lesions were measured under the assistance of a computer-imaging program designed to estimate the area of irregularly shaped regions (UTHSCSA Image Tool 3.0, Texas, USA). All of the procedures were repeated twicely and the average was calculated.
Double trial was done in procedures of each distance apart and similar results were shown between two trials. Continuous strip lesions were formed when the cannulae were spaced 24 mm or less apart. From further distances apart, even with larger maximum surface area, two separate monopolar lesions were formed (Fig. 1). Time to form initial continuous strip lesion in each group were 11, 10, and 12 minutes in 10, 20, and 24 mm. Maximal surface area through the formation of continuous strip lesion were 221 mm2, 375 mm2, and 476 mm2 in 10, 20, and 24 mm at 23, 22, and 24 minutes, respectively. Summation of maximal surface area of each monopolar lesions were 394 mm2 and 103 mm2 in 26 and 28 mm at 28 and 27 minutes, respectively (Fig. 2).
Recently for more accurate targeting and larger lesion formation, bipolar RF was proposed and has been applied in various procedures for pain management including sacroiliac joint denervation and facet rhizotomy [5-7]. In previous reports regarding use of bipolar RF ablation on sacroiliac joint dysfunction, placement of the cannulae less than 1 cm apart and treatment at 90℃ for 90 seconds was recommended [5]. Pino et al. [8] reported that using two 22-gauge, 100.5 mm cannulae with 5-mm active tips in egg white, a continuous strip lesion was formed when the two electrodes were placed closer than 6 mm apart. They reported that maximal surface area was 48.2 mm2 after 90 seconds at 90℃ when the probes were separated by 4 mm. Using egg white as a medium, Choi et al. [9] reported that in order to create strip lesion through bipolar RF thermocoagulation, a more than 80℃ in temperature and 90 seconds in time was required for 5 mm active tip within 6 mm intervals, and 90℃ and 120 seconds for a 10 mm active tip within 8 mm intervals. We previously reported sequential bipolar radiofrequency technique in lumbar sympathectomy [10]. The reason that sequential bipolar radiofrequency technique used was that the lesion created by conventional RF technique was not large enough for area required for sympathectomy.
In comparison with a conventional bipolar RF, water-cooled tip RF enables a significant larger lesion. It is associated with current delivery at high power and prolonging the duration of RF delivery in cooled tip RF [11]. Watanabe et al. [4] reported that by using cooled tip, depth and volume of myocardial lesion were significantly larger in dogs. For creating a larger lesion with less accurate targeting, bipolar RF with water-cooled tip is advantageous in various procedures of pain management of severe degenerative changes or failed back surgery syndrome in which accurate placement of electrode is difficult [5,12]. A significant increase in delivered energy necessary for an increase lesion size is associated with an increased duration of RF delivery. Prevention or delay of carbonization which increases the duration of RF delivery was observed between 20 to 50 Watt [11]. In this study, the electrodes were maintained energy level between 10 to 12 Watt and the temperatures of the cooled tip were also kept about 35℃ to prevent carbonization.
Continuous strip lesions were formed in three groups of 10, 20, and 24 mm. In group of 26 mm apart, the maximum surface area of two monopolar lesions around both cannulae tips was larger than a single lesion formed by a needle placed 24 mm apart. Two electrodes should be placed between 20 mm to 24 mm apart in clinical practice in order to -maximize the surface area and to form a resultant strip lesion. Treatment duration is required about 22 to 24 minutes to achieve maximal surface area.
As biologic effect of RF treatment is to denature protein, egg white, predominantly protein seemed a suitable medium in which to examine the production of a strip lesion [13,14]. Moreover, translucency of the egg white allowed visualization of the formation of the lesion over time and not just the result. Considering that the size of the lesions may be varied by factors such as vascularity and tissue conductivity of heat [15], further studies on medium other than egg white is required to exactly model in vivo tissue.
In conclusion, water-cooled bipolar Radiofrequency technology creates continuous "strip" lesions in size proportional to the distance between the probes when the distance between cannulae is 24 mm or less. Further trials with various medium are required to confirm the promising results by using bipolar RF with a cooled tip in pain management.
References
1. Nakada SY, Jerde TJ, Warner TF, Wright AS, Haemmerich D, Mahvi DM, et al. Bipolar radiofrequency ablation of the kidney: comparison with monopolar radiofrequency ablation. J Endourol. 2003; 17:927–933. PMID: 14744366.

2. Anfinsen OG, Kongsgaard E, Foerster A, Aass H, Amlie JP. Radiofrequency current ablation of porcine right atrium: increased lesion size with bipolar two catheter technique compared to unipolar application in vitro and in vivo. Pacing Clin Electrophysiol. 1998; 21:69–78. PMID: 9474650.

3. Wang YG, Lu ZY, Zhao HY, Song YE, Li RL. A comparative study of radiofrequency ablation in unipolar and bipolar fashion. J Tongji Med Univ. 1995; 15:73–76. PMID: 8731956.

4. Watanabe I, Masaki R, Min N, Oshikawa N, Okubo K, Sugimura H, et al. Cooled-tip ablation results in increased radiofrequency power delivery and lesion size in the canine heart: importance of catheter-tip temperature monitoring for prevention of popping and impedance rise. J Interv Card Electrophysiol. 2002; 6:9–16. PMID: 11839878.
5. Ferrante FM, King LF, Roche EA, Kim PS, Aranda M, Delaney LR, et al. Radiofrequency sacroiliac joint denervation for sacroiliac syndrome. Reg Anesth Pain Med. 2001; 26:137–142. PMID: 11251137.

6. Gauci CA. Wedley JR, Gauci CA, editors. Sacroiliac joint denervation. Handbook of clinical techniques in the management of chronic pain. 1994. Chur, Switzerland: Harwood Academic;p. 12–13.
7. Ray CD. Percutaneous radiofrequency facet nerve blocks: treatment of the mechanical low back syndrome. Procedure technique series. 1982. Boston, MA: Radionics;p. 18–19.
8. Pino CA, Hoeft MA, Hofsess C, Rathmell JP. Morphologic analysis of bipolar radiofrequency lesions: implications for treatment of the sacroiliac joint. Reg Anesth Pain Med. 2005; 30:335–338. PMID: 16032584.

9. Choi EM, Shin KM, Nam SK, Cheong IY. A study about size and shape of bipolar radiofrequency lesions. Korean J Anesthesiol. 2008; 54:197–200.

10. Kang SS, Shin KM, Jung SM, Park JH, Hong SJ. Sequential bipolar radiofrequency lumbar sympathectomy in Raynaud's disease -A case report-. Korean J Anesthesiol. 2010; 59:286–289. PMID: 21057622.

11. Lorentzen T. A cooled needle electrode for radiofrequency tissue ablation: thermodynamic aspects of improved performance compared with conventional needle design. Acad Radiol. 1996; 3:556–563. PMID: 8796717.

12. Sim WS, Lee AR. Radiofrequency lumbar medial branch denervation using bipolar probe in patient with facet joint syndrome. J Korean Pain Soc. 2004; 17:153–158.

13. Lee KH, Yun SH, Kim HJ, Jung BH, Lim SY, Shin KM, et al. A comparison of the size and shape of radiofrequency lesions produced by different temperatures using straight and curved electrodes. Korean J Anesthesiol. 2000; 39:260–264.

14. Lee KH, Kim KS, Lim SY, Hong SY, Won RS, Shin KM. Experimental radiofrequency lesion size utilizing Different parameters and neuropathologic correlation on the peripheral nerve. Korean J Anesthesiol. 2002; 42:368–382.

15. Derby R, Lee CH. The efficacy of a two needle electrode technique in percutaneous radiofrequency rhizotomy: an investigational laboratory study in an animal model. Pain Physician. 2006; 9:207–213. PMID: 16886029.
Fig. 1
Bipolar cooled radiofrequency lesions formed with cannulae spaced 10, 20, 24, 26, and 28 mm apart in egg white when maximal surface area achieved. A continuous "strip" lesion is formed when the cannulae are separated by 24 mm or less and discrete lesions are formed when the cannula are 26 mm or more apart.
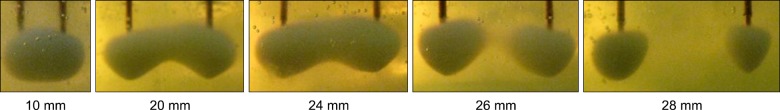
Fig. 2
Lesion surface area (mm2) according to duration of bipolar cooled radiofrequency treatment (minutes) is shown. The spacing of the 2 cannulae is indicated to the right of each line. Continuous "strip" lesions were made when the cannulae were spaced 24 mm or less apart. This figure was created by spreadsheet program (Microsoft excel® 2007, California, USA).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download