Abstract
A psoas compartment block has been used to provide anesthesia for orthopedic surgical procedures and analgesia for post-operative pain. Currently, this block is advocated for relieving pain in the lower extremity and pelvic area resulting from various origins. We report a case of a 69-year-old male patient who had gait abnormality with posterior pelvic and hip pain, which were both aggravated by hip extension. From the magnetic resonance image, the patient was found to have a laterally herniated intervertebral disc at the L2/3 level, which compressed the right psoas muscle. This was thought to be the origin of the pain, so a psoas compartment block was performed using 0.25% chirocaine with triamcinolone 5mg, and the pain in both the pelvis and hip were relieved.
The psoas muscle is involved with the curvature of the pelvis and spine, which starts at the thoracic vertebrae to connect with the lower vertebral body and transverse process. It proceeds past the pelvis to extend up to the lesser trochanter [1]. The psoas muscle plays a most important role when walking, as it pulls the spine forward while standing, and balances the body when sitting. Therefore, when the psoas muscle continuously contracts due to injury or stress, the vital dynamics of the pelvis, lumbar, and even the cervical vertebrae, can be disturbed. This incongruity can be the cause of pain in the lower back, pelvis, buttocks, and the femoral region. It can trigger a distinctive psoas gait, where the patient drags their leg while walking since the leg is not strongly pushed forward [2].
The psoas compartment block is performed on parts of the lumbar plexus and the sacral plexus for pain in the front thigh and inner, lower leg [3]. Since Chayen et al. first reported its use in the pelvic joint and lower thigh surgery in 1976 [4], it has also been performed in the open reduction of femoral neck fracture [5], and applied in the pain reducing treatment of cancer patients [6].
The author encountered a 69 year old male patient who had gait abnormality with pain in the hip joint caused by a laterally herniated intervertebral disc at the L2/3 level, which compressed the right psoas muscle. In a short term monitoring follow up, a satisfactory effect of pain control was obtained through psoas compartment blockade, thus it is being reported for literature review.
A 69 year old male patient, with height at 172 cm and weight at 70 kg, visited the hospital with gait abnormality in his right leg and pain in the pelvic joint area, which had continuously continued since its occurrence two years ago. The patient had a history of undergoing low anterior resection, radiation treatment, and chemotherapy four years prior for rectal cancer, and was taking insulin and oral hypoglycemics for diabetes. Since two years ago, the patient's leg could not be straightened properly when walking and pain in the pelvic area occurred when there was sudden movement. He had visited pain clinics, rehabilitation clinics, neurology, and orthopedics, but did not receive any specific diagnosis and had endured with the aid of physical and drug treatments. The degree of pain was 4-5/10 in the visual analog scale (VAS), and the symptoms were pain in the right pelvic joint when walking, and when lying down, the pubic area felt tight and painful when the leg was completely straightened, with pain subsiding when the leg was bent.
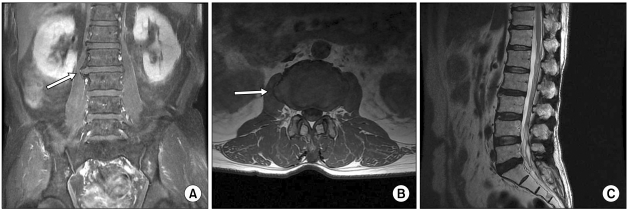
During the physical examination, the straight leg raising test was 90/90, but there was pain in both thighs, and the Patrick test indicated that both sides were positive. The Ganslene test was also positive in both sides, but the pain was worse in the right. There was tenderness in the spinous process of L3, and there were no tender points in the facet joints. The patient also complained of tenderness in sacroiliac joints, gluteus medius, and piriformis. In the magnetic resonance image (MRI), there were no metastasis or recurrence observed, but the disc between L2 and 3 had been herniated to the right and was pressing the right psoas (Fig. 1).
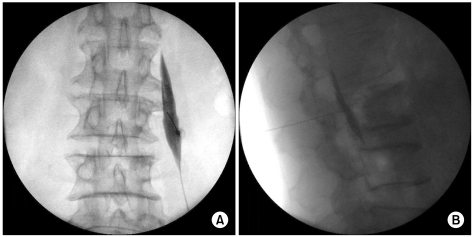
Hence, the gait abnormality and pain was considered to be caused by the laterally herniated intervertebral disc that compressed the right psoas muscle, and so a right psoas compartment blockade was performed. First, the patient was laid prone and the skin was sterilized. Under C-arm guidance, the transverse processes of the L3 were confirmed and an approach was made with a 22-G Tuohy needle (ARROW®, Arrow International Inc., USA). At the position where resistance ceased, was the location after the psoas muscle was observed with the contrast medium, which was shown when 0.25% levobupivacaine (Chirocaine®, Abbott, Elverum, Norway) 10 ml and triamcinolone diacetonide 5 mg were injected (Fig. 2). The patient stated that there were no effects from the drug therapy received at another hospital, so in order to discern the effects of the blockade no other particular oral medication was prescribed. When the patient visited the outpatient clinic one week after the procedure, periods without pain had continued for two to three days and gait abnormality had also disappeared during this period, but at the time of visit, a pain of VAS 5/10 was experienced by the patient. Hence, it was decided that the psoas compartment blockade was effective, so it was performed three times in two week intervals. As a result, the patient has shown improvements in pain of about VAS 3/10, so we are still monitoring his progress.
The psoas muscle is the muscle involved with the curve of the pelvis and spine, which starts at the thoracic vertebrae to connect with the lower vertebral body and transverse process. It goes past the pelvis and extends up the lesser trochanter [1]. When standing, it pulls the spine forward, while keeping the balance of the body when sitting, so it has an important role during walking motion. Therefore, when the psoas muscle continuously contracts from injury or stress, the vital dynamics of the pelvis, lumbar, and even the cervical vertebrae can be disturbed. This incongruity can cause pain in the lower back, pelvis, buttocks, and the femoral region. Also, there could be a transformation in the hip joint curve, and as a result, movement can be limited when using the hip joint. Thus, when there is a problem in the psoas muscle, it can trigger a distinctive psoas gait, where the patient drags their leg while walking as the leg cannot be strongly pushed forward [2].
The differential diagnosis for patients with these symptoms can consider infectious diseases, such as an abscess in the psoas muscle, hemorrhagic lesions, such as hematoma, and the metastasis of cancer. An abscess in the psoas muscle is not common, but is recently showing an increasing trend. Uncontrollable diabetes can be an important preceding factor [7], and symptoms, such as fever, pain in the side or hip area, and limitation in movement of the hip joints appear. Hemorrhagic lesions, such as hematomas, are known to occur more in patients who are either taking antiplatelet agents or anticoagulant treatment, or patients with blood coagulation disorders [8]. It is not common for cancer to spread to the psoas muscle, but for patients with a history of cancer, it must be taken into consideration that the psoas compartment can be a channel for the tumors to directly infiltrate the retroperitoneal, skeletal muscles, and pelvis [9]. There is also a report that, in a patient with rectal cancer, a biopsy performed in suspicion of an abscess in the psoas muscle, revealed the metastasis of cancer [10]. Treatment methods can be different for these diseases, such as internal medicine and surgery, so an accurate diagnosis is important. After differentiating the suspected diagnosis to a certain degree, through medical history, physical examination, and blood tests, it can be further confirmed through imaging.
Our case shows the discovery of the lateral disc herniation in the MRI. The case of lateral disc herniation is where the disc is herniated to the side of the root foramen, toward the outside of the spinal canal. Lateral disc herniation is a lesion that is easily missed because it is difficult to observe in a MRI image [11]. Even in our case, the reinforced image of T2 did not show a herniated disc or compression of the nerves (Fig. 1C), so if lesions in the psoas muscles had not been suspected, diagnosis would have been delayed under the false judgment that there were no disc problems. There are not many studies regarding the relationship between lateral disc herniation and the psoas muscle. However, there is a study that analyzes the connection between the sciatica and the reduced sectional area of the psoas muscle resulting from lateral disc herniation [12]. In addition, a case study reporting similar symptoms to meralgia paresthetica that results from lateral disc herniation is also available [13]. Since the psoas muscle is adjacent, through fibrous attachments, to all discs in the lumbar excluding the discs between L5 and S1 [14], lesions in the lumbar disc can affect the fascia disease of the psoas muscle [2]. This knowledge should also be included in the differential diagnosis.
Treatment regarding myofasciopathy, caused by the compression of the psoas muscle, is based on conservative treatment, but there is no proven definite treatment as of yet [14]. The authors thought of the mechanism for pain relief and gait abnormality when a psoas compartment blockade was performed using steroids. The psoas compartment is the space located between the psoas muscle and quadrates lumborum, and is surrounded by the psoas muscle and its fascia in the front, the lumbar, and the transverse process of the lumbar, ligament, muscle, and quadrates lumborum in the back [15]. Within this compartment, the lumbar plexus, the ventral ramus of the sacral plexus, iliohypogastric nerve, ilioinguinal nerve, genitofemoral nerve, lateral femoral cutaneous nerve, femoral nerve, obturator nerve, and parts of the sciatic nerve pass through [3]. The psoas compartment block is generally performed on the L3 or L4 disc and serves to block the lateral femoral cutaneous nerve, femoral nerve, and the obturator nerve, so the block is also known as the posterior lumbar plexus block. The iliohypogastric, ilioguinal, and genitofemoral nerve can be further blocked if medication is expanded toward the cephalad within the fascia [16]. As in this case, where the psoas compartment block was performed on L3, the steroid and local anesthetic is spread to the psoas muscle fascia and nerve within the psoas compartment, which relieves pain in the psoas muscle and hip joint, and results in the improvement of gait abnormality. The amount of steroid used in the psoas compartment block is not determined in general, but 40-80 mg of triamcinolone diacetonide is used for each procedure when performing the epidural block [17]. However, in the case of the psoas compartment block, the fascia is located adjacently so muscle atrophy can occur from the steroid, and since the patient in this case had diabetes as an underlying disease, only 5 mg of triamcinolone diacetonide was used in the initial procedure. There was also the purpose of determining the effects of the blockade. Therefore in further additional procedures, increasing the amount of steroid can be considered. It was found that using local anesthesia, coupled together with steroids, is more effective and also possesses long-term pain relief. These effects are thought to be from the steroid suppressing the hypothalamus, pituitary gland, and the adrenal gland [6].
The patient in our case had a history of rectal cancer and had diabetes as an underlying disease, so an abscess in the psoas muscle or metastasis was suspected. However, the suspicion proved to be incorrect since the symptoms had gradually occurred for two years and there were no signs of infection. The MRI results showed compression of the psoas muscle by a laterally herniated disc, so pain was relieved and gait abnormality improved through the psoas compartment blockade. In these kinds of patients, detailed history taking, physical examination, and imaging should be performed for accurate diagnosis and proper treatment, with the psoas compartment blockade now being able to be considered as another treatment method.
References
1. Bogduk N, Pearcy M, Hadfield G. Anatomy and biomechanics of psoas major. Clin Biomech (Bristol, Avon). 1992; 7:109–119.

2. Travell JG, Simons DG. Myofascial pain and dysfunction: the trigger point manual. 1983. Baltimore: Lippincott Williams & Wilkins;p. 89–109.
3. Brown DL. Psoas compartment block. Atlas of regional anesthesia. 2006. 3rd ed. Philadelphia: Elsevier/Saunders;p. 95–96.
4. Chayen D, Nathan H, Chayen M. The psoas compartment block. Anesthesiology. 1976; 45:95–99. PMID: 937760.

5. Chelly JE, Casati A, Al-Samsam T, Coupe K, Criswell A, Tucker J. Continuous lumbar plexus block for acute post-operative pain management after open reduction and internal fixation of acetabular fractures. J Orthop Trauma. 2003; 17:362–367. PMID: 12759641.

6. Lee WJ, Sung NS, Kim C. Effect of psoas compartment block in low extremity pain from stomach cancer: a case report. J Korean Pain Soc. 1992; 5:113–116.
7. Lansdown AJ, Downing A, Roberts AW, Martin D. Psoas abscess formation in suboptimally controlled diabetes mellitus. Case Report Med. 2011; 2011:249325. PMID: 21811508.

8. Wada Y, Yanagihara C, Nishimura Y. Bilateral iliopsoas hematomas complicating anticoagulant therapy. Intern Med. 2005; 44:641–643. PMID: 16020897.

9. Yang WT, Yeo W, Metreweli C. Imaging of iliopsoas metastasis. Clin Radiol. 1999; 54:85–89. PMID: 10050734.

10. Avery GR. Metastatic adenocarcinoma masquerading as a psoas abscess. Clin Radiol. 1988; 39:319–320. PMID: 3396286.
11. Hood RS. Far lateral lumbar disc herniations. Neurosurg Clin N Am. 1993; 4:117–124. PMID: 8428146.

12. Dangaria TR, Naesh O. Changes in cross-sectional area of psoas major muscle in unilateral sciatica caused by disc herniation. Spine (Phila Pa 1976). 1998; 23:928–931. PMID: 9580961.

13. Trummer M, Flaschka G, Unger F, Eustacchio S. Lumbar disc herniation mimicking meralgia paresthetica: case report. Surg Neurol. 2000; 54:80–81. PMID: 11024511.

14. Sajko S, Stuber K. Psoas Major: a case report and review of its anatomy, biomechanics, and clinical implications. J Can Chiropr Assoc. 2009; 53:311–318. PMID: 20037696.
15. Torres GM, Cernigliaro JG, Abbitt PL, Mergo PJ, Hellein VF, Fernandez S, et al. Iliopsoas compartment: normal anatomy and pathologic processes. Radiographics. 1995; 15:1285–1297. PMID: 8577956.

17. Manchikanti L. Role of neuraxial steroids in interventional pain management. Pain Physician. 2002; 5:182–199. PMID: 16902669.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download