This article has been
cited by other articles in ScienceCentral.
Abstract
Intracranial hypotension is characterized by a postural headache which is relieved in a supine position and worsened in a sitting or standing position. Although less commonly reported than postural headache, sixth nerve palsy has also been observed in intracranial hypotension. The epidural blood patch (EBP) has been performed for postdural puncture headache, but little is known about the proper timing of EBP in the treatment of sixth nerve palsy due to intracranial hypotension. This article reports a case of sixth nerve palsy due to spontaneous intracranial hypotension which was treated by EBP 10 days after the onset of palsy.
Go to :

Keywords: abducens nerve palsy, epidural blood patch, spontaneous intracranial hypotension
Headache due to spontaneous intracranial hypotension is characterized by an orthostatic headache without a recent history of dural puncture and not attributable to another disorder. It can be diagnosed by meeting at least one of the following criteria: (1) low CSF opening pressure (≤ 6 cmH
2O), (2) sustained improvement of symptoms after epidural blood patching, (3) demonstration of an active spinal CSF leak, and (4) cranial MRI changes of intracranial hypotension (eg, brain sagging or pachymeningeal enhancement) [
1]. Other symptoms such as nausea, neck stiffness, and tinnitus can also be observed [
2]. On rare occasions, cranial nerve palsy can be involved. Among the cranial nerves associated with ophthalmolplegia, the sixth cranial nerve is the most frequently involved, either unilaterally or bilaterally [
3,
4] with horizontal diplopia and blurred vision. For diagnosis, magnetic resonance imaging (MRI) of the brain, nuclear cisternography and computed tomography (CT) and more recently MR myelography can be performed. Although the initial treatment is conservative care, EBP can be helpful if symptoms do not respond to conservative treatment.
CASE REPORT
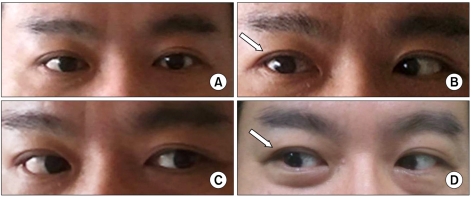
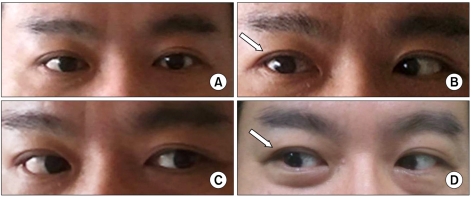
A 43-year-old male visited the Department of Family Medicine with a history of mild headache, neck pain and nausea which had been ongoing for a day. He had a history of hypertension for 2 years and his blood pressure was 145/95 mmHg on his first visit. The patient had a chief complaint of a headache in both the occipital and temporal areas and tightness in the posterior neck which were aggravated by standing, coughing and shaking of the head. On the other hand the symptoms were relieved by lying down. Simple analgesics and muscle relaxants were prescribed, but they did not ease the headache. On the sixth day since the onset of headache, the patient experienced blurred and double vision and this led him to the hospital again. On neurologic examination, he had horizontal diplopia which became worse when gazing to the right side (
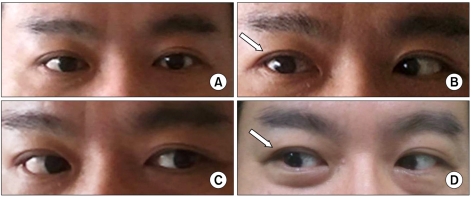
Fig. 1A-C). Ophthalmologic consultation confirmed right sixth cranial nerve palsy, and the consulting neurologist recommended performing brain and orbit MRI. The brain MRI showed diffuse pachymeningeal thickening and enhancement (
Fig. 2A). The patient was admitted on the supposition that intracranial hypotension might have caused the headache and sixth nerve palsy. Spinal tap was performed and revealed an opening pressure of 11 cmH
2O in the right decubitus position. A CT myelogram was also taken, and contrast leakage was found in the posterior epidural space from C4 to C6 (
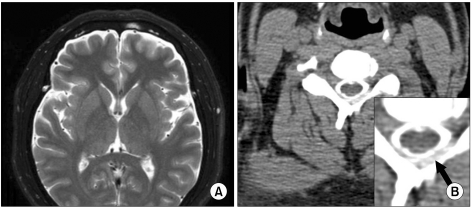
Fig. 2B). The patient's symptoms, MRI finding, and CT myelogram could all be explained by spontaneous intracranial hypotension in spite of the normal CSF pressure. He was referred to the pain clinic for EBP 10 days after the onset of the diplopia. We performed the EBP at the C4/5 level under fluoroscopic guidance by injecting 8 ml of autologous blood (
Fig. 3). The headache was nearly relieved by the following day, but the diplopia was only partially improved. After discharge from the hospital, the patient was observed for 2 months and we confirmed his complete recovery from the diplopia (
Fig. 1D).
 | Fig. 1Right sixth cranial nerve palsy (arrow): Looking forward (A), gazing to the right (B), and gazing to the left (C), and 1 month later after EBP, gazing to the right (D). 
|
 | Fig. 2Brain MRI shows diffuse pachymeningeal thickening and enhancement (A). CT myelogram shows contrast leakage in the posterior epidural space, black arrow in the magnified inset indicates CSF leakage (B). 
|
 | Fig. 3Cervical epidurography for EBP. 
|
Go to :

DISCUSSION
Transient sixth nerve palsy resulting from lumbar puncture was first reported in the early 1900s [
5], and it was usually associated with large gauge cutting spinal needles. The advent of smaller and pencil point spinal needles may have decreased the incidence of sixth nerve palsy, as well as the comments on this complication in many textbooks. However, anesthesiologists, who are frequently consulted for EBP as the treatment of intracranial hypotension, should always keep in mind the possibility of cranial nerve palsy in these patients. According to the review of Zada et al. [
3], in patients with cranial nerve manifestations resulting in ocular deficits secondary to intracranial hypotension, 83% of patients had abducens (6
th) nerve palsies, 14% had oculomotor (3
rd) nerve palsies, and 7% had trochlear (4
th) nerve paresis. Abducens nerve palsy due to intracranial hypotension is a benign condition and about 80% of patients recover spontaneously. However, if symptoms continue for 8 months or more, the possibility of permanent damage increases [
5].
Previously, the abducens nerve has been suggested to be susceptible to stretch by brain displacement or traction due to its long intracranial course. These days, more specific mechanisms for the development of abducens nerve damange have been suggested [
4,
6]. Anatomically, this nerve exits the brain stem between the medulla oblongata and pons, rises upward along the clivus, crosses branches of the basilar artery, and pierces the dura mater. Then, the nerve sharply bends over the ridge of the petrous apex of the temporal bone. The abducens nerve runs in the same direction in which typical caudal displacement of the brain occurs with intracranial hypotension. As a result, the force of traction associated with changes in intracranial pressure is fully transmitted to the nerve. The nerve can be stretched by downward displacement of the pons, and it may also be compressed at the dura, petrous apex, or basilar artery if the penetration aperture for the nerve in the dura or petrous apex is sharply edged or if branches of the basilar artery are well developed [
4,
6].
Since Gormley introduced the EBP for treatment of intracranial hypotension in 1960, the procedure has been widely used to treat postdural puncture headache (PDPH) and it has proven very effective. However, little is known about the proper timing of EBP in the treatment of sixth nerve palsy due to intracranial hypotension. According to the review of Bechard et al. [
7], among 12 cases of EBP for the management of PDPH and sixth nerve palsy, 11 cases completely resolved eventually, and in the review of Zada et al. [
3], ophthalmoplegia secondary to spontaneous intracranial hypotension was successfully corrected by EBP in 14 out of the 15 cases examined. In spite of the absence of clinical studies on the efficacy of the EBP, these cases imply that EBP could be helpful for treatment of sixth nerve palsy secondary to intracranial hypotension.
As for the proper timing of EBP, Bechard et al. [
7] suggested that EBP may lead to partial improvement and/or early resolution of symptoms if performed within 24 hr from the onset of diplopia, and that EBP performed more than 24 hr after the onset of diplopia systematically fails to relieve the palsy. However, our patient showed favorable results from an EBP performed 10 days after the onset of diplopia. This kind of variability in responses to EBP may be due to differences in the degree of nerve compression and injury.
The volume of autologous blood used for EBP differs according to the level of injection. Compared to the lumbar area, a lesser volume (about 10 ml) is used in the cervical area [
8]. In the present case, we injected 8 ml of blood, because the patient began to complain tightness at the injection site at this volume.
We report a case of a patient with abducens nerve palsy due to spontaneous intracranial hypotension who experienced improvement of diplopia after an EBP which was performed 10 days from the onset of diplopia.
Go to :