Abstract
Background
Rocker bottom shoes (RBS) are popular among patients with different foot, leg, or back problems in Korea. Patients with knee osteoarthritis concurrent weakness in the quadriceps femoris muscle, who wear these shoes, are often assumed to develop piriformis syndrome (PS). This study was performed to improve the understanding about the effect of wearing such shoes on duration of the syndrome in knee osteoarthritis.
Methods
We randomly assigned 150 patients with PS, who had used RBS daily for at least 6 months, to 2 groups, the S (stopped wearing) and K (kept wearing) groups. Both the groups were subdivided into the O and N groups, comprising patients with and without knee osteoarthritis, respectively. The effects of the treatment, including piriformis muscle injections and a home exercise program, were compared between the 2 groups by using a flexion-adduction-internal rotation (FAIR) test, a numeric rating scale (NRS), and the revised Oswestry disability index (ODI) during the 12-week follow-up.
Since 2003, shoes with a soft sole, rounded in the anterior-posterior direction underneath the heel area, providing an unstable base of support with a rocker bottom, have been popular among patients with different foot, leg, or back problems in Korea. They alter movement patterns, particularly at the ankle, increasing the angle of dorsiflexion at initial contact and causing continuous plantar-flexion until the end of the stance phase. Rocker bottom shoes (RBS) have been designed as a training method to strengthen the lower leg muscles. However, it has been noted that they should be used with caution in patients with knee problems, since these subjects walked with slightly increased flexion during the stance phase accompanied by increased activity in the vastus medialis and lateralis muscles. Activity of the rectus femoris muscle was also reduced during the stance-to-swing transition period [1].
Piriformis syndrome (PS) is a neuromuscular disorder that occurs when the sciatic nerve is compressed or irritated by the piriformis muscle. It is characterized by pain, tingling, and numbness in the buttocks and along the path of the sciatic nerve, down the lower thigh and into the leg [2]. Primary PS can be due to the intrinsic pathology of the piriformis, such as myofascial pain, anatomical variations, hypertrophy, and myositis ossificans, or can be caused by trauma to the pelvis or buttock. Secondary PS includes all other etiologies such as herniated disc, facet syndrome, trochanteric bursitis, sacroiliac joint dysfunction, endometriosis, or other conditions impinging on the sciatic nerve [3].
Weakness of the quadriceps femoris muscles is a common clinical sign associated with knee osteoarthritis (OA) and pain [4,5]. Patients with knee OA favor certain motions in order to avoid acute pain. Weakness of the quadriceps femoris, the extensor group of the anterior thigh muscles, is common in patients with symptomatic knee OA, and the weakness of this muscle is strongly associated with knee pain [6].
RBS increase the range of motion of the ankle joints. This subsequently increases tension in the posterior compartment of the leg muscles, the extensor group of the anterior thigh muscle, and the outer hip and gluteal muscles, finally including the piriformis muscle. If patients with OA and associated weakness of the quadriceps femoris muscle wear RBS, they may often develop PS. This study was performed to determine the effect of RBS on the development or continuation of PS in patients with knee OA.
This study was conducted from January 2009 to May 2010. The protocol was approved by the Research Ethics Committee at the Hospital. At the first visit, we randomly assigned 150 patients, who had developed piriformis syndrome after wearing RBS daily for at least 6 months, into 2 groups: the S group (stopped wearing RBS) and K group (kept wearing RBS). Both the groups were subdivided into O and N groups based on the presence or absence of grade 1 or 2 (classified according to Kellgren-Lawrence grading scale) knee OA [7].
PS was diagnosed by using both symptoms and signs. The main symptom was pain over the buttock area, radiating downwards to the posterior thigh or leg along the course of the sciatic nerve. Diagnosis of PS by physical examination required the following results: (1) a negative straight leg raise test, (2) positive Laségue's test, and (3) positive flexion-adduction-internal rotation (FAIR) test. In the event of a positive FAIR test, a confirmatory diagnostic and therapeutic injection of 5 ml of 1% lidocaine and 20 mg of triamcinolone was delivered into the affected piriformis muscle under fluoroscopic guidance to confirm the diagnosis (Fig. 1). A change from a positive to a negative FAIR test 1 h after the injection was confirmed the presence of PS. Exclusion criteria were previous surgery of the spine, hip, or knee.
Identical treatment with oral medications and a perform-at-home self-exercise program was provided for both the groups. The medications included an analgesic mixture of a weak opioid, an acetaminophen, and a non-steroidal anti-inflammatory drug and tizanidine, which is used as a muscle relaxant. The self exercise program required the patient perform to assume a certain position 20 times a day (Fig. 2). The effects of treatment in the 4 groups were compared using the FAIR test, a numeric rating scale (NRS, from 0 to 10, with 0 being no pain at all and 10 being the worst pain imaginable), and the revised Oswestry disability index (the revised ODI) [8,9], expressed as the disability percentile with respect to activities of daily living before and 1, 4, 8, and 12 weeks after the injection.
All statistical analysis was performed using SPSS program (ver. 12.0 for Windows, SPSS Inc., Chicago, IL) was used for statistical analysis. Intergroup comparisons of the demographic data, i.e., the age of the patients and duration of wearing shoes with the rocker bottom were performed using an analysis of variance ANOVA test with multiple comparisons. The numbers of patients in each group were compared using a chi-square test. During the follow-up period, the percentage of positive FAIR tests was compared between using a chi-square test. The NRS scores and the revised ODIs were compared between groups by using a repeated-measures ANOVA test.
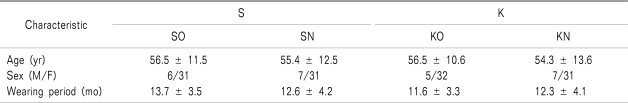
At first visit, no intergroup differences were observed in the age and sex of the patients, and in the duration of wearing RBS. The M/F ratio of PS development was found to be 25/125 (Table 1).
All the evaluation indices, namely the FAIR test ratios, NRS scores, and revised ODIs, significantly decreased in all the 4 groups 1 week after confirmatory diagnostic and therapeutic injection. However, there were no intergroup differences in these evaluation indices between the subjects of the 4 groups (Fig. 3). The positive-FAIR ratios were significantly higher in the KO group than the SN group at weeks 4, 8, and 12, and the SO group at weeks 8 and 12 after injection (Fig. 3A). The mean NRS scores in the KO group were significantly higher than the SN group at weeks 4, 8, and 12 (Fig. 3B). In the KO group, the revised ODIs weeks 4 to 12 after injection were significantly higher than those in the SN and SO groups (Fig. 3C).
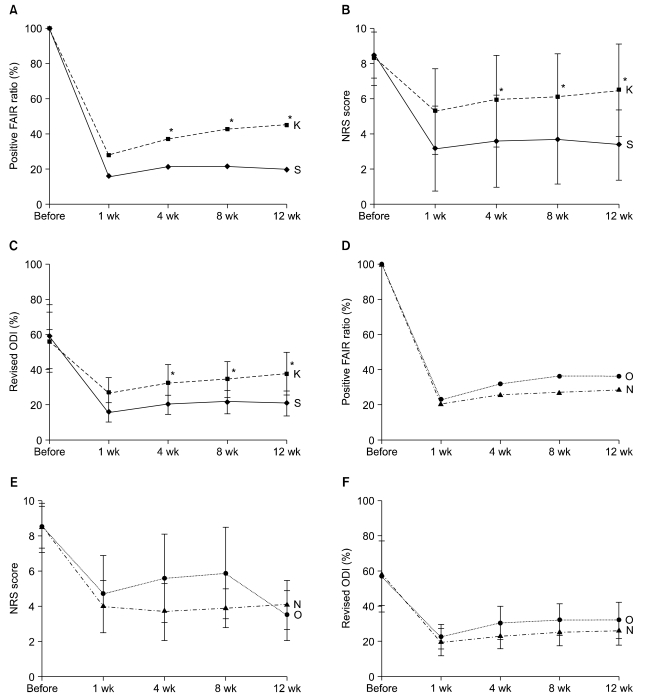
The effectiveness of the treatment, compared on the basis of the ratio of the FAIR tests, the NRS scores, and the revised ODIs, was identical in all the 4 groups for at least 1 week after confirmatory diagnostic and therapeutic injection. Among the patients who developed PS after wearing RBS for over 6 months, the OA patients who had kept wearing the shoes during the study period of 12 weeks (the KO group) were more refractory to the treatment than the patients without OA who had stopped wearing the shoes after the first visit (SN group). The S group patients were more receptive to the treatment than the K group from the 4 weeks after the injection until the end of the study. However, the presence of OA did not affect treatment effectiveness; no difference was observed between the O and N groups. In addition, gender seemed to play a role in development of PS with women being more vulnerable to PS if they wore RBS, regardless of the presence of OA at the first visit.
The piriformis muscle originates at the pelvic surface of the second- to fourth sacral vertebrae and inserts at the apex of the greater trochanter of the femur. Therefore, the main action of the muscle is external rotation, abduction, and extension of the hip joint. Its innervations are direct branches from the sacral plexus from L5 to S2. The hip and gluteal muscles can be categorized into 3 groups according to their location and functions: the inner hip muscles, the outer hip muscles, and the adductor muscle group. The inner hip muscles are the iliopsoas muscles. The adductor muscle group is composed of the obturator externus, pectineus, adductors longus and brevis, adductors magnus and minimus, and gracilis muscles. The outer hip muscles can be divided by the orientation of the muscles. The vertically-oriented outer hip muscles are the gluteus maximus, medius, and minimus, tensor fasciae latae, and piriformis muscles, whereas, the horizontally-oriented outer hip muscles are the obturator internus and quadratus femoris muscles [10].
During normal walking, each leg functions alternately as the stance leg and the swing leg. The stance phase, which makes up for 60% of the gait cycle, begins when the heel contacts the ground (heel strike), and ends when the toes push off from the ground (toe-off). The swing phase, which makes up 40% of the gait cycle, begins with toe-off and ends with heel strike. Therefore, 1 gait cycle can be defined as the period between 2 heel strikes of the same foot [10]. Heel strike process is the connection between the end of swing phase and the beginning of stance phase; it is required to for stabilize the gait cycle. However, heel strike tends to be omitted when using RBS. Thus, walking becomes unstable, and an increased power output is required from the normally unused muscles of the lower extremities. The walking speed was significantly slower in subjects wearing RBS, because of shorter step length and slight reduction in the number of steps/min (cadence). It is likely that some of the RBS-caused changes in the kinematic data from the hip, for example, reduced peak hip flexion at the initial stance and range of motion over the gait cycle, are caused by this decrease in the stride length [4]. However, when the subjects walked at a normal speed or a little faster, RBS had a destabilizing effect and perturbed the stance [11].
Patients with knee OA favor certain motions to avoid acute pain. Weakness of the quadriceps femoris, the extensor group of the anterior thigh muscles, is a common clinical sign associated with knee osteoarthritis and pain [5,6]. In case of patients with OA wearing RBS, a series of events may occur due to increased movement of the ankle joint: increased muscular tension in the lower legs, increased tension of the weakened quadriceps femoris muscle, and eventually increased tension in the piriformis and other gluteal muscles. PS is known to be more common in women than in men. In this study, PS occurrence was 5 times higher in women than in men. This may be due to the biomechanics associated with the wider quadriceps femoris muscle angle ("Q angle") in the os coxae (pelvis) of women [12]. In genu varum, the mechanical axis causes abnormal pressure on the medial aspect of the knee joint and abnormal tension in the lateral joint structures: lateral collateral ligament, iliotibial tract, and biceps femoris muscle. In such situations, the tension in the piriformis muscle may be increased in order to lessen the abnormally increased tension in the lateral structures of the knee. In addition, in the toe-out gait in patients with knee OA, the external knee adduction moment is partially transformed into flexion during the early stance phase. This suggests that the load is partially shifted away from the medial compartment of the knee to the other structures [13]. However, RBS prevents the toe-out gait and may cause knee pain. To relieve the knee pain, the piriformis muscle gets overused and tightened; this may eventually lead to PS. We attributed the lack of difference in treatment effectiveness between O group and N groups in our study to the fact that PS development was observed in patients with knee OA only after the use of RBS.
This study had certain limitations. First, such a study assessing the causative, attributing, or triggering factors has to be performed including volunteers with and without OA. This study investigated the effect of RBS on the continuation of PS, -not on the development of the PS. Further studies on the influence of RBS in the development of PS in OA patients are required. Second, patients with OA (the SO and KO group) could not efficiently perform the home-exercise program because of their knee pain and deformity. Therefore, better exercise program or physiotherapy is required for the treatment of PS in OA patients. Third, primary PS-related anatomical variations in the relationship between the piriformis muscle and the sciatic nerve were not considered. At least 3 types of variable courses of the sciatic nerve over the piriformis muscle have been described. The most common situation (almost 85% of cases) is that the sciatic nerve leaves the lesser pelvis inferior to the piriformis muscle. Common variants of this situation are a high division of the sciatic nerve (approximately 15% of cases). The fibular division (the common fibular nerve), and sometimes, the posterior femoral cutaneous nerve, pass through the piriformis muscle, and may become compressed at the location, thereby, causing PS. The other variant is that the fibular part of the sciatic nerve leaves the lesser pelvis above the piriformis muscle (only about 0.5% of cases). Further research is required into the variability of nerve passage. This research may help education of vulnerable patients with PS, who have a variant passage of the sciatic nerve over the piriformis muscle. A fourth limitation of this study is that it did not consider the habits of the individuals wearing RBS. Each case differed in terms of duration of wearing RBS, as well as, the activity levels in daily life. Some patients walked very fast without warming up before the leg exercises. This study did not restrict or control the gait of the patients.
RBS have been designed as a training method to strengthen the muscle groups of the lower leg. In Korea, these shoes are used by a wide range of patients with foot, leg, or back problems, without any warning to the OA patients. However, the RBS-caused gait alterations may lead to the development of PS in patients with existing knee OA. In conclusion, RBS may extend the period of spasm of the piriformis muscle in OA patients despite of treatment. Furthermore, they may be a triggering factor of PS in some patients with knee OA.
References
1. Romkes J, Rudmann C, Brunner R. Changes in gait and EMG when walking with the masai barefoot technique. Clin Biomech (Bristol, Avon). 2006; 21:75–81.

2. Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve. 2009; 40:10–18. PMID: 19466717.

3. Dere K, Akbas M, Luleci N. A rare cause of a piriformis syndrome. J Back Musculoskelet Rehabil. 2009; 22:55–58. PMID: 20023365.

4. Messier SP, Loeser RF, Hoover JL, Semble EL, Wise CM. Osteoarthritis of the knee: effects on gait, strength, and flexibility. Arch Phys Med Rehabil. 1992; 73:29–36. PMID: 1729969.
5. Slemenda C, Brandt KD, Heilman DK, Mazzuca S, Braunstein EM, Katz BP, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997; 127:97–104. PMID: 9230035.

6. Lewek MD, Rudolph KS, Snyder-Mackler L. Quadriceps femoris muscle weakness and activation failure in patients with symptomatic knee osteoarthritis. J Orthop Res. 2004; 22:110–115. PMID: 14656668.

7. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957; 16:494–502. PMID: 13498604.

8. Fairbank JC, Pynsent PB. The oswestry disability index. Spine. 2000; 25:2940–2952. PMID: 11074683.

9. Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002; 82:8–24. PMID: 11784274.

10. Ross LM, Lamperti ED. Thieme atlas of anatomy: General anatomy and musculoskeletal system. 2006. Stuttgart: Thieme;p. 360–509.
11. Albright BC, Woodhull-Smith WM. Rocker bottom soles alter the postural response to backward translation during stance. Gait Posture. 2009; 30:45–49. PMID: 19329317.

12. Pace JB, Nagle D. Piriform syndrome. West J Med. 1976; 124:435–439. PMID: 132772.
13. Jenkyn TR, Hunt MA, Jones IC, Giffin JR, Birmingham TB. Toe-out gait in patients with knee osteoarthritis partially transforms external knee adduction moment into flexion moment during early stance phase of gait: a tri-planar kinetic mechanism. J Biomech. 2008; 41:276–283. PMID: 18061197.

Fig. 2
A perform-at-home self-exercise program for piriformis muscle stretching. The exercise begins with a push- up position using hands and toes (A), followed by placing the affected leg across and underneath the body trunk so that, if possible, the affected knee is outside the trunk (B). The unaffected leg is extended straight back behind the trunk keeping the pelvis straight (C). The hips are moved backward toward the floor; the body is leant forward with the forearms toward the floor; the affected leg is kept in place, until a deep stretch is felt (D). The stretch is held for 30 s and then, the patient slowly returns to starting position.
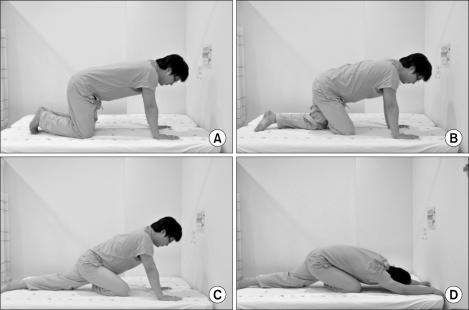
Fig. 3
Changes in the positive flexion-adduction-internal rotation (FAIR) test ratios (A), the mean numeric rating scale (NRS) scores (B), and the mean revised Oswestry disability indices (ODIs) (%) (C), during the follow-up period in the 4 groups. *All variables were significantly higher in the KO group than in SN group (P < 0.05). †All variables were significantly higher in the KO group than in the SO group (P < 0.05).
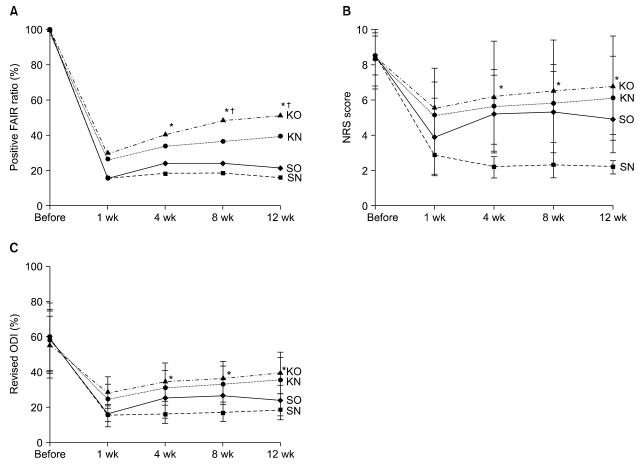
Fig. 4
Changes in the positive flexion-adduction-internal rotation (FAIR) test ratios (A), the mean numeric rating scale (NRS) scores (B), and mean revised Oswestry disability indices (ODIs) (%) (C), during the follow-up period in the S and K groups. No difference was observed in treatment effectiveness between N and O groups (D?F). *All variables were significantly higher in the K group than in the S group (P < 0.05).




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download