Abstract
Background
Facet joint disease plays a major role in axial low-back pain. Few diagnostic tests and imaging methods for identifying this condition exist. Single photon emission computed tomography (SPECT) is reported that it has a high sensitivity and specificity in diagnosing facet disease. We prospectively evaluated the use of bone scintigraphy with SPECT for the identification of patients with low back pain who would benefit from medial branch block.
Methods
SPECT was performed on 33 patients clinically suspected of facet joint disease. After SPECT, an ultrasound guided medial branch block was performed on all patients. On 28 SPECT-positive patients, medial branch block was performed based on the SPECT findings. On 5 negative patients, medial branch block was performed based on clinical findings. For one month, we evaluated the patients using the visual analogue scale (VAS) and Oswestry disability index. SigmaStat and paired t-tests were used to analyze patient data and compare results.
Facet joint disease, also known as zygapophyseal joint pain plays a major role in axial low-back pain. Pain derived from the zygapophyseal joint is characterized by local tenderness and pain on extension or exercise [1]. The low back pain distributes in a segmental nature and tends to have referred pain [2]. However no unique feature is present in facet joint disease which can distinguish it from pain from other sources, making diagnosis difficult. In addition, few diagnostic tests and imaging methods exist for identifying the exact anatomical level, making decisions of treatment difficult [2-5].
Some disagreement exists on the ability of radiologic imaging, including computed tomography (CT) and magnetic resonance imaging (MRI), to diagnose facet joint disease and predict its response to diagnostic nerve blocks [2,6-8]. However some studies have reported that bone scintigraphy with single photon emission computed tomography (SPECT) has a high sensitivity and specificity in diagnosing facet joint disease [9-11].
As facet joint disease does not completely correlate with physical signs and symptoms or with radiologic findings, deciding which medial branch level should be blocked accurately is difficult [2,8,12]. This leads to overuse of treatment agents, diagnostic tests, and unnecessary visits and procedures which result in negative cost-effectiveness.
We prospectively evaluated the use of bone scintigraphy with SPECT for the identification of patients with low back pain suspected to be related to facet joint disease. This was done to obtain an accurate diagnosis of the affected facet joint level. An ultrasound guided medial branch block was performed for treatment at the target level joint nerve directly based on SPECT findings.
The study was approved by the institutional review board and written informed consent was received from all patients participating in the research. This study enrolled 33 patients (14 males and 19 females) between 28 and 88 years of age. The patients had experienced chronic low-back pain over at least 6 months with aggrevation of the symptoms or expression of low-back pain with extension or rotation of the lumbar spine which was relieved by flexion and mild exercise. The exclusion criteria were a history of lumbar trauma, a history of lumbar surgical intervention, lumbar radiculopathy, uncontrolled or acute medical problems and chronic conditions that would interfere with interpretation of the outcome assessments.
All selected patients underwent bone scintigraphy followed by SPECT scanning of the lumbar spine. Technetium-99m was intravenously injected and delayed bone scintigraphy was taken. A planar image was acquired which was followed by SPECT of the lumbar spine. Bone scintigraphy and SPECT results were examined and assessed by nuclear medical physicians. Abnormal results and increased uptake of the facet joints were noted as 'positive' and normal results were noted as 'negative' (Fig. 1).
After the scintigraphy and SPECT results were obtained, ultrasound guided medial branch blocks were performed on all patients. For patients showing a high uptake in SPECT images, the medial branches of dorsal rami innervating the joint lesion level and showing a high uptake on SPECT images were blocked by ultrasound guidance. For SPECT-negative candidates, medial branch blocks were performed at levels based on clinical symptoms and physical examinations, because images showing the lesion were not available. All patients received 1% lidocaine, 2 ml each level and total dose of triamcinolone 30 mg. The amount and type of medial branch block agent were given equally to SPECT-positive and negative patients. After medial branch block treatment, all patients were followed-up at the second and fourth week. All previously prescribed adjuvant analgesics and physical treatments continued as scheduled.
For one month, visual analogue scale (VAS) and Oswestry disability index of all participating patients were evaluated at 2-week intervals. Demographic findings and previous medical histories were collected, and adverse events after medial branch block treatment were reported. The sensitivity and specificity of SPECT were calculated at the second and fourth week.
SigmaStat (version 3.0, Systat software Inc, San Jose, California, USA) was used as the statistical software tool. A paired t-test was applied for comparing before and after treatment results of the ultrasound guided medial branch block. Statistical significance was set at P < 0.05.
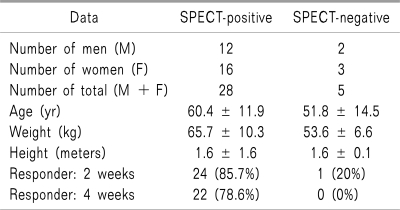
This study enrolled 33 patients with clinically suspected facet joint disease. Among total 33 patients, the number of the SPECT-positive patients showing increased uptake was 28 and the normal imaging SPECT-negative patients was 5. Patients showing more than a 50% reduction in the VAS score from their initial VAS score after medial branch block treatment were assigned 'responders'. The VAS score was measured at the second week and fourth week after treatment. The Oswestry disability index results were also collected. Table 1 shows the demographic characteristics of the patients and the number of responders.
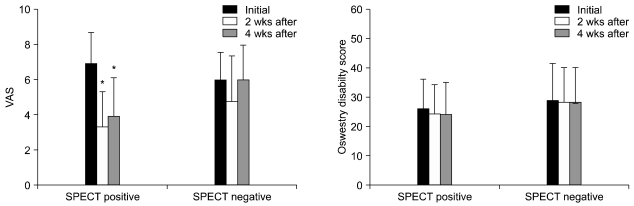
Of the 28 SPECT-positive patients, 24 (85.7%) were responders at the second week after medial branch block treatment and 22 (78.6%) at the fourth week. Of the 5 SPECT-negative patients, 1 (20%) was a responder at the second week and none were found (0%) at the fourth week. The initial VAS score of the 28 SPECT-positive patients was 6.8 ± 1.8 (mean ± SD). After medial branch block treatment, the VAS score was 3.13 ± 1.54 (mean ± SD) in the second week and 3.9 ± 2.16 (mean ± SD) in the fourth week. The initial VAS score of 5 SPECT-negative patients ranged from 6.33 ± 1.87 (mean ± SD). The VAS score ranged from 5 ± 2.28 (mean ± SD) in the second week and 6 ± 2 (mean ± SD) in the fourth week. No meaningful results were observed in the Oswestry disability index (Fig. 2).
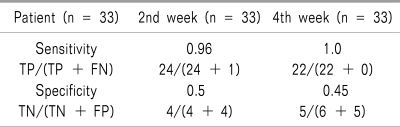
Table 2 lists the sensitivity and specificity of SPECT at the 4-week follow-up. The results shows a sensitivity value of 96% at the second week and 100% at the fourth week. The specificity was 50% at the second week and 45% at the fourth week.
The result show that SPECT-positive patients showed a significantly better response to ultrasound guided medial branch block than SPECT-negative patients. The sensitivity of SPECT was high although the specificity was low.
No adverse events from the medial branch block were reported during the study, except for one 54-year old male patient who complained of dizziness for two days. This condition spontaneously relieved.
In this study, we found that bone scintigraphy and SPECT results can be helpful in diagnosing clinicaly suspected facet disease. SPECT was found useful in finding the actual site and level where the procedure (medial branch block) should be performed. When patients with positive bone scintigraphy and SPECT results were treated with an ultrasound guided median branch block at the increased uptake level, improvements were found in the VAS score for four weeks, although no significant changes were observed in the Oswestry disability index. SPECT-negative patients showed almost no meaningful response to medial branch block, actually showing probability of miss-diagnosis.
Facet joint disease is one of the major causes of chronic low-back pain in population. Chronic facet joint pain occurs with repeated chronic strains or after an acute traumatic event beyond its physiologic limits. Eisenstein and Parry [1] have researched the pathologic presentation of facet disease patients and found damage, necrosis, ulceration, and fibrillation of articular cartilage with exposure of the subchondral bone in the facet joints. However disagreement exists about the exact criteria of facet joint disease and few methods exists for diagnosing it, along with risks of overestimation [2-5]. The prevalence of lumbar facet disease varies widely according to age, medical history, and patient occupation [2,13,14]. Screening criteria [4] are not suitable for predicting treatment outcomes [15]. Controlled diagnostic blocks are the method of choice for diagnosing facet joint disease [2,4,16,17]. Single blocks are known to be low in reliability for diagnosis because of their high false-positive results. Controlled blocks have the most specificity in diagnosis. However, some physicians are concerned about cost, time, and the invasiveness of the procedure. Intraarticular injection and medial branch block, including radiofrequency neurotomy, are valid treatments for facet joint disease. Of the two some doubt exists concerning the value of intraarticular corticosteroid injections in patients suffering from chronic low back pain [18]. Medial branch block is the definite method of choice in treatment of facet disease patients [17,19]. Most medial branch block procedures are perfomed under fluoroscopy guidance and these procedures need specialy equipped clinics. A risk of irradiation is also present to both patients and physicians. However, an ultrasound guided approach can be safe and reliable without the need for special spaces for radiation devices [20]. Ultrasound guided medial branch block is recently studied to have a high success rate, cost-effective, and has fewer complications [20-22].
Many attempts have been made to find the anatomic relationship of facet joint disease through radiologic imaging methods including MRI and CT. However none showed significant relationship in predicting positive response to medial branch block [2,23]. Facet joint disease findings from MRI images were interpreted differently among radiologists, which indicates a low reliability [7]. Lehman et al. [8] found that CT had a higher reliability than MRI, but it had only moderate agreement values among interpreters. These results show that defining the precise level of medial branch block based on radiologic readings is not reliable. Previous studies reported that patients with positive SPECT scans showed significant improvement in VAS scores and pain questionnaire scores after intra-facet joint injection [9,10]. Holder et al. [11] reported the value of using a planar scan and SPECT in facet joint disease patients. In this study, they reported a high sensitivity of SPECT scans and high negative predictive value. However we performed a medial branch block instead of a joint injection because a medial branch block known to be superior to facet joint injection in diagnosis and treatment. Our study results also showed a high sensitivity (100%) value in the 4weeks of follow up, as 79% of patients showed response to the medial branch block based on SPECT findings.
Previous studies reported that screening of patients suspected of facet disease, based on an examination of symptoms and signs, produces some false negative diagnoses [24]. This can be due to technical problems or inadequate target selection. And as so, phsycians have difficulty deciding where to perform the block. The use of SPECT can be helpful in determining the site of the block. This can increase the sensitivity of the diagnostic block and produce a higher success rate while reducing costs and time. We concluded that SPECT is useful in identifying the abnormal anatomic level to be blocked so that the medial branch block treatment would be more effective.
In conclusion, SPECT can be a good adjuvant method in diagnosing facet disease with high sensitivity. It can identify and locate the site where a medial branch block should be performed. Although SPECT is insufficient alone in diagnosing facet disease, and we could not prove its superiority over other diagnostic methods because of its low specificity, it can be helpful in finding the specific affected anatomic site of the lesion.
The small number of patients in the control group and short time of patient follow up is the limitation of this study. Further study with larger group with more control group, and more long-time follow up of patients is necessary. Also comparison of ultrasound guided medial branch block against medial branch block under fluoroscopic guidance would be helpful.
References
1. Eisenstein SM, Parry CR. The lumbar facet arthrosis syndrome. Clinical presentation and articular surface changes. J Bone Joint Surg Br. 1987; 69:3–7. PMID: 2950102.

2. Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007; 106:591–614. PMID: 17325518.

4. Revel M, Poiraudeau S, Auleley GR, Payan C, Denke A, Nguyen M, et al. Capacity of the clinical picture to characterize low back pain relieved by facet joint anesthesia. Proposed criteria to identify patients with painful facet joints. Spine. 1998; 23:1972–1976. PMID: 9779530.

5. Manchikanti L, Pampati V, Fellows B, Baha AG. The inability of the clinical picture to characterize pain from facet joints. Pain Physician. 2000; 3:158–166. PMID: 16906195.
6. Schwarzer AC, Wang SC, O'Driscoll D, Harrington T, Bogduk N, Laurent R. The ability of computed tomography to identify a painful zygapophysial joint in patients with chronic low back pain. Spine. 1995; 20:907–912. PMID: 7644955.

7. Carrino JA, Lurie JD, Tosteson AN, Tosteson TD, Carragee EJ, Kaiser J, et al. Lumbar spine: reliability of MR imaging findings. Radiology. 2009; 250:161–170. PMID: 18955509.

8. Lehman RA Jr, Helgeson MD, Keeler KA, Bunmaprasert T, Riew KD. Comparison of magnetic resonance imaging and computed tomography in predicting facet arthrosis in the cervical spine. Spine. 2009; 34:65–68. PMID: 19127162.

9. Dolan AL, Ryan PJ, Arden NK, Stratton R, Wedley JR, Hamann W, et al. The value of SPECT scans in identifying back pain likely to benefit from facet joint injection. Br J Rheumatol. 1996; 35:1269–1273. PMID: 9010055.

10. Pneumaticos SG, Chatziioannou SN, Hipp JA, Moore WH, Esses SI. Low back pain: prediction of short-term outcome of facet joint injection with bone scintigraphy. Radiology. 2006; 238:693–698. PMID: 16436824.

11. Holder LE, Machin JL, Asdourian PL, Links JM, Sexton CC. Planar and high-resolution SPECT bone imaging in the diagnosis of facet syndrome. J Nucl Med. 1995; 36:37–44. PMID: 7799079.
12. Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. Clinical features of patients with pain stemming from the lumbar zygapophysial joints. Is the lumbar facet syndrome a clinical entity? Spine. 1994; 19:1132–1137. PMID: 8059268.

13. Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O'Donnell CJ, et al. Facet joint osteoarthritis and low back pain in the community-based population. Spine. 2008; 33:2560–2565. PMID: 18923337.

14. Manchikanti L, Pampati V, Fellows B, Bakhit CE. Prevalence of lumbar facet joint pain in chronic low back pain. Pain Physician. 1999; 2:59–64. PMID: 16906217.

15. Laslett M, Oberg B, Aprill CN, McDonald B. Zygapophysial joint blocks in chronic low back pain: a test of Revel's model as a screening test. BMC Musculoskelet Disord. 2004; 5:43. PMID: 15546487.

16. Manchikanti L, Singh V, Pampati V. Are diagnostic lumbar medial branch blocks valid? Results of 2-year follow-up. Pain Physician. 2003; 6:147–153. PMID: 16883373.
17. Manchikanti L, Pampati V, Fellows B, Bakhit CE. The diagnostic validity and therapeutic value of lumbar facet joint nerve blocks with or without adjuvant agents. Curr Rev Pain. 2000; 4:337–344. PMID: 10998741.

18. Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y, et al. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991; 325:1002–1007. PMID: 1832209.

19. Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-up. Int J Med Sci. 2010; 7:124–135. PMID: 20567613.

20. Greher M, Kirchmair L, Enna B, Kovacs P, Gustorff B, Kapral S, et al. Ultrasound-guided lumbar facet nerve block: accuracy of a new technique confirmed by computed tomography. Anesthesiology. 2004; 101:1195–1200. PMID: 15505456.
21. Greher M, Scharbert G, Kamolz LP, Beck H, Gustorff B, Kirchmair L, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004; 100:1242–1248. PMID: 15114223.
22. Ha DH, Shim DM, Kim TK, Kim YM, Choi SS. Comparison of ultrasonography- and fluoroscopy-guided facet joint block in the lumbar spine. Asian Spine J. 2010; 4:15–22. PMID: 20622950.

23. Stojanovic MP, Sethee J, Mohiuddin M, Cheng J, Barker A, Wang J, et al. MRI analysis of the lumbar spine: can it predict response to diagnostic and therapeutic facet procedures? Clin J Pain. 2010; 26:110–115. PMID: 20090436.

24. Kaplan M, Dreyfuss P, Halbrook B, Bogduk N. The ability of lumbar medial branch blocks to anesthetize the zygapophysial joint. A physiologic challenge. Spine. 1998; 23:1847–1852. PMID: 9762741.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download