Occipital neuralgia is usually defined by International Headache Society as following criteria: (1) paroxysmal stabbing pain, with or without persistent aching between paroxysms, in the distribution(s) of the greater, lesser and/or third occipital nerves and (2) tenderness over the affected nerve. (3) Pain is eased temporarily by local anesthetic block of the nerve [1]. The pain may be idiopathic in nature or may develop following a history of cervical trauma. Neck movement or pressure over the occiput may worsen the pain [2]. In general, the management of occipital neuralgia comprises conservative treatment, conventional therapy, and medications. However, in a small percentage of cases, conservative treatment fails, and the pain causes such a high degree of disability that surgery becomes necessary [3].
The technique for identifying the location of the greater occipital nerve (GON) is well-established. The nerve is located in just above the superior nuchal line, about 2.5-3.0 cm lateral to the external occipital protuberance. The occipital artery, which is the most reliable landmark, is palpable at this point. However, in some patients, pulsation of the occipital artery cannot be detected, or detection is technically difficult because the occipital artery is small, the course of the artery is variable, or the patient has a thick neck [4]. Here, we describe a new technique of occipital neurectomy for occipital neuralgia of the bilateral GON and lesser occipital nerve (LON) performed using transcranial Doppler (TCD) sonography; this technique affords enhanced accuracy for detection of the occipital artery and provides quick pain relief.
CASE REPORT
A 64-year-old man with intractable stabbing pain in the distributions of the bilateral GON and LON presented at our hospital. On the day of presentation, he experienced pain all day, and the pain level was 8.9 on the visual analogue scale (VAS). Approximately 4 years before admission to our hospital, he had developed a burst fracture of C2 with cervical cord injury due to a fall (7 m) (Fig. 1A). His motor strength was quadriparesis grade 3. He underwent bilateral C1 lateral mass, C2 transpedicular, and C3 lateral mass screw fixation using the VERTEX® system via a posterior approach (Fig. 1B). After the operation, he complained of stabbing pain in the distribution of the bilateral GON and LON in the occipital area above the superior nuchal line (Fig. 2A). He was then transferred to a rehabilitative care unit for sequela of the cervical cord injury and was discharged from our hospital with grade 3 quadriparesis. However, he continued to experience intractable pain in the occipital area despite continuous medication. Pain control could not be achieved in spite of medical treatment with non-steroidal anti-inflammatory drugs, opioids (oxycodone 60 mg), antidepressants (amitriptyline 30 mg), and anticonvulsants (gabapentin 2,400 mg). Nerve blocks (GON, LON, and third occipital nerve blocks) were performed several times, which led to temporary improvements. The patient also underwent radiofrequency (RF) thermocoagulation of the bilateral GON and the third occipital nerve 18 months ago. However, these procedures provided temporary pain relief. We recommended stimulator implantation on bilateral GON and LON, but the patient rejected the recommendation due to financial constraints and other factors. Therefore, we performed occipital neurectomy of the bilateral GON and LON. We started the approach with the patient under general anesthesia in the prone position by using a horseshoe-shaped headrest. After shaving a limited area over the superior nuchal line, pulsation of the occipital artery was detected by using a portable TCD sonography machine, and an 8-MHz probe was manipulated along the superior nuchal ridge until the blood flow in the occipital artery was audible and visible (Fig. 2B). The occipital artery was easily detected, and the point was marked. An incision was made in the skin around the marked occipital artery along the superior nuchal line, and skin edges were retracted. The fascia containing the neurovascular bundle (GON and occipital artery) was exposed (Fig. 3). Further, the nerve was separated from the vessels, and an approximately 3-cm-long portion of the nerve was excised. Thereafter, the branches of the LON were avulsed along the superior nuchal line, and the excised GON tissue was sent for histological examination. After the operation, his headache disappeared gradually, despite the fact that he had discontinued all medication except antidepressants. Histological examination revealed normal nerve bundles. The patient was doing well at 5 months after the operation.
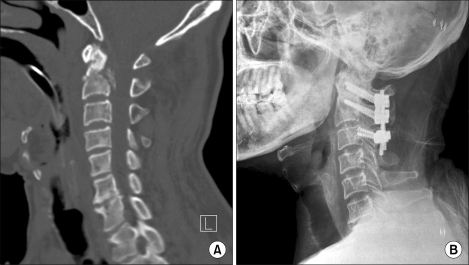 | Fig. 1(A) Computed tomography (CT) scan of the cervical spine with the bone-window setting showing a burst fracture of C2. (B) Postoperative plain lateral radiography showing C1-C3 screw fixation. |
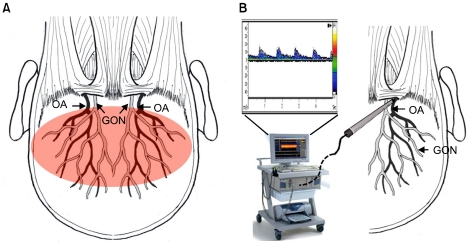 | Fig. 2(A) Pain distribution in the patient in the distribution of the bilateral greater occipital nerve and lesser occipital nerve in the occipital area above the superior nuchal line. (B) The pulsation of occipital artery can be detected by using a portable transcranial Doppler (TCD) sonography machine: an 8-MHz probe is manipulated along the superior nuchal ridge until the blood flow in the occipital artery is audible and visible. GON: greater occipital nerve, OA: occipital artery. |
Go to : 
DISCUSSION
Patients with occipital neuralgia can be divided into the following 2 groups: patients with structural causes and patients with idiopathic causes. Structural causes of occipital neuralgia include trauma to the GONs and/or LONs, compression of the GONs and/or LONs or C2 and/or C3 nerve roots by degenerative changes in the cervical spine, cervical disc disease, and tumors affecting the C2 and C3 nerve roots [2]. In patients with occipital neuralgia, surgical considerations are carefully taken into account if medical management is ineffective [3]. Several surgical tools such as electric stimulation, dorsal cervical rhizotomy, neurolysis of the GON, and surgical decompression are available, and RF thermocoagulation may be considered [2,3,5-9]. RF thermocoagulation has been widely used to treat occipital neuralgia. The benefits of this procedure are that it is safe and efficacious and is associated with a short recovery period and no permanent scarring; however, the results can be certainly different if direct coagulation of the trunk is performed [2]. Occipital nerve avulsion has benefits over an alcohol block or occipital nerve section since it provides more prolonged pain relief and since there is less likelihood of development of a painful traumatic neuroma resulting from the procedure [3]. In cases in which entrapment of the nerve by scar tissue or suture material is encountered, neurolysis of the GON and sectioning of the inferior oblique muscle may provide pain relief, thereby obviating the need for nerve avulsion [9]. Occipital nerve stimulator implantation has been shown to significantly reduce pain in occipital neuralgia patients in whom conservative therapies failed [6]. The procedure has some advantages, including minimal invasion and no permanent destruction of nerves or other vital structures. Another benefit is that patients can first undergo a trial of temporary percutaneous lead placement for several days prior to permanent lead implantation [2].
In the present case, pain management using medication, physical therapy, nerve block, and RF thermocoagulation did not provide consistent substantial pain relief, and it was followed by recurrence of pain. We recommended stimulator implantations on bilateral GON and LON, but the patient rejected the recommendation due to financial constraints. Therefore, we performed occipital neurectomy of the bilateral GON and LON. Occipital neurectomy is usually indicated in cases in which nerve blocks provide relief initially but, through repetition, lose their effectiveness [3]. Before the operation, our patient underwent occipital nerve block several times, which provided temporary pain relief. Although neurectomy of the GON does tend to result in pain relief, the available evidence is insufficient to conclude that surgery is an effective treatment for occipital neuralgia. Moreover, this procedure can cause many complications such as early recurrence, scalp hypersensitivity, dysesthesias, and formation of a painful neuroma beneath the scalp [3]. Therefore, the surgeon should carefully consider all neurectomy-related complication and explain to the patients prior to considering surgical intervention.
The GON receives sensory fibers from the C2 nerve root and is the thickest cutaneous nerve in the body. It emerges below the middle of the inferior oblique muscle, pierces the trapezius 2.5 cm lateral to the external occipital protuberance, and supplies the posterior part of the vertex [2,4]. The occipital artery, which serves as the most reliable landmark, is palpable at this point. Identification of the occipital artery is important for identifying the precise location of the occipital nerve. However, identification of the occipital artery by palpation can be technically difficult in patients with thick necks or small occipital arteries. Although palpation is possible, accurate determination of the site is difficult owing to weak pulsation in some patients. Therefore, traditional method determined on the basis of palpation of the occipital artery is time-consuming. We performed occipital neurectomy of the GONs and LONs by using TCD sonography, and we believe that TCD sonography can be used to easily and precisely detect the pulsation of the occipital artery. Occipital neurectomy performed using TCD sonography has some advantages, which are follows: (1) In almost all patients, the locations of the occipital artery and the GON could be identified; (2) The location of the occipital artery and nerve could be more accurately determined in a very short time; and (3) Precise detection of the GON via a small incision afforded short operation time. We believe that this new technique of occipital neurectomy via a small skin incision performed using TCD sonography is easy and reliable, has a short operative time, and provides rapid pain relief in cases of occipital neuralgia.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download