Abstract
Kummell's disease is a spinal disorder characterized by delayed post-traumatic collapse of a vertebral body with avascular necrosis. Although definitive treatment for Kummell's disease has not been established, it has been reported that percutaneous vertebroplasty or kyphoplasty has shown good results. However, these procedures are not recommended for severely collapsed vertebral bodies because of the risk of cement leakage or technical difficulties. Authors report a rare case of spontaneous reduction in vertebral height by the insertion of a working cannula into the vertebral body in Kummell's disease.
Go to : 
Kummell's disease is a disorder characterized by vertebral body avascular necrosis and collapse, and the clinical pattern is that patients suffer relatively mild lower back pain immediately after trauma and then a more severe pain comes following a silent period [1-3]. Radiologically, a characteristic intravertebral vacuum cleft is observed [1]. Although definitive treatment for Kummell's disease has not been established, it has been reported that percutaneous vertebroplasty or kyphoplasty has shown good results as a minimally invasive treatment [4]. However, vertebra plana with a compression rate higher than 70% is known as a relative contraindication for general percutaneous vertebroplasty because of cement outflow or difficulties in the procedure [5,6]. We performed a kyphoplasty in a patient with Kummell's disease accompanied by a severe vertebral body compression fracture in which the compression rate was higher than 70%. During the procedure, we experienced a rare case in which the height of the vertebral body was spontaneously recovered immediately after inserting a lumbar puncture needle into it. Thus, herein we report this case with a relevant review of the literature.
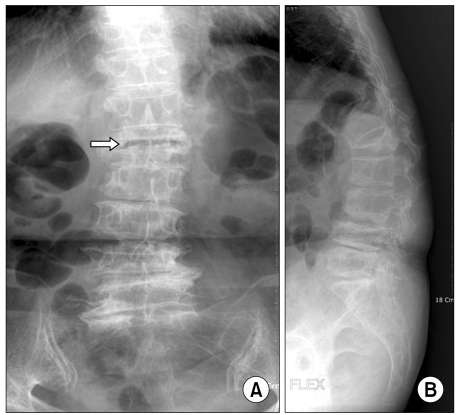
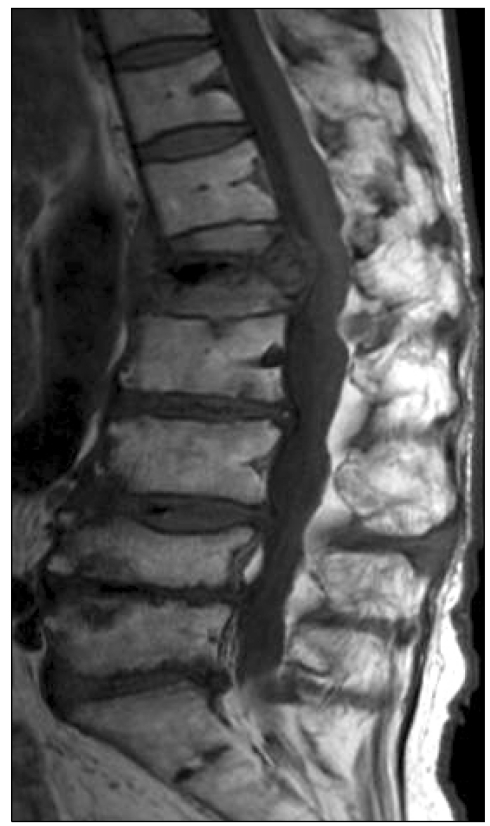
A 73-year old female patient 150 cm tall and weighing 50 kg visited our hospital presenting with the complaints of lower back pain and radiating pain to right lower extremity. The lower back pain started when the patient fell down nine years ago. At first, mild lower back pain had occurred from time to time, but severe pain with a visual analogue score (VAS) of 8 or higher started to occur three months prior to her visit. The patient did not have any particular medical history except osteoporosis diagnosed in her late fifties. She felt pain as if her body was collapsing or sinking, accompanied by pulling pain at the hip and groin. The pain became more severe when standing up and moving, and relieved when lying down at rest. The physical examination showed tenderness at the first lumbar (L1) spinous process region. There were no abnormal findings in any other neurological examinations. The plain radiograph showed severe osteoporosis over the vertebral bodies, a severe compression fracture of the L1 vertebral body in which the anterior compression rate was 70% or higher, and an intravertebral vacuum cleft in the vertebral body (Fig. 1). Magnetic resonance imaging showed a low signal area of L1 in the T1 weighted image and a high signal in the T2 weighted image (Fig. 2).
Despite conservative treatment for more than four weeks including continuous epidural pain control, the patient's pain did not decrease and she was rejecting surgical procedures such as a spinal fusion. Although the case was not a general indication of percutaneous vertebroplasty and kyphoplasty due to the severe collapse of the vertebral body, we decided to do transpedicular kyphoplasty using this method to block the cement outflow by slowly injecting highly viscous bone cement.
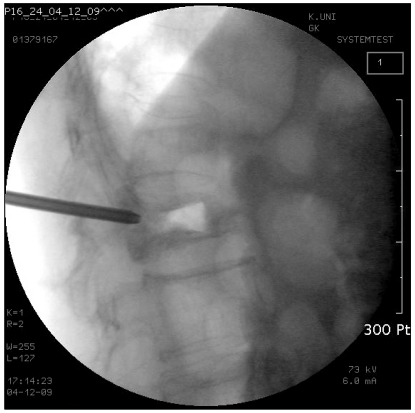
Before the procedure, cefazolin 1 g was intravenously injected to the patient as a preventive antibiotic. We had the patient take the prone position, supporting her abdomen with a pillow, in order to reduce abdominal lordosis. To check the patient's state during the procedure, we monitored the blood pressure, heart rate, and oxygen saturation, with supplement of oxygen through a nasal cannula. The skin on the area to be operated on was aseptically prepared and draped. For the sake of sedation and analgesia during the procedure, when needed, we injected fentanyl intravenously with a total of 100 µg. Using the C-arm image, we verified the pedicle of L1 and determined a working cannula implantation position and angle. Local infiltration anesthesia was performed with 1% lidocaine on the expected cannula implantation pathway. Under fluoroscopic C-arm guidance, we implanted the cannula into the fractured vertebral body through the vertebral pedicle. At the moment when the left cannula was inserted into the vertebral body, air flowed into the vertebral body with a popping sound, and the level of the vertebral body recovered spontaneously (Fig. 3). The cannula was also inserted into the right side, and balloons were inflated with a pressure of 50-100 psi to recover the level of vertebral body. Then, 4.5 ml of bone cement was slowly injected through each side of cannulas through the L1 vertebral body (Fig. 4). While injecting the bone cement, cement leakage out of the vertebral body was meticulously examined in both posteroanterior and lateral fluoroscopic views. The kyphoplasty was successfully implemented without cement leakage or clinical problems. The patient was discharged after the procedure without any particular abnormal findings. After the procedure, the VAS of the patient was 2, indicating that the preoperative pain almost disappeared. Currently, the patient during follow-up visits has not received any particular treatments except for the medication for osteoporosis.
Go to : 
Kummell's disease is a delayed disorder characterized by avascular necrosis and the collapse of a vertebral body. The avascular necrosis accumulates gas or liquid inside the vertebral body, which is characteristically found as an intravertebral vacuum cleft on the computed tomography or plain radiograph. In an intravertebral vacuum cleft, a space formed by the necrotic bones, fusion of the fractured bones is difficult, and pseudoarthrosis, which could be moved by the patient's posture or respiration, forms [7]. This causes severe pain depending on the patient's posture and motion.
Previous reports in the literature have mainly advocated conservative treatments such as bed rest and the wearing of aids as the treatment for Kummell's disease. However, the effect of the conservative treatment is often limited because vertebral body necrosis continuously progresses and natural healing hardly occurs in this disease [4,8]. In the case where there is neurological damage, spinal fusion is done as a surgical treatment [9,10]. However, spinal fusion through general anesthesia is also quite limited because most of the patients are old accompanied by severe osteoporosis. Hence, percutaneous vertebroplasty and kyphoplasty have become effective treatments as minimally invasive treatment. Bone cement injected during these treatments appropriately agglutinates fractures and resolves the instability due to the pseudoarthrosis by filling the vacuum cleft. In particular, kyphoplasty is considered as the more safe and effective procedure than percutaneous vertebroplasty in treating Kummell's disease because it can recover the vertebral body and reduce the cement outflow toward the space outside the vertebral body. Although it is known that there is no absolute contraindication for these procedures as a treatment for vertebral compression fractures; however, a severely collapsed vertebral body such as vertebra planar is generally considered as a contraindication for these procedures due to the difficulties in the procedure and the risk of cement outflow [5].
In this case, we performed kyphoplasty without any other alternatives, although the patient had a severe osteonecrotic vertebral compression fracture in which the vertebral compression rate was higher than 70% and difficulties including the difficulties of the procedure itself as well as the risk of cement outflow were anticipated. Unexpectedly, we experienced during the procedure spontaneous recovery of the vertebral body level as air suddenly flowed into the vacuum cleft of the vertebral body. This was rare even for us, and no similar cases were found in the literature. The possibility of an air embolism concerned us since air suddenly flowed into the vacuum cleft of the vertebral body; however, no complications including an air embolism occurred due to the flow of air into the vertebral body during the recovery process for the vertebral body. We assumed that the spontaneous recovery of the vertebral body level took place as the vacuum cleft was filled with air immediately after the cannula was inserted because negative pressure existed in the vacuum cleft where the intravertebral pseudoarthrosis had formed. Although there was the risk of bone cement outflow since the vertebral body could be damaged due to the sudden recovery, the kyphoplasty was successfully performed by slowly and meticulously injecting the bone cement, which had a consistency that was more viscous than the normal bone cement [11]. The patient achieved drastic analgesia and recovery of mobility after the procedure.
In conclusion, A kyphoplasty is worthy of considering as a good treatment modality that may provide analgesia and recovery of mobility without any complications for patients with Kummell's disease accompanied by severe vertebral body compression fracture. In some cases where a vacuum cleft in which negative pressure exists has been formed, spontaneous recovery of vertebral body level could occur.
Go to : 
References
1. Van Eenenaam DP, el-Khoury GY. Delayed post-traumatic vertebral collapse (Kummell's disease): case report with serial radiographs, computed tomographic scans, and bone scans. Spine (Phila Pa 1976). 1993; 18:1236–1241. PMID: 8362333.
2. Young WF, Brown D, Kendler A, Clements D. Delayed post-traumatic osteonecrosis of a vertebral body (Kummell's disease). Acta Orthop Belg. 2002; 68:13–19. PMID: 11915453.
3. Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978; 129:23–29. PMID: 693884.

4. Heini PF, Wälchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 2000; 9:445–450. PMID: 11057541.

5. Masala S, Fiori R, Massari F, Simonetti G. Kyphoplasty: indications, contraindications and technique. Radiol Med. 2005; 110:97–105. PMID: 16163144.
6. Masala S, Fiori R, Massari F, Cantonetti M, Postorino M, Simonetti G. Percutaneous kyphoplasty: indications and technique in the treatment of vertebral fractures from myeloma. Tumori. 2004; 90:22–26. PMID: 15143966.

7. McKiernan F, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res. 2003; 18:24–29. PMID: 12510802.

8. Mathis JM, Barr JD, Belkoff SM, Barr MS, Jensen ME, Deramond H. Percutaneous vertebroplasty: a developing standard of care for vertebral compression fractures. AJNR Am J Neuroradiol. 2001; 22:373–381. PMID: 11156786.
9. Kempinsky WH, Morgan PP, Boniface WR. Osteoporotic kyphosis with paraplegia. Neurology. 1958; 8:181–186. PMID: 13517483.

10. Li KC, Li AF, Hsieh CH, Liao TH, Chen CH. Another option to treat Kümmell's disease with cord compression. Eur Spine J. 2007; 16:1479–1487. PMID: 16568304.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download