Abstract
Background
Stellate ganglion block is usually performed at the transverse process of C6, because the vertebral artery is located anterior to the transverse process of C7. The purpose of this study is to estimate the location of the transverse process of C6 using the cricoid cartilage in the performance of stellate ganglion block.
Methods
We reviewed cervical lateral neutral-flexion-extension views of 48 patients who visited our pain clinic between January and June of 2010. We drew a horizontal line at the surface of the cricoid cartilage in the neutral and extension views of cervical lateral x-rays. We then measured the change in the shortest distance from this horizontal line to the lowest point of the transverse process of C6 between the neutral and extension views.
Results
There was a statistically significant difference in the shortest distance from the horizontal line at the surface of the cricoid cartilage to the lowest point of transverse process of C6 between neutral position and neck extension position in both males and females, and between males and females in both neutral position and neck extension position. The cricoid cartilage level was 4.8 mm lower in males and 14.4 mm higher in females than the lowest point of transverse process of C6 in neck extension position.
Go to : 
Stellate ganglion block is a sympathetic block of the head, neck, and upper extremity, and it is widely used in treating pain associated with the sympathetic nervous system [1]. Stellate ganglion block is sometimes used for preventing cough in awake surgery, or for lowering pulmonary hypertension in cardiac surgery [2,3]. The stellate ganglion is located at the C7-T1 vertebral level. Generally, stellate ganglion block is performed at the transverse process of C6 with operator's palpation by anterior paratracheal approach [4], because the vertebral artery is located in front of the transverse process of C7. The cricoid cartilage is known as the landmark of the C6 vertebral level in supine neutral position [5]. However, stellate ganglion block is almost always performed in supine "neck extension" position [6]. We speculated, therefore, that the anatomical relationship between the C6 vertebra and the cricoid cartilage would be changed in supine neck extension position. The purpose of this study is to estimate how much the level of the cricoid cartilage is changed from neutral position to neck extension position, and thus to more accurately find the position of the transverse process of C6 for stellate ganglion block.
Go to : 
The study protocol was approved by the Institutional Review Board for clinical trials. We reviewed cervical neutral-flexion-extension views of 48 patients who visited our pain clinic between January and June of 2010.
Inclusion criteria for the study were: (1) patients undergoing cervical neutral-flexion-extension views, and (2) patients with normal range of neck flexion (normal range: 45-70°). Exclusion criteria were: (1) patients with cervical spine operations, (2) patients with cervical disc space narrowing or severe cervical degenerative change, and (3) patients whose cricoid cartilage could not be identified in the x-rays.
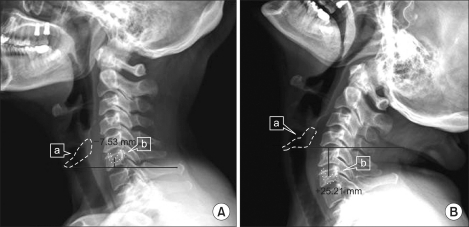
We drew a horizontal line at the surface of the cricoid cartilage in the neutral and extension views of cervical lateral x-rays. We then measured the change in the shortest distance from that horizontal line to the lowest point of the transverse process of C6 between neutral and extension views, using a picture archiving and communication system (Fig. 1).
Data concerning the distance were expressed as means ± SD, and statistical program SPSS version 18.0 (SPSS Inc., Chicago, Illinois, USA) was used for analysis. The change in the distance from the horizontal line at the surface of the cricoid cartilage to the lowest point of the transverse process of C6 between neutral and extension view was analyzed with paired t-test, and the difference in the distance from the horizontal line to the lowest point of the transverse process of C6 in the same position between males and females was also analyzed with paired t-test. A P value less than 0.05 was considered statistically significant. Because there was no preliminary study, we could not estimate the sample size. So we just reviewed x-ray views of 48 patients who visited our pain clinic between January and June of 2010.
Go to : 
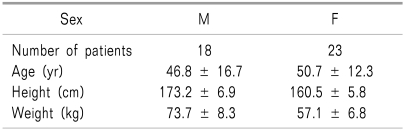
Table 1 summarizes the demographic data of the subjects. 3 patients were excluded because of cervical spine operations, and 4 patients were excluded because we could not identify the cricoid cartilage in their x-rays.
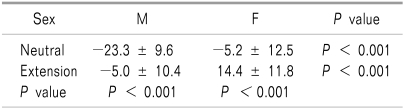
In the neutral position, the mean cricoid cartilage level was lower than the lowest point of the transverse process of C6 by 23.3 mm in males and 5.2 mm in females. In the neck extension position, the mean cricoid cartilage level was lower by 4.8 mm in males and higher by 14.4 mm in females than the lowest point of the transverse process of C6. The mean difference in the shortest distance from the horizontal line at the surface of the cricoid cartilage to the lowest point of the transverse process of C6 between neutral position and neck extension position was 18.3 mm in males and 19.6 mm in females. There was a statistically significant difference in the shortest distance from the horizontal line at the surface of the cricoid cartilage to the lowest point of the transverse process of C6 between neutral position and neck extension position in both males and females (Table 2). In addition, the difference in the shortest distance from the horizontal line at the surface of the cricoid cartilage to the lowest point of the transverse process of C6 between males and females was statistically significant in both neutral position and neck extension position (Table 2).
Go to : 
In our study, we showed that there was a statistically significant difference in the shortest distance from the horizontal line at the surface of the cricoid cartilage to the lowest point of the transverse process of C6 between neutral position and neck extension position in both males and females. We can observe cephalad movement of the cricoid cartilage level in neck extension position. In addition, the difference in position of the cricoid cartilage between males and females was statistically significant in both neutral position and neck extension position.
The target of injection for stellate ganglion block is the anterior tubercle of the C6 transverse process, and the cricoid cartilage is known as the landmark of the level of the C6 vertebra in supine neutral position. Therefore, if we use the cricoid cartilage as a landmark in stellate ganglion block, we should consider that the cricoid cartilage level is changed in neck extension position. Our results showed that the cervical vertebra which is palpated at the level of the cricoid cartilage might not be the transverse process of C6 in neck extension position for stellate ganglion block, because the difference in the shortest distance from the cricoid cartilage to the lowest point of the transverse process of C6 between neutral position and neck extension position was nearly 20 mm in both males and females. In particular, the position of cricoid cartilage in females was statistically higher than that in males, and the cricoid cartilage level in females was 14.4 mm higher than the transverse process of C6 in neck extension position. Therefore, it is highly possible that the cricoid cartilage level in females marks the C5 vertebra in neck extension position. Another interesting question is whether the cricoid cartilage is in fact the real landmark of the C6 vertebral level in neutral position. In our study, the cricoid cartilage level in males was lower by 23.3 mm than the transverse process of C6 in neutral position. This finding shows that the cricoid cartilage may not mark the C6 vertebral level in males.
Janik et al. [7] examined computed tomography (CT) images of the cervical spine of 70 adult patients to measure the distances between various points on the cricoid cartilage, anterior tubercle, posterior tubercle, and nadir of the vertebral gutter. Their study showed large variability in the size and location of the landmarks used for needle placement during stellate ganglion block. Due to this variability, it is difficult to find the precise C6 level, and that may help explain the significant failure rate of stellate ganglion block. In addition, most clinicians determine the injection point merely by palpating the transverse process of C6, and this landmark is not trustable in supine neck extension position for stellate ganglion block. Cha et al. [8] have examined the use of the neck crease landmark in identifying the level of C6 in obese patients. Their study was performed in standard position for stellate ganglion block, and found that in about 30% of cases, the cervical transverse process which was palpated by investigators was not the real C6 transverse process. Their results are consistent with our results, and these findings may explain one of the reasons why block failure has been reported in as many as 30% of patients.
As a possible method to lower the failure rate, some articles have discussed ultrasound-guided stellate ganglion block [9]. This method is especially useful in obese patients, because it is difficult to palpate cervical vertebral tubercles or transverse processes in obese patients. Ultrasound-guided stellate ganglion block shows benefits not only in lowering the failure rate but also in reducing the dose of local anesthetic [10]. However, the conventional technique remains popular as it does not require the preparation of ultrasound equipment.
There are some limitations in our study. First, we analyzed the relationship between neck extension and cricoid cartilage movement using x-rays which were taken in erect position. That is not a precise comparison, because stellate ganglion block is performed in supine position, not erect position. Second, the degree of neck extension during cervical lateral x-ray view might be not identical to the degree of neck extension during stellate ganglion block. Therefore, the estimation of cricoid cartilage movement in standard position for stellate ganglion block on the basis of cervical lateral x-ray view is not an accurate analysis. Third, our results cannot be applied to other races, because our entire study population was Asian (Korean). We think, therefore, that further multi-racial studies are needed. Fourth, our study had no age limitation. We believe that cricoid cartilage movement in neck extension may have age-related differences, so a study about age-related cricoid cartilage movement may be meaningful. Another limitation of our study is that we did not consider the position change of the stellate ganglion in neck extension. We did not evaluate whether the stellate ganglion also has cephalad movement in neck extension position. If the position of the stellate ganglion is changed according to neck extension, it may be another important factor in a successful block. If the stellate ganglion has cephalad movement in neck extension, we can expect a more successful block, because the stellate ganglion will be closer to the injection point.
In conclusion, we determined that the position of the transverse process of C6 is not identical to the level of the cricoid cartilage in neck extension position. However, we think that the difference in the shortest distance between these two points will be reduced in the standard position for stellate ganglion block, because the patient's neck is not fully extended in that position. The cricoid cartilage has been the easy, simple landmark of the transverse process of C6, but as we have shown, the cricoid cartilage as a landmark is less useful in neck extension position. However, if we recognize that the cricoid cartilage has cephalad movement in neck extension, the cricoid cartilage can be still useful as a landmark for stellate ganglion block. Further prospective studies are needed to find the best landmark for the real C6 transverse process for stellate ganglion block.
Go to : 
References
1. Park CG, Kim JS, Lee WH. The effect of stellate ganglion block for controlling postoperative pain after the shoulder joint surgery. Korean J Pain. 2006; 19:197–201.

2. Al-Abdullatief M, Wahood A, Al-Shirawi N, Arabi Y, Wahba M, Al-Jumah M, et al. Awake anaesthesia for major thoracic surgical procedures: an observational study. Eur J Cardiothorac Surg. 2007; 32:346–350. PMID: 17580117.

3. Garneau SY, Deschamps A, Couture P, Levesque S, Babin D, Lambert J, et al. Preliminary experience in the use of preoperative echo-guided left stellate ganglion block in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2011; 25:78–84. PMID: 20580574.

4. Raj PP. Pain medicine: a comprehensive review. 1996. St. Louis, MO: Mosby;p. 228–235.
5. Agur AMR. Grant's atlas of anatomy. 1991. 9th ed. Baltimore, MD: Williams & Wilkins;p. 551.
7. Janik JE, Hoeft MA, Ajar AH, Alsofrom GF, Borrello MT, Rathmell JP. Variable osteology of the sixth cervical vertebra in relation to stellate ganglion block. Reg Anesth Pain Med. 2008; 33:102–108. PMID: 18299089.

8. Cha YD, Lee SK, Kim TJ, Han TH. The neck crease as a landmark of Chassaignac's tubercle in stellate ganglion block: anatomical and radiological evaluation. Acta Anaesthesiol Scand. 2002; 46:100–102. PMID: 11903081.

9. Kapral S, Krafft P, Gosch M, Fleischmann D, Weinstabl C. Ultrasound imaging for stellate ganglion block: direct visualization of puncture site and local anesthetic spread. A pilot study. Reg Anesth. 1995; 20:323–328. PMID: 7577781.
10. Jung G, Kim BS, Shin KB, Park KB, Kim SY, Song SO. The optimal volume of 0.2% ropivacaine required for an ultrasound-guided stellate ganglion block. Korean J Anesthesiol. 2011; 60:179–184. PMID: 21490819.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download