Abstract
Hiccups have more than 100 etiologies. The most common etiology has gastrointestinal origins, related mainly to gastric distention and gastroesophageal reflux disease. Intractable hiccups are rare but may present as a severe symptom of various diseases. Hiccups are mostly treated with non-invasive or pharmacological therapies. If these therapies fail, invasive methods should be used. Here, we present a patient on whom we performed a blockage of the phrenic nerve with the guidance of a nerve stimulator. The patient also had pneumothorax as a complication. Three hours after intervention, a tube thoracostomy was performed. One week later, the patient was cured and discharged from the hospital. In conclusion, a stimulator provides the benefit of localizing the phrenic nerve, which leads to diaphragmatic contractions. Patients with thin necks have more risk of pneumothorax during phrenic nerve location.
A hiccup is defined as an involuntary, rhythmic and spasmodic contraction of the diaphragm [1]. When a person suddenly inhales, a hiccup occurs causing an involuntary closure of the glottis with a characteristic sound [1]. Dehydratation, sleep disturbance, depression, gastrointestinal diseases, and even death of a relative may be predisposing factors for hiccups [2,3]. Hiccups usually subside within 48 hours. However, if they continue for more than 48 hours and up to 1 month, they are called "persistent" hiccups. If they continue more than 1 month, it is called intractable hiccups [1,4]. Traditionally, hiccups are treated via non-invasive pharmacological methods. In some rare cases, invasive interventions are performed. Nerve blocks may be considered only for intractable hiccups.
We present a case in which a nerve blockage was performed on a patient suffering from intractable hiccups who had not responded to pharmacological therapy.
A 78-year-old male patient was hospitalized in the General Surgery Clinic with diagnosis of gastroesophageal reflux disease (GERD) and intractable hiccup. His medical treatment was sodium alginate liquid 100 mg/day, pantoprazol 40 mg/day, chlorpromazine 200 mg/day, and ursodeoxycolic acid 10 mg/kg/day. He had a history of a nissen fundoplication operation 3 years previous and, after myocardial infarction, a coronary artery bypass grafting operation 5 years previous. He had intermittent hiccups several times, but all his hiccups ceased without any treatment. However, this last hiccup attack was intractable and persisted for more than one month. First, chlorpromazine (200 mg/day) was given for the hiccups as pharmacological therapy, but no benefit was observed. The 45 days of pharmacological therapy also included other drugs, such as baclofen (15-25 mg/day), gabapentin (300-1,200 mg/day). In spite of these treatments, his condition deteriorated and the frequency of the hiccups gradually increased. Finally, nutritional and oral feeding issues were noted. His quality of life was significantly affected with aggravating psychological and physical problems. Therefore, a phrenic nerve block was planned. Informed consent was acquired before intervention.
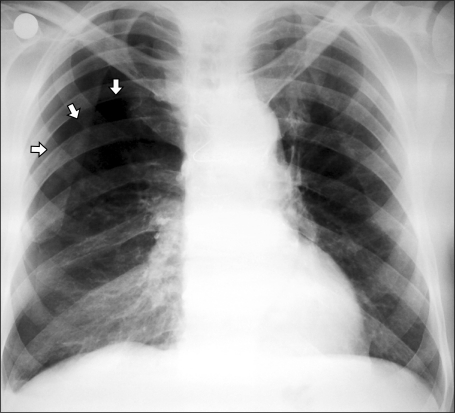
In the operating room, the right phrenic nerve was blocked under sterile conditions. A nerve stimulator (Stimuplex HNS11, B. Braun Medical Germany) was used with a 50 mm 21 G isolated needle (Stimuplex; B. Braun, Melsungen, Germany). The needle was inserted between the sternocleidomastoid muscle and the anterior scalenius muscle. Electrical current (1,5 mA; 2-Hz) was applied. After multiple trials, synchronized diaphragmatic movements were observed, which indicated that the phrenic nerve was found. Next, 25 mg 0.5% of bupivacaine and 40 mg of triamsinolone were injected slowly in 15 ml volume. No immediate complication was observed and the patient was transferred to the wards. Hiccup frequency subsided and ceased completely after 3 hours. However, pneumothorax was detected on his control chest x-ray (Fig. 1). A tube thoracostomy was performed. At the 7th day, the tube was removed and the patient was discharged. During 6 months of follow-up, no medical treatment for hiccups was given. Only one temporary hiccup period (self-limited, less than 24 hours) was reported during the follow-up.
Hiccups have more than 100 etiologies [2-5]. The most common etiology is gastrointestinal. The GI disorders are mainly gastric distention and GERD [2,6]. Esophageal disorders are also associated with hiccups. These include benign stricture, hiatal hernia, pill esophagitis, esophageal reflux, and infectious esophagitis [2]. In this case study, the hiccups were associated with esophagitis and GERD. Also, metabolic derangements and drugs may also predispose to hiccup [4,7].
In the treatment of hiccups, the etiology of the predisposing disease should first be thoroughly evaluated. Therapy plans can then be made. Therapy usually has 3 steps; non-pharmacological, pharmacological, and nerve blocks. The first step involves non- pharmacological inhibition of the afferent pathway of the vagus nerve. This includes, holding breathe, drinking cold water, compressing the eye ball, inhaling carbon dioxide, inserting a nasogastric catheter, and gastric lavage [5,8]. If these methods fail to stop the hiccups, pharmacological methods are attempted. This can include the use of metoclopramide, chlorpromazine, amitriptyline, phenytoin, and valproic acid [4,9]. Recently, baclofen and gabapentin have been introduced for both monotherapy and combined therapy [1,4,5,9]. In a case-report by Turkyilmaz and Eroglu [10], a patient with a tumor on the esophagogastric intersection had hiccups after stent placement. They reported successful treatment of the hiccups with baclofen. Ong et al. [1] reported successful treatment of intractable hiccups in a peritoneal dialysis patient. Lierz and Felleiter [9] reported treatment of hiccups which did not respond to pharmacological therapy. They used neuromuscular blockers under general anesthesia with a facemask. Gilson and Busalacchi [11] showed the therapeutic efficacy of marijuana in the treatment of intractable hiccups. Several reports exist of nerve blocks achieving successful outcomes in treating hiccups [7,12].
Nerve stimulators are used to find the exact location of the phrenic nerve which is responsible for the diaphragmatic contractions in hiccups. Nerve stimulators are useful in finding the phrenic nerve in patients whose sternocleidomastoid muscle cannot be defined. Stimulation with 1 or 2 Hz can easily discriminate contractions due to hiccup or stimulator. Stimulators may still not be able to differentiate high frequency hiccups [8]. Only nerve stimulation itself is reported to be effective in hiccup treatment [13].
Our patient had a positive response to pharmacological therapy for his intermittent hiccups. However, his last hiccup attack did not respond to pharmacological therapy. Chlorpromazine (200-300 mg/day), baclofen (15-25 mg/day), and gabapentin (900-1,800 mg/day) all failed to treat his hiccups. Intractable hiccups can disturb daily life activities. Hospitalization may be indicated. Physical or psychological problems may also arise [2,9]. Our patient lost weight (9 kg) and suffered similar problems.
After multiple attempts to use the nerve stimulator, pleural damage occurred. Our patient was slim and had an asthenic structure, a thin neck, and a cough. These factors may have contributed to the pleural damage that occurred during intervention. This risk increases in repeated blocks. Therefore, ultrasound has recently been used to guide nerve blocks. Ultrasound can detect anatomic structures like nerves, muscles, and blood vessels. The possibility of complications decreases and a phrenic nerve block may be more easily facilitated [3,7,14].
In conclusion, considering the predisposing factors and repeated (multiple) try outs, the use of intervention methods requires accuracy and care. This case report presents the possibility of the occurrence of pneumothorax during phrenic nerve block using a stimulator. Further studies are needed to confirm the safety and efficacy of intervention therapy for hiccups.
References
1. Ong AM, Tan CS, Foo MW, Kee TY. Gabapentin for intractable hiccups in a patient undergoing peritoneal dialysis. Perit Dial Int. 2008; 28:667–668. PMID: 18981399.

2. Schreiber LR, Bowen MR, Mino FA, Craig TJ. Hiccups due to gastroesophageal reflux. South Med J. 1995; 88:217–219. PMID: 7839166.

3. Kang KN, Park IK, Suh JH, Leem JG, Shin JW. Ultrasound-guided pulsed radiofrequency lesioning of the phrenic nerve in a patient with intractable hiccup. Korean J Pain. 2010; 23:198–201. PMID: 20830266.

4. McAllister RK, McDavid AJ, Meyer TA, Bittenbinder TM. Recurrent persistent hiccups after epidural steroid injection and analgesia with bupivacaine. Anesth Analg. 2005; 100:1834–1836. PMID: 15920222.

5. Petroianu G. Idiopathic chronic hiccup (ICH): phrenic nerve block is not the way to go. Anesthesiology. 1998; 89:1284–1285. PMID: 9822029.
6. Pooran N, Lee D, Sideridis K. Protracted hiccups due to severe erosive esophagitis: a case series. J Clin Gastroenterol. 2006; 40:183–185. PMID: 16633116.
7. Calvo E, Fernández-La Torre F, Brugarolas A. Cervical phrenic nerve block for intractable hiccups in cancer patients. J Natl Cancer Inst. 2002; 94:1175–1176. PMID: 12165648.

8. Okuda Y, Kitajima T, Asai T. Use of a nerve stimulator for phrenic nerve block in treatment of hiccups. Anesthesiology. 1998; 88:525–527. PMID: 9477074.

9. Lierz P, Felleiter P. Anesthesia as therapy for persistent hiccups. Anesth Analg. 2002; 95:494–495. PMID: 12145080.

10. Turkyilmaz A, Eroglu A. Use of baclofen in the treatment of esophageal stent-related hiccups. Ann Thorac Surg. 2008; 85:328–330. PMID: 18154840.

11. Gilson I, Busalacchi M. Marijuana for intractable hiccups. Lancet. 1998; 351:267. PMID: 9457104.

12. Babacan A, Oztürk E, Kaya K. Relief of chronic refractory hiccups with glossopharyngeal nerve block. Anesth Analg. 1998; 87:980. PMID: 9768811.

13. Okuda Y, Kitajima T, Asai T. Use of a nerve stimulator for phrenic nerve block in treatment of hiccups. Anesthesiology. 1998; 88:525–527. PMID: 9477074.

14. Okuda Y, Kamishima K, Arai T, Asai T. Combined use of ultrasound and nerve stimulation for phrenic nerve block. Can J Anaesth. 2008; 55:195–196. PMID: 18310638.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download